Find out more about diseases starting with the letter “O”: Fainting (syncope); Occlusive hydrocephalus; Occlusion of the carotid arteries; Olivopontocerebellar degenerations; Optico-chiasmatic arachnoiditis; Neuromyelitis optica; Brain tumors; Cerebellar tumors; Tumors of peripheral nerves; Spinal cord tumors; Brain stem tumors; Central nervous system tumors; Tumor of the cauda equina; Tumor of the pineal gland; Oromandibular dystonia; Osteocondritis of the spine; Brain swelling; Carbon monoxide poisoning; Ophthalmoplegic migraine.
Brainstem tumors are pathological formations of the middle, medulla oblongata and pons of the brain. Symptoms are very diverse: hearing impairment, strabismus, nystagmus, sore throat, facial asymmetry, impaired coordination of movements, changes in gait, single upper or lower paresis, multiple paresis, liquor-hypertensive syndrome.
MRI of the brain is a unique way to accurately diagnose tumor formations. Surgical treatment is acceptable in 20% of clinical cases of the disease. Radiotherapy and chemotherapy are acceptable for other patients. Most of the patients die in the first year of manifestation of the disease - the prognosis is extremely unfavorable.
Total information
Pathological formations of the trunk are detected in children under the age of 15 years - up to 70% of operated patients. Most of the patients are children 5-6 years old. Of the total number of brain tumors, stem tumors make up 10-15%. Of this amount, 90% are brain gliomas. The high level of morbidity in childhood, the difficulty of diagnosis, the complexity of treatment and the high mortality rate make stem tumors a vital problem in oncology, neurology, pediatrics and neurosurgery.
Pathogenesis and morphology of the disease
The multiple functions of the brainstem provide connections between the activities of the central nervous system and the peripheral nervous system. The interaction of the two departments guarantees the vital functions of the body - motor functions, breathing processes and cardiac activity, vascular tone. The nerve pathways run from the cerebellum, cortex, and medulla through the trunk to the spinal cord. The nuclei of the III-XII pairs of cranial nerves are localized in the trunk. The centers of breathing and cardiovascular function are located in the brain stem and make it a vital element of the body.
The complexity of the structure of the trunk, the presence of conductive and nuclear systems provide a variety of clinical symptoms. In a differential way, it is necessary to exclude cerebellar neoplasms. Tumor-like lesions of the brainstem do not cause liquorodynamic disturbances that cause hydrocephalus. A tumor in the area of the Sylvian aqueduct can cause similar clinical manifestations.
Most of the tumors are benign in structure and are astrocytoma with diffuse distribution. Malignant astrocytomas account for 15-30% of all brain stem tumors. Hemangioblastoma, epindymoma, modloblastoma, ganglioglioma, astroblastoma, and metastatic melanoma are diagnosed much less frequently.
Types of tumors
There are two types of tumors: primary and secondary. Disruptions in brain activity caused by harmful factors will ultimately lead to the chaotic division of damaged cells until they are completely replaced by healthy ones. This is how a primary tumor of the brain stem appears in children and older people. It is based on glial cells. Brain stem cancer can start and develop in one part of the organ. A common place for oncology to appear is the bridge (about 60%). Slightly less - in the midbrain and medulla oblongata. Brain stem tumors occur in the plural.
Secondary are those that appear in one place and continue to grow on the brain stem. Moreover, in only 5% of cases, metastases occur in the trunk, penetrating from other organs. A brain stem tumor is a parastem formation (para – about).
Common types of tumors are gliomas, which develop from glial cells.
- Astrocytomas account for about 60% of diseases. There are multiforme, pilocytic, anaplastic and fibrillary. Benign ones include pilocytic and fibrillary. Pilocytic forms occur in children. Glioblastoma (multiforme) is considered aggressive, which occurs most often in men under 50 years of age.
- Ependymomas account for 5% of all tumors. Most often it is benign.
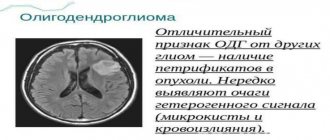
- Oligodendrogliomas occur in 8% of diseases. Large tumor sizes. There are 4 degrees of malignancy.
