HEMORRHAGIC CORTICAL RENAL NECROSIS
(Greek, haimorrhagia bleeding; lat. corticalis cortical; necrosis; synonym
symmetrical cortical necrosis of the kidneys
) - a disease caused by spasm and thrombosis of the renal vessels with subsequent necrosis of the glomeruli and tubules of the renal cortex and clinically manifested as acute renal failure.
G. Ph.D. item was first described by the French. doctor Juhel-Renou (E. Juhel-Renou) in 1886. The largest number of patients with this pathology is presented in the work of Sheehan and Moore (H.L. Sheehan, H.S. Moore, 1953). In childhood, the disease occurs mainly in boys in the neonatal period and only in 10% of cases over 2 years of age? W adults G. k.n. p. is more often observed in women aged 20-35 years.
Etiology and pathogenesis
One of the causes of cortical necrosis of the kidneys may be the hemolytic process (hemolytic disease of the newborn, hemolytic-uremic syndrome, etc.), intrauterine and postpartum hypoxia and fetal asphyxia.
In women, the development of the disease is associated with abundant menorrhagia and metrorrhagia, as well as with pathology during pregnancy and childbirth (premature placental abruption, massive placental hemorrhages, placenta previa, eclampsia) and intensive treatment with vasoconstrictors (oxytocin, norepinephrine). A smaller role in the etiology of G. k.n. etc. are played by surgical interventions, burns, severe infections, disseminated neoplasms.
The basis of G.’s pathogenesis is c.n. n. there are disorders of the renal circulation according to the type of ischemia that occurs in various pathol, conditions. For ischemia lasting up to 3 hours. mainly the tubules are affected; longer ischemia leads to necrosis of the cortex.
Causes
If we talk in detail about what kidney necrosis is, then this condition can be characterized as structural damage to the proteins of the cytoplasm of the cells of a paired organ, as a result of which the death of individual sections of the kidney tissue is observed.
This condition occurs with equal frequency in both adult patients and newborns. Potential factors for the development of necrotic changes include:
- Generalized spread of infection throughout the body (sepsis);
- Traumatic injury to the kidney area;
- Rejection of a previously transplanted kidney by the body;
- Placental abruption in a pregnant woman;
- Bites from poisonous snakes and insects;
- Poisoning by toxic components and chemical compounds;
- Complications of existing vascular and heart diseases.
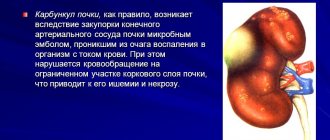
Pathological anatomy
Macroscopically, the kidneys are enlarged, dark red or chocolate in color, swollen, and flabby. The cortex is thinned. There are many areas of necrosis and hemorrhage on the surface of the kidneys and on the incision. The kidney pyramids and mucous membrane of the pelvis are unchanged. When gistol, the study finds multiple blood clots of interlobular arteries and afferent arterioles, in places accumulation of lymphoid cells in the interstitial tissue. In the future, mineralization (calcification) of necrobiotic areas is possible.
Complications and prognosis
The only possible complication for each form of renal necrosis is functional renal failure. This condition is characterized by severe intoxication of the whole body, heart failure and septic complications. Only timely diagnosis and proper treatment can save a person’s life.
With timely treatment, it is possible to preserve the paired organ and restore its functional state.
Despite this, statistics indicate that 70% of patients with a similar problem require an organ transplant. For patients with diagnosed necrosis, hemodialysis is vital. In especially severe cases, if treatment is not timely, death is likely. Share:
Clinical picture
Kidney damage in newborns and infants develops against the background of otitis, mastoiditis, meningitis, and nasopharyngitis. The leading symptom of G. k.n. n. in newborns there is anuria (see), which is difficult to diagnose due to physiol, oliguria (see) in the first days of life. The disease is accompanied by fever, vomiting, diarrhea, dehydration, red blood cells, white blood cells, hyaline and granular casts are noted in the urine. Moderate anemia, hyperleukocytosis, neutrophilia with a shift to the left, and thrombocytopenia are observed. Edema and hypertension are usually absent. In neurol, the status is initially dominated by anxiety, convulsions, and then drowsiness, hypotension, coma develops with impaired breathing and swallowing. In the terminal stage, bloody vomiting (see Hematemesis) and melena (see). In adults, in addition, severe lower back pain is noted. Changes in other organs are associated with the disease preceding G. c. n. P.
G. Ph.D. may be complicated by progressive anemia, cerebral edema (see Edema and swelling of the brain), nephrotic syndrome (see).
Classification
Depending on the location of necrotic changes and the processes occurring in the paired organ, the following types of renal necrosis are distinguished:
- Tubular (acute) necrosis. In this case, necrotic changes affect the epithelium of the renal tubules. The disease