Ependymoma is a brain tumor that develops when the cells lining the surface of the brain ventricles mutate. Refers to the primary formations of the central nervous system; it can have a benign or malignant course. Most often localized in the posterior cranial fossa or the region of the lateral ventricles, it grows slowly, but is capable of penetrating into adjacent brain structures. Brain ependymoma is dangerous because it can go unnoticed for a long time, and the first signs of the disease appear when the tumor has reached a large size or has metastasized. The main approach to treating a tumor is an integrated approach, which consists of resection of the tumor followed by chemotherapy and radiation therapy. Why does pathology develop, what are its symptoms and what treatment gives a positive prognosis?
Causes of brain ependymoma
What serves as a prerequisite for the development of a tumor is unknown, but still there are several factors that can influence the development of pathology:
- heredity;
- long-term use of potent drugs;
- ionizing radiation;
- trauma to the skull or central nervous system;
- oncogenic viral diseases (human papillomavirus, herpes);
- poor environmental conditions;
- smoking and alcohol abuse.
The cancer trigger was initially thought to be the SV40 virus, which was discovered in ependymoma cells. However, subsequent studies did not confirm this theory, so the etymology of the disease is still unknown. As practice shows, cerebral ependymoma most often occurs in children and adolescents, less often in adults.
Symptoms
Unlike other types of brain tumors, ependymoma is rare. Cancer cells can have different levels of malignancy. Some tumors grow slowly, while others grow quickly, compressing surrounding vessels and tissues, causing characteristic symptoms.
Clinical signs of ependymoma directly depend on the location and size of the formation. As with other types of cancer, in the early stages it does not cause obvious symptoms and only as the tumor grows do the symptoms become more noticeable and, in some cases, severe.
The main signs of the disease are blurred vision and hearing, convulsions, difficulty swallowing and speech impairment, which are manifested as a result of increased intracranial pressure. Other characteristic symptoms include:
- headache of a bursting or aching nature;
- dizziness;
- impaired coordination of movements;
- unsteady gait;
- tremor of the limbs;
- chronic fatigue;
- a sharp decrease in body weight;
- nausea, urge to vomit;
- memory loss;
- sudden change of mood;
- “floaters” or “fog” before the eyes;
- convulsions, numbness of extremities;
- difficulty swallowing.
Symptoms depend on where the formation is located. If the tumor is located in the cerebellum, balance and gait will be affected. Its location in the cerebrum causes seizures. The presence of a formation in the spinal cord - numbness of the face, disturbances in the functioning of the digestive system. The exact location of cancer can only be recognized with the help of comprehensive diagnostics, which is prescribed by a doctor if an oncological process is suspected.
Types of ependymoma
In oncology, ependymomas are divided into 4 main stages, which differ in the level of benignity and developmental features:
- Myxopapillary (papillary) is a benign tumor that is localized in the conus of the spinal cord and is characterized by slow growth. With timely treatment, it has a good prognosis. Refers to the first stage of malignancy, since there is a risk of its degeneration.
- Subependymoma - develops from subependymal glia. Externally it has the shape of a node and is located in the ventricular system of the brain. As in the first case, it develops slowly and has a good prognosis.
- Classic ependymoma is the most common type of tumor, which is localized in the ventricles of the brain. It often relapses and can degenerate into malignant cancer. It has 2 degrees of malignancy.
- Anaplastic ependymoma is a severe form of cancer with a poor prognosis. Characterized by rapid growth and metastases. Refers to stage 3 oncology.
The last 2 stages of the disease are considered the most dangerous, since even with surgery and therapy they are capable of relapses and metastases. According to the localization of the tumor process, it is divided into:
- supratentorial - the location of the tumor is diagnosed above the cerebellar tentorium. Such ependymomas are formed outside the ventricles of the cerebral hemispheres, have a nodular shape, a bumpy or smooth surface, and can fill all the cavities of the ventricles.
- infratentorial - located in the posterior cranial fossa, often affecting the brain stem and fourth ventricle.
Cancerous tumors in brain structures, regardless of location, should be diagnosed in a timely manner, this increases the chances of a positive prognosis from treatment.
Ependymomas grow slowly compared to other cancers, but they are capable of displacing tissue in the brain or spinal cord, but not growing into them. Such cancer cells rarely metastasize beyond the central nervous system. In the case of grade 3 malignancy and surgery is performed, a new focus of formation appears at the local level (close to the original process).