Classification
New growths of the trunk are divided according to their location. A primary stem neoplasm grows from the stem substance and can be intrastem or exophytic-stem. Auxiliary stem pathogenesis is formed in the membranes of the fourth ventricle and the substance of the cerebellum and spreads into the brain stem. Parastem tumors are classified into a separate group. They can deform the trunk or grow together with it.
The Institute of the Russian Academy of Medical Sciences has formulated a classification of stem tumors depending on the type of their growth. Neoplasms are divided into:
- nodular - grow very quickly, separated from brain tissue by a capsule represented by dense intertwined processes of tumor cells, often cystic in nature.
- diffuse - very common - up to 80% of cases of all tumors. The neoplasm cells spread in the medulla, so it is impossible to determine the boundaries of the formation using a macroscopic method. The substance of the brain stem undergoes decomposition, its partial damage and rupture are determined.
- infiltrative - the rarest type of neoplasm. It has well-defined boundaries, due to which it has the second definition of “pseudonodal tumor”. Macroscopic analysis reveals infiltrative tumor growth and destruction of nearby nerve tissue.
Classification of brain stem tumors
Stem tumors are classified as follows: • primary stem formations: exophytic stem and intrastem; • secondary stem formations: growing onto the brain stem through the bottom of the rhomboid fossa and growing onto it through the cerebellar peduncles; • parastem formations: deforming the brain stem and closely adjacent to it.
The first group includes those neoplasms that are formed from the tissue of the brain stem itself, the second - those formed from the cerebellum, the membranes of the fourth ventricle and growing into the brain stem. All groups have differences in the onset of the disease. In the first group, stem dysfunction is already present at the beginning of the disease, and in the second it is observed later. Stem structures are of great importance, which affects the severity of the disease and the difficulties of neurosurgical intervention.
Symptoms of the clinical picture of the disease
The nuclei of the cranial nerves, nerve pathways, centers - all components of the brain stem influence the development of many symptoms of its damage. The compensatory properties of children's nervous tissue provoke a long-term course of the disease in children. The occurrence of a tumor process affects the initial symptoms of the disease; further manifestations depend entirely on the type of tumor.
Probably, the development of main paresis of the facial nerve with a violation of facial symmetry, nystagmus, strabismus, as well as the occurrence of motor coordination disorders, unsteadiness of gait. Symptoms include dizziness, hand tremors, hearing loss, difficulty swallowing and a sore throat. Decreased muscle activity, paresis of the arms, legs or half of the body are added to the main symptoms. In a later period of the disease, symptoms of hydrocephalus appear - headache, nausea, vomiting. The death of the patient occurs due to disorders of cardiovascular functioning and the respiratory center of the brain stem.
Tumors of the medulla oblongata and pons
Treatment of cancer >> Books on oncology >> N. A. Popov, “Intracranial tumors” Len. dept. Medgiz Publishing House, Leningrad, 1961 OCR Wincancer.Ru Given with some abbreviations
Tumors of the medulla oblongata and pons are less common than other tumors of the posterior cranial fossa. Although their topical diagnosis usually does not present serious difficulties, at the onset of the disease it is possible to confuse them with other types of pathological processes, since tumors of this localization are rarely accompanied by a significant increase in intracranial pressure, and sometimes occur without cerebral symptoms. This is partly explained by the fact that patients often die before the conditions for intracranial hypertension are created.
A characteristic feature of tumors of this localization is the slowly increasing development of nuclear palsies of the cranial nerves (one or the other depending on the level of damage to the trunk) - in combination with cross conduction symptoms (pyramidal hemisyndrome and sensitivity disorders), i.e. alternating paralysis.
In contrast to their typical expression in vascular stem processes, in tumors of this type, paralysis is not so clearly defined, being, moreover, only a passing stage in the progressive development of the process. Soon they move to the other side or from the very beginning, to one degree or another, capture both halves of the trunk, which is more typical of tumors of the medulla oblongata.
Then the process may begin with damage to the nuclei of the cranial nerves (if the tumor grows dorsally), which is later joined by conduction disorders, or begin with the latter (if the tumor develops ventrally) with subsequent involvement of the cranial nerves. As a rule, the process ends with damage to the entire diameter at the level of maximum tumor development.