EPENDYMOMA
EPENDYMOMA
(
ependymoma
) is a neuroectodermal tumor that develops from ependymocytes lining the ventricles of the brain and the spinal canal.
According to L.I. Smirnov (1962), ependymomas make up about 3% of all tumors of the central nervous system (see Brain, tumors). Ependymoma is observed mainly in young people (the average age of patients is 22 years).
Rice. 1. Gross specimen of the brain (frontal section) for intraventricular ependymoma of the third ventricle: the arrows indicate the tumor in the form of a clearly demarcated node filling the lumen of the third ventricle of the brain.
Brain ependymomas are more often located intraventricularly; paraventricular localization of these tumors is less common. Spinal cord ependymomas arising from the ependyma of the central canal are located intramedullary, and those developing from the ependyma of the terminal ventricle or filum terminale are extramedullary. Macroscopically, ependymoma most often has the appearance of a clearly demarcated node (Fig. 1), in which large smooth-walled cysts can be identified on the section. Intramedullary ependymoma often takes the form of a pin or spindle. In the area of initial tumor growth, as a rule, there are no clear boundaries with the brain tissue.
Rice. 2. Microscopic specimen of brain ependymoma (the main histological type is ependymoma itself): arrows indicate characteristic perivascular structures - “pseudorosettes”; hematoxylin-eosin staining; x 400.
In accordance with the International Histological Classification of Tumors of the Central Nervous System (1979), four types of ependymoma are distinguished. The main histological type is ependymoma itself, which is characterized by the presence of perivascular and true “rosettes”. Perivascular “rosettes” (“pseudorosettes”, “corona radiata”) are formed by tumor cells located around blood vessels (Fig. 2). In true rosettes, tumor cells are located around channels lined by ependymal epithelium. Less common is papillary ependymoma, consisting of villi and trabeculae covered with ependymal epithelium. This type of tumor most often has an extramedullary localization (ependymoma of the cauda equina). During histological examination in cases of papillary ependymoma, a differential diagnosis must be made with choroidpapilloma (see). Myxopapillary ependymoma is also localized extramedullary, most often in the cauda equina region, and is characterized by mucous degeneration (see) and edematous melting of tissue with the formation of mucous cysts. Subependymoma (subependymal nodular astrocytoma, ependymoastrocytoma, ependymoglioma) develops from subependymal glia and consists of islands of monomorphic ependymal cells lying in a dense stroma of glial acellular fibers. Most often, subependymoma has the shape of a node and is located intraventricularly.
In addition to these histological types, a malignant variant of ependymoma is distinguished (anaplastic ependymoma, ependymoblastoma), characterized by typical morphological signs of anaplasia. With this type of ependymoma, metastases can spread throughout the subarachnoid space. Bailey (P. Bailey), X. Cushing (1926), L. I. Smirnov (1962), B. S. Khominsky (1969) also identify a very rare variant of the tumor - epithelial ependymoma (ependymoeshgthelioma, or neuroepithelioma of the brain), consisting of epithelial-like cells.
Clinical picture
ependymomas are determined by the location of the tumor. In intraventricular ependymoma with occlusion of the cerebrospinal fluid pathways, most often the first and main sign of the disease is hypertensive-hydrocephalic syndrome, which is characterized by headaches accompanied by vomiting, swelling of the optic discs, secondary hypertensive changes on the craniogram (see Hypertensive syndrome). With ependymoma of the lateral ventricle, symptoms of intracranial hypertension may be accompanied by moderately pronounced signs of focal damage to the corresponding cerebral hemisphere. For ependymoma of the third or fourth ventricles, along with hypertensive-hydrocephalic syndrome, more distinct local (focal) symptoms are typical. With a tumor of the third ventricle, hormonal disorders are observed (obesity or cachexia, diabetes insipidus, sexual disorders); with a tumor of the fourth ventricle - symptoms of irritation of the formations that form it - fixed position of the head, paroxysmal headaches, vomiting not associated with headache, cerebellar disorders, symptoms of nuclear or radicular damage to the cranial nerves, Bruns attacks (severe dizziness, changes in pulse rate, breathing, collaitoid state).
Intramedullary ependymoma causes a pattern of gradually developing transverse lesions of the spinal cord. Cauda equina ependymoma is characterized by radicular pain, dysfunction of the pelvic organs, muscle atrophy, paresis, sensory disturbances, and loss of tendon reflexes in the lower extremities.
Diagnostics
ependymoma of the brain is based mainly on data from visualization methods of the ventricles of the brain - computed tomography (see Computed tomography), ventriculography (see), pneumoencephalography (see). Diagnosis of ependymoma of the spinal cord is based on the general principles of diagnosing all tumors of the spinal cord - spinal puncture (see) with liquorodynamic tests (see) and determination of the protein content in the cerebrospinal fluid (see), ascending and (or) descending myelography (see) .
Treatment
ependymomas surgically, in some cases followed by external beam radiation therapy (see), which is most indicated for the malignant version of the tumor. As a rule, ependymoma can be removed radically, but with tumors arising from the walls of the third ventricle, the bottom of the fourth ventricle, with long intramedullary ependymomas and ependymoma of the cauda equina, which grows on the roots of the lumbar nerves forming the cauda equina, the operation is associated with significant difficulties. In these cases, the use of microsurgical techniques is required (see Microsurgery).
Forecast
relatively favorable and is determined by the location of the tumor and the radicality of the operation. The prognosis for anaplastic ependymoma is less favorable.
See also Brain, tumors; Spinal cord, tumors.
Bibliography:
Badmaev K. N. and Smirnov R. V. Radionuclide diagnostics and radiation therapy of diseases of the nervous system, M., 1982; Razdolsky I. Ya. Clinic of brain tumors, L., 1957; aka, Tumors of the spinal cord and spine, L., 1958; Smirnov L.I. Tumors of the brain and spinal cord. M., 1902; Khominsky B. S. Histological diagnosis of tumors of the central nervous system, M., 1969; Brain tumors, ed. by DGT Thomas a. DIG ra li am, L. - B about s to n, 1980; Ziilch K. J. Die Hirn-gesclnvulste in biologischer und morpliolo-gischer Darstellung, Lpz., 1958; o n e, Atlas of the histology of brain tumors, V. ao, 1971; o n e, Histological typing of tumors of the central nervous system, Geneva, 1979.
T. M. Wichert, B. A. Kadashev.
Diagnostics
To diagnose brain ependymoma, you need to consult a neurologist. The specialist will examine the medical history in detail and prescribe a number of tests and studies:
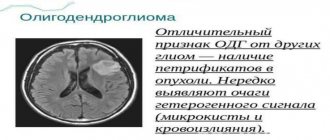
- MRI is an informative examination method that allows you to accurately determine the size and location of the tumor, its structure, and shape.
- CT scan – determines the focus of the disease, reveals whether there are metastases to other organs and systems.
- Electroencephalography – examines the functioning of the blood vessels in the brain.
- Ophthalmoscopy - the procedure consists of examining the fundus, assessing the optic nerve and retina.
- Angiography is performed using contrast to assess the condition of the blood vessels in the brain.
- A biopsy is a procedure that allows you to determine the type of tumor. During the process, tumor tissue is collected and then tested in the laboratory.
The examination results allow the doctor to obtain a complete picture of the disease. If necessary, the doctor prescribes a consultation with doctors from other areas of medicine: ophthalmologist, otolaryngologist, psychologist. Comprehensive diagnostics is the basis for making a final diagnosis and determining further treatment tactics.
Treatment of brain ependymoma
Modern oncology and neurosurgery has the latest equipment for the diagnosis and treatment of brain tumors. Research Institute of Neurosurgery named after. Burdenko is one of the few where complex operations to remove ependymoma are performed. The clinic employs a team of high-level doctors who, over several years, have performed many complex operations to remove tumors from brain structures. The oncology center is equipped with modern equipment for diagnosis and treatment. An integrated approach and an affordable price allow us to consider the Burdenko Clinic one of the best in Moscow.
To get a full consultation and detailed information about treatment at the Burdenko Clinic, you can go to the website of the neurological center, where all the necessary information for patients is provided. The cost of treatment at the oncology center is calculated individually for each patient. If a person is unable to pay for treatment, the clinic has a quota for free treatment.
Considering that brain ependymoma has a high degree of malignancy, therapy is most often complex, consisting of surgery and radiation therapy. Chemotherapy treatment is carried out only if surgery is not possible. This treatment of ependymoma does not give a good prognosis; it can only prolong the patient’s life by several months.