When the tumor is localized in the pons, the main symptom is damage to the trigeminal nerve with possible crossed hemihypesthesis or (with a more caudal localization) alternating paralysis of the facial nerve. A very striking symptom may be a violation of vestibular function in the form of sharp systematized dizziness due to damage to the nucleus of the vestibular nerve, which may make one suspect a tumor of the fourth ventricle, especially if there is also irritation of the vomiting center.
In cases of tumor growth within the medulla oblongata, severe bulbar disorders develop. There are often cerebellar symptoms due to the involvement of the cerebellar peduncles in the pathological process. They can be one of the early and clear signs of the disease, which often gives rise to an erroneous diagnosis of a tumor of the cerebellum or cerebellopontine angle. Due to the gliomas that often develop here and are relatively fast-flowing, it is possible that the tumor process may initially be mixed with others, such as inflammatory diseases (encephalitis), vascular diseases, multiple sclerosis, etc.
The difficulty of early and rapid recognition of brain stem tumors, as mentioned above, depends largely on the absence of cerebral symptoms, which are less common here than in other localizations, or appear late. However, T. M. Strelinskaya observed congestive nipples in half of her cases. If we take into account that tumors rarely develop in the brain stem, then at first, naturally, we have to think first of all about other diseases of the nervous system.
The prognosis of brain stem tumors is unfavorable, since surgical treatment is impossible: only radiotherapy can delay the steadily and usually rapidly progressing process.
Patient M., 10 years old, was admitted to the hospital on 17/X 1955 with complaints of headaches, sometimes with vomiting, a feeling of numbness in the right half of the body, and an unsteady gait. The pain began more than a year ago, but only recently became particularly intense. About two weeks ago, the patient began to notice that when turning her head to the left, a feeling of dizziness arose.
Objectively: Forced position of the head with a tilt to the right and slightly forward. The patient can only lie on the right side, otherwise severe dizziness occurs. The fundus, visual acuity and visual field were unchanged. Rotatory large-amplitude nystagmus, intensifying when looking up. Hypoesthesia of the left half of the face and scalp, the corneal reflex on the left is absent. VIII pair: auditory function without changes; caloric test: pronounced labyrinthine nystagmus, but no reactive miss. During the pointing test, the right hand spontaneously swings outwards.
The tongue deviates slightly to the right. Tendon reflexes are increased, on the legs they predominate on the right. Abdominal - not called. Decreased muscle tone in the right leg. Right-sided hemihypesthesia of skin sensitivity, with the exception of the face; deep sensitivity without changes. Performs coordination tests with uncertainty, adiedochokinesis in the right hand. The gait is unsteady with a deviation predominantly to the right and back; cannot stand on his right leg.
Craniogram without changes. Cerebrospinal fluid: protein - 0.033%o, cytosis - 0, ROE - 48 mm per hour. Clinical diagnosis: Tumor of the fourth ventricle arising from the upper half of the bottom of the rhomboid fossa. The patient was transferred to a neurosurgical clinic. Operation 30/XI 1955: Cloudy arachnoid adhesions in the area of the cistern magna were excised. Examination of the fourth ventricle revealed a tumor of the brain stem protruding from the bottom of the rhomboid fossa. A large amount of cerebrospinal fluid was released. Three weeks after the operation, horizontal gaze paresis to the left, paresis of the left facial nerve, right-sided hemiparesis and hemihypesthesia appeared. General cerebral symptoms and forced head position disappeared. Subsequently, tetraparesis, dysphagia, and dysarthria developed. On March 13, 1956, the patient died.
Section: Tumor of the pons (which is sharply changed and increased in size), protruding deeply into the greatly dilated IV ventricle, filling it almost completely. Histologically - glioblastoma multiforme.
In this observation, the tumor of the pons was taken to be a primary neoplasm of the fourth ventricle, which gave rise to surgical intervention. The most striking and important symptom in this case was the forced position of the head - a symptom so characteristic of intraventricular localization. Although this symptom was associated with attacks of severe dizziness in certain positions of the head, its dependence on disturbances in the circulation of cerebrospinal fluid, which occurs with neoplasms of the fourth ventricle, could not be excluded.