I consider surgery to be the optimal method for treating such a tumor. It is performed using microscopic technology, which allows intervention into brain structures with minimal risk to health and the highest accuracy. During the operation, there is often a need for craniotomy. This allows access to the tumor and its complete or partial excision. Removing brain ependymoma does not provide a 100% guarantee for the complete destruction of cancer cells, so surgery is often combined with radiation therapy. The procedure has a detrimental effect on cancer cells that could not be eliminated by surgery.
Stereotactic radiosurgery, which involves exposing tumor tissue to radioactive rays, is often used to destroy tumor cells. Thanks to this technique, it is possible to stop tumor progression and destroy cancerous tissue, without affecting the healthy membranes of the brain.
Treatment of ependymoma in the clinic takes a long time, since the patient, even after the operation, must be under medical supervision. After therapy, the patient requires rehabilitation, which includes diet therapy, consultation with a speech therapist, psychologist, and therapeutic exercises. The recovery period may take several months.
Considering the complexity of the operation and intervention in the structures of the brain and central nervous system, there are always risks of postoperative complications. They can manifest themselves in the form of neurological disorders - seizures, loss of memory, vision and hearing. Sometimes patients learn to speak, read and write again. They require constant care and examinations. Medical supervision after surgery allows you to monitor the dynamics of the disease, the appearance or absence of relapses. In case of complications, the patient is prescribed special restorative therapy to eliminate symptoms and improve the patient’s quality of life.
Any tumor in the brain, regardless of whether it is malignant or benign, requires immediate treatment, since even a small tumor can have a negative impact on the functioning of the body and a person’s well-being.
Treatment of ependymoma
The only effective treatment for ependymoma is radical removal of the tumor. Surgical treatment is performed by a neurosurgeon using microsurgical technologies. During the entire manipulation, motor and sensory potentials are monitored.
During the operation, the benign formation is easily separated from the surrounding tissue and completely removed. For a malignant tumor, extended resection of neoplasia is performed. In the postoperative period, a control MRI is performed. If the slightest part of the tumor is not removed, repeat surgery is recommended.
Radiation therapy is carried out when the malignant nature of the ependymoma is confirmed. In the future, a course of rehabilitation with massage and exercise therapy is required. Drug treatment involves the prescription of anti-inflammatory, vascular, and neurometabolic drugs.
Prognosis after surgery
Life after treatment for ependymoma largely depends on the stage of the disease. If the disease is diagnosed in time and treated appropriately, the survival rate for more than 5 years is 70%. A less favorable prognosis is present with an anaplastic tumor, which can grow rapidly and metastasize. In this case, the chances of life are not great, and the treatment provided will prolong life by 1 - 2 years. If surgery is not possible, supportive care may increase life expectancy by just a few months.
If the operation fails to completely remove the tumor, there is always a risk of its recurrence. In such cases, the prognosis worsens, and the risk of its metastases to other organs and systems increases significantly. Unfortunately, there are no preventive measures that can protect against brain cancer. However, if you follow some rules, you can reduce tumor formation:
- proper and healthy nutrition;
- rejection of bad habits;
- eliminate the effects of radiation on the body;
- undergo regular medical examinations;
- monitor the state of the immune system.
By following basic rules, you can significantly reduce the risk of any cancer. Ependymoma is a type of brain cancer that requires timely diagnosis and quality treatment. By treating this pathology in the early stages of the disease, the chance of a positive prognosis is quite good, and the patient himself has the opportunity to return to a full life.
Reviews of doctors providing the service - Back and spine injuries
In 2000, Andrei Arkadyevich performed spinal surgery on me.
Four days in the clinic and I have been living a full life for 20 years without restrictions on movement and I remember with gratitude Dr. A.A. Khodnevich. God bless him. And in 2000 he could walk no more than 10 meters. Read full review Viktor Alexandrovich
20.05.2020
Low bow to Alexander Semenovich Bronstein and Andrei Arkadyevich Khodnevich. I arrived at CELT on July 2, 2021 with extreme pain that I endured for 10 days. Hernia C6-C-7. I was given two blockades in Ivanovo, about 9 complex IVs, I lost 6 kg in a week and was in a panic, I didn’t see a way out and nothing happened to me... Read full review
Elena Nikolaevna L.
20.10.2019