In a certain contradiction with this was the absence of typical Bruns syndrome, as a result of acutely occurring occlusive hydrocephalus. However, with tumors of the ventricle, dizziness can be very pronounced and even dominate the picture of the disease, being a focal symptom from the bottom of the rhomboid fossa. Then the pathogenesis of the forced position of the head can be understood as a manifestation of tonic reflexes on the neck muscles in connection with irritation of the vestibular apparatus at the bottom of the IV ventricle, i.e., as a phenomenon of a purely reflex nature.
The dependence of this symptom on the participation of secondary vestibular formations is supported by spontaneous bulbar nystagmus and caloric test data: the presence of pronounced thermal nystagmus in the absence of reactive overshoot, which indicated a break in the vestibular pathways from the nucleus to the cerebellum. This fact makes it possible to understand the mechanisms of vestibular dizziness in tumors of the trunk and fourth ventricle and make them dependent on the disinhibition of the function of the vestibular nerve; the auditory function is completely preserved (1).
Severe headaches, vomiting, and cerebellar symptoms could also indicate a tumor of the fourth ventricle; The participation of the trigeminal nerve did not contradict this, which is possible with tumors arising from the lateral indentation of the ventricle (I. Ya. Razdolsky). However, there was cross hemihypesthesia of pain and thermal sensitivity - a symptom that began with a feeling of paresthesia (numbness) as one of the early signs of the disease. This anamnestic fact was not properly assessed, which became obvious retrospectively: neither sensory nor motor conduction disorders are characteristic of tumors of the fourth ventricle, although they cannot be excluded (G. Cushing, I. Ya. Razdolsky).
The latter often observed severe dizziness depending on the position of the head and body. He considers isolated dizziness, as a nesting symptom, to be especially characteristic of tumors arising from the upper half of the rhomboid fossa. The author points out the significant difficulty of differential diagnosis of intrapontine tumors and the indicated part of the brain ventricle. The absence of symptoms from cranial nerves and motor conduction disorders at the onset of the disease also inclined the diagnosis more likely in favor of the ventricle rather than the brainstem.
Thus, the observation shows that the differential diagnosis of tumors of the brain stem and the fourth ventricle is sometimes very difficult and that a lesion of the dorsal pons involving the vestibular nuclei and forced position of the head can simulate a primary tumor of the fourth ventricle.
Patient B., 15 years old, was admitted to the hospital on 2/IX 1954 with complaints of severe double vision and headache. She has been ill since July 1954, but strabismus and diplopia appeared on 26/V 1954.
Objectively: General physical underdevelopment. There was no menstruation. Paresis of the left abducens nerve, diplopia. The fundus is unchanged. Convulsive contractions of the diaphragm occur periodically, which leads to involuntary noisy exhalation. Slightly unsteady, cerebellar gait. There are no motor, sensory or coordination disorders observed.
Cerebrospinal fluid leaked out in frequent drops; protein - 0.39%o, cytosis - 2/3. For 3 1/2 weeks (symptoms are described in sequential order - ——————————— 1 According to G.S. Zimmerman, a forced position of the head, as a consequence of tonic labyrinthine reflexes, is observed with damage to the oral parts of the brain trunk. ——————————— ity of their development) there was some difficulty in speech, absence of the pharyngeal reflex, smoothness of the left nasolabial fold. The girl began to exhibit some psychotic symptoms (lack of criticism of her own condition, depression, etc.). Drooping of the right palatal arch, choking when eating. The gait became unsteady, dizziness, a sensation of noise and ringing were observed, strabismus and diplopia intensified, and horizontal spontaneous nystagmus. Corneal reflexes are reduced.
Peripheral paresis of the left facial nerve, paresis of the soft palate. Diffuse muscle hypotonia, tendon reflexes in the legs are animated, bilateral Babinski's sign. In the left hand there is uncertainty during the finger-nose test, instability with a tendency to fall to the left, and a cerebellar gait. Increased headaches. The patient's condition progressively worsened, drowsiness appeared, and psychotic disorders intensified; the voice became aphonic, and bulbar symptoms increased. The fundus remained normal. Mild right-sided hemiparesis appeared. Violation of coordination tests on both sides.
X-ray of the skull: digital impressions, flattening of the sella turcica. Clinical diagnosis: Brain stem tumor. Operation 10/XI: Trepanation of the posterior cranial fossa, revision of the bottom of the fourth ventricle - no tumor was found. The cerebellar tonsils are lowered and flattened. After separation of the arachnoid adhesions, cerebrospinal fluid appeared. After surgery and radiotherapy, her general condition improved. The patient was discharged on January 22, 1955, and 3 months later she was admitted again in serious condition with apartria, involuntary urination, but still without motor and sensory conduction disorders (there was only anisoreflexia of the limbs and bilateral Babinski's sign). The patient died on 29/IV from bulbar palsy.
Section: The pons is greatly enlarged in volume, the tumor infiltrates mainly the base of the bridge, mainly on the left side; hemorrhages into the tumor tissue. Histologically - astrocytoma.
In this case, the first and for a long time the only symptom of the disease was paresis of the left abducens nerve (diplopia, strabismus); headaches came later, as did breathing problems and an unsteady gait. The fundus was normal. All this made me think at first about brainstem encephalitis. However, subsequent involvement in the pathological process of the facial, auditory and vagus nerves gave reason to suspect the presence of a tumor of the pons, which was facilitated by the appearance of psychotic symptoms (euphoria, moria), then drowsiness, lethargy and others. These disorders, in the absence of signs of intracranial hypertension, should be explained by obvious neurodynamic disturbances of cortical activity due to the presence of a lesion in the brain stem.
In addition to paralysis of the abducens nerve, the vagus nerve was affected, while the facial and auditory nerves were slightly affected (with complete preservation of vestibular function); there were also mild cerebellar symptoms. However, the patient did not have conduction (motor or sensory) disorders, therefore, there were no alternating paralysis. The latter are considered characteristic of brain stem tumors, but, as observation shows, they may not appear even at the height of the development of the disease.
The absence of paralysis of the limbs for a long time cast doubt on the diagnosis of a tumor of the trunk, despite damage to the cranial nerves. This circumstance did not allow us to exclude the possibility of a tumor of the fourth ventricle, especially since the first symptom was paresis of the abducens nerve, which, together with the facial nerve, is most often affected by tumors of the fourth ventricle emanating from the upper half of the rhomboid fossa (I. Ya. Razdolsky). This is what made the decision to undergo revision of the fourth ventricle. The descent of the cerebellar tonsils into the foramen magnum was apparently the cause of the bulbar symptoms.
Noteworthy is urinary retention at the height of the disease, which was then replaced by incontinence, despite the absence of motor pyramidal disorders. We also observed a similar fact in the case of cysticercus of the pons, and L. Ya. Pines and L. O. Sklyarchik in the case of a tumor of the pons (taken for encephalitis).
When comparing the clinical and anatomical data, the discrepancy between the severity of damage to the bridge and the clinic is striking: the almost complete absence of paralysis, despite the tumor predominantly affecting the base of the bridge, while clinical symptoms were observed mainly from the tegmentum - the nuclei of the cranial nerves. This is explained, according to A. N. Ageeva and E. P. Semenova, by the relative preservation of cells and myelin fibers not only in astrocytomas, but also in polymorphic cell glioblastomas. T. M. Strelinskaya and especially L. M. Dukhovnikova emphasize the possibility of a compensatory function of the cortex. This circumstance also contributes to difficulties and errors in the diagnosis of stem tumors. A. N. Ageeva points out that most of the cases she studied anatomically were diagnosed erroneously as a tumor of the cerebellum (cerebellopontine angle); the same fact is noted by E. P. Semenova.
Patient L., 27 years old, was admitted to the clinic I7/XII 1949 with complaints of headaches, speech disorder, and unsteady gait. Ill since early September 1949; in November, paresthesia in the left hand and mild swallowing disorders began to appear periodically. On November 28, the patient stopped working.
Objectively: The fundus of the eye is unchanged. Horizontal nystagmus of the eyeballs. The right corneal reflex is reduced, mild hypoesthesia and a feeling of numbness in the right half of the face. Peripheral paresis of the right facial nerve. Mild dysarthria and dysphagia. Slight left-sided hemiparesis with hyperreflexia, Babinski's sign and foot clonus. Abdominal reflexes are not evoked. Feeling of numbness in the left hand and slight intention tremor. The gait is ataxic. Over the course of two months, the painful phenomena progressed steadily.
Nine days later, there was an absence of the right corneal reflex, weakness of the masticatory muscles, an increase in the masseter reflex, a decrease in taste on the right side of the tongue, an increase in dysphagia and dysarthria and left-sided paresis of the limbs; mild hemihypesthesia, disturbance of coordination tests on both sides, and spastic-atactic gait appeared.
Cerebrospinal fluid: protein - 0.33%o, cytosis - 1/3. 23/I visual acuity and fundus are normal. There is a loss of symmetrical areas in the upper halves of the visual field - partial horizontal hemianopsia, and a narrowing of the visual field to colors along all meridians in its lower halves. Left-sided hemiplegia and right-sided hemiparesis with severe ataxia of the limbs. Aphonia. From 13/II there is paresis of the abducens nerve on the right, limited movements of the lower jaw, atrophy of the masticatory muscles, paralysis of the right facial nerve, decreased hearing on the right, a sharp limitation of tongue movements, paresis of the soft cabbage, and a sharp impairment of swallowing. Anarthria, tetraplegia, hyperpathia of the left half of the body; retention of urine and stool. 20/II the patient died. Clinical diagnosis: Spongioblastoma multiforme of the pons. The anatomical diagnosis is the same.
Recognizing the nature of the tumor and its location did not present any particular difficulties in this case, but at the onset of the disease the presence of symptoms such as nystagmus, dysarthria, paresthesia in the face and hand, increased and uneven tendon and absence of abdominal reflexes, cerebellar symptoms could be indicated in 27 -year-old patient with multiple sclerosis. This was the initial diagnosis. However, headaches, a rapid increase in previous symptoms and the appearance of new symptoms soon gave reason to suspect a tumor of the pons, which was confirmed by the entire further course of the disease. The rapid development of the process made the malignant nature of the neoplasm obvious. The absence of congestive nipples and other signs of increased intracranial pressure confirms the generally accepted idea of the rarity or later appearance of hypertensive symptoms in tumors of the pons. However, according to some data (T. M. Strelinskaya, A. N. Ageeva), they are observed quite often.
Noteworthy are the peculiar changes in the visual field: loss of symmetrical areas in the upper halves of the visual field to white and almost complete horizontal hemianopia to red - an unusual symptom for this localization. It develops in the terminal period of the disease along with tumor growth and is obviously caused by the dislocation of stem formations in the direction of both visual tracts; their compression can explain this kind of change in the visual field, which is generally very rare. (1)
A. N. Ageeva established significant dislocation of the brain stem in many cases of tumors of the pons. —————————————— 1 In the optic cords, such a grouping of fibers is allowed in which the upper and lower sections of the optic tracts are connected, respectively, to the upper and lower halves of the retinas of both eyes. —————————————— Secondary changes in the cerebral appendage due to vascular compression have been described, which led to the appearance of pituitary symptoms (Time). A.D. Dinaburg and D.L. Voloshchenko discovered the mixing of brain formations in the direction of the chiasmatic cistern.
It should be noted that in this, as in many other cases, changes in the visual field appear more clearly when examined with the help of colored marks. In addition, for the red color there is a narrowing along all meridians and the lower halves of the visual field, which confirms the actual existence of these visual disorders. Obviously, the appearance of this symptom is possible only in later stages of the disease, but detection of visual field defects then becomes especially difficult due to the serious condition of the patient.
Patient M., 32 years old, was admitted to the clinic on December 7, 1945, with complaints of attacks of headaches, sometimes with vomiting and involuntary urination, and blurred vision. She has been ill since the summer of 1943, when the above symptoms and short-term loss of consciousness first appeared. Since then, the mentioned attacks have been repeated at intervals of up to six months. In the spring of 1945, a convulsive attack developed; tapeworms (tapeworm) were discovered. Since September, decreased vision has been noted; in October, pain in the right half of the face and a feeling of numbness in the left hand, double vision and staggering when walking. Sometimes during attacks I experienced a peculiar sensation: “some kind of hot stream will flow deep in the forehead and the urge to stool immediately arises.” In November, the patient's condition noticeably worsened, and night and morning headaches appeared.
Objectively: Sharply expressed congestive nipples. The pupils are unchanged. Atrophy of the masticatory muscle and absence of the mandibular reflex on the right. Hyperesthesia in the area of innervation of the first and second branches of the right trigeminal nerve. Forced position of the head: the patient throws it back, sometimes tilting it to the right and supporting it with her hands. Slight neck stiffness, mild Kernig's sign. Slight left-sided hemiparesis, worsening after hypertensive attacks. Sensitivity is not impaired. Craniogram without changes.
Convulsive attack I2/XII with loss of consciousness; the muscle tone of the left arm is sharply increased, it is bent at the elbow joint, the left leg is in a state of extension; pulse weak, rare; face pale. After the attack, ptosis of the right eyelid, nasal tone of speech, and paresthesia in the right half of the face were observed. Clinical diagnosis: Cysticercosis of the brain (region of the pons, cerebellum). The patient died on December 18, 1945.
Section: On the right in the area of the putamen, in the optic thalamus and in the cortex of the inferior parietal lobule there are separate bubbles of the cysticercus. In the pons, at the level of the root of the fifth pair on the right, there is a single bubble, the size of a small hazelnut (well encapsulated, with a fin inside), forming a protrusion into the cavity of the fourth ventricle.
In this observation, it should be noted the very rapid development of the disease with severe hypertensive crises, which led the patient to death 11 days after admission. The diagnosis of cysticercosis was not in doubt, as was the localization of the process in the pons. Attacks of pain and paresthesia in the face were sometimes accompanied by paroxysmal disorders of complex visceral functions - urination and defecation, which are usually not observed with damage to this level. This indicates the possibility of the development of seizures with dysfunction of the bladder and rectum when the pons is damaged, as the clinic shows, apparently through a reflex pathway from the trigeminal nerve nucleus. The above once again indicates a very close functional relationship between the animal and autonomic nervous systems.
Doubts could arise when explaining movement disorders, namely seizures of unilateral tonic convulsions. The position of the limbs of the Wernicke-Mann type, which characterizes these convulsions, and transient post-seizure stem symptoms (ptosis, paresthesia in the facial area, paresis of the soft palate) undoubtedly indicated their stem origin.
The forced position of the head with its deviation back, which is rarely observed in general, and the Bruns symptom complex (in the absence of cerebral hydrocele) are apparently explained by the protrusion of the cysticercus bubble from the substance of the brain into the cavity of the fourth ventricle, which disrupted the circulation of the cerebrospinal fluid and thereby contributed to the occurrence of hypertensive crises. In this case, the position of the cysticercus bubble, generally rarely observed in the pons, explains the periodic nature of the occlusion of the Sylvian aqueduct at the site of its entry into the IV ventricle and thereby the onset of severe hypertensive crises.
Here, the possibility of a once living cysticercus of the fourth ventricle, which only later turned out to be “immured” in its bottom, cannot be excluded, as sometimes occurs in connection with reactive inflammation of the ependyma in the circumference of the bladder.
See further: Multiple brain tumors >>
Diagnostics
Based on the medical history information obtained by the neurologist and the results of detailed neurological diagnostics, a preliminary diagnosis is established. For confirmation, neuroimaging examinations are used - computed tomography, magnetic resonance imaging, MSCT.
MRI using a contrast solution provides particularly complete and accurate information about the tumor. High-resolution imaging can detect small tumors that are not visible on CT scans.
MRI results suggest determining the histological structure of the tumor, determining in advance the growth pattern, the extent of exophytic growth of the tumor element and the level of infiltration of the medulla. It is necessary to conduct a detailed collection of all data to determine the likelihood and rationality of surgical treatment of the tumor.
Interpretation of MRI examination data reveals the concentration of the tumor, the forms of accumulation of the contrast agent - uniform, uneven, ring-shaped. If the tumor has a diffuse or infiltrative structure, the outlines of the staining do not correspond to the actual size of the pathogenesis.
In T2 mode, the MR signal changes its propagation to areas where the contrast agent has not accumulated. These areas may be an area of swelling of brain tissue, a space for its growth, or both. The simplest neuroectodermal formations are determined by the presence on MRI images of implantation metastases in the ventricular system of the brain, in the subarachnoid spaces.
It is important to differentiate tumor processes in the brain stem from multiple sclerosis, brain stem inflammation, demyelinating encephalomyelitis, ischemic stroke, intracerebral hematoma, and lymphoma.
Treatment of neoplasms
Previously, there was a widespread belief that stem tumors are not subject to surgical treatment due to the fact that they have an infiltrative nature and are capable of diffusely growing into stem elements.
Despite the fact that among all stem structures, most tumors have diffuse germination, sometimes there are delimited nodular formations that are easily removed. Before choosing treatment tactics and deciding on the possibility of surgical intervention, the patient needs to consult a neurosurgeon.
The preferred method of eliminating a brain stem tumor is the maximum possible resection of the tumor with minimal damage to brain structures. Microneurosurgical surgical techniques are developing and provide a chance for a higher level of treatment.
Almost 80% of brain stem tumors are considered inoperable forms. Chemotherapy and radiation treatment are used for inoperable forms, in the preoperative and postoperative period. Cytostatic agents are used in combination form for chemotherapy. 75% of patients receive symptom relief from radiation therapy. The vast majority of cases of the disease end in the death of the patient. Radioisotope treatment can prolong the life of children with similar tumors. The life expectancy of 30% of children who underwent radiotherapy increased by 2 years.
Stereotactic radiosurgery is the newest method for treating brainstem tumors. Two types of radiosurgery can be performed:
- gamma knife - a special helmet is placed on the patient’s head for irradiation from multiple points. The rays converge at one point where the tumor focus is localized. Healthy tissues are practically not affected by this effect. Each beam has a small amount of gamma energy, but the total effect of all beams contributes to achieving maximum effect.
- cyber knife - performed using a robot and is an automated procedure. The device independently concentrates radiation into the area where the tumor is located. The patient's movements and breathing prevent any confusion in aiming the beam of rays.
Studies prove the validity of these methods in the treatment of benign neoplasms up to 3.5 cm in size.
Today, three main types of brain stem tumors are identified:
- Ependymoma
- Glioma
- Astrocytoma
Due to the location of the tumor, treatment requires the highest skill of the surgeon and the most modern equipment.
At the Imedical Medical Center , depending on the size of the tumor, two tactics are used to treat brain stem tumors.
To accurately determine the location and size of the tumor, it is necessary to conduct an MRI scan of the brain. The cost of an MRI of the brain is 1,200 USD.
After the MRI, the radiologist interprets the images and they are sent to a scientific council consisting of two of the world's strongest brain neurosurgeons: Professor Zvi Ram and Professor Nevo Margalit . They determine the optimal tactics for further treatment of a brain stem tumor. In the case of ependymoma, the treatment tactics are determined by Professor Shlomo Konstantini .
If the tumor size does not exceed 35 mm, stereotactic radiosurgery is the tactic of choice. Stereotactic radiosurgery is a modern bloodless and painless radiation method for treating pathological lesions of the brain and spinal cord. The principle of operation is that a focused X-ray beam destroys DNA structures in tumor cells, thereby stopping the growth of the tumor. The rays hit tumor tissue and metastases with extreme precision, while at the same time not damaging healthy tissue and brain cells. Treatment can take place either in one session (high dose of radiation) or in several, depending on the location and type of tumor.
The cost of treating brain stem tumors in Israel at the Imedical Medical Center using stereotactic radiosurgery is from 22,000 USD.
If the tumor size exceeds 35 mm, the tactic of choice is neurosurgical craniotomy. Professor Nevo Margalit is one of the three best neurosurgeons in the world for the removal of brain stem tumors and, according to Forbes magazine (Israel), has the highest success rate of operations for this pathology in Israel.
The cost of craniotomy surgery for a brain stem tumor in Israel at the Imedical Medical Center:
- Consultation with Professor Nevo Margalit – 550 USD
- Preoperative thorough preparation (X-ray of the lungs, ECG, consultation with an anesthesiologist) - 110 USD
- Craniotomy operation (the operation is performed personally by Professor Nevo Margalit) - from 32,000 USD
For questions regarding the treatment of brain stem tumors in Israel, leave a request or call: +7 (in Russia) or + (972) 528 282 416 (Viber, WhatsApp)
Forecast for the development of the disease
The slow growth and subclinical course of benign neoplasms allow the disease to last up to 10-15 years. Malignant forms of tumors respond poorly to treatment. From the first symptoms it takes from a month to several years before death. Specific treatment alleviates symptoms and slightly prolongs the patient's life.
An MRI is necessary to diagnose a brain stem tumor. You can choose a clinic using our website. Registration for an appointment is free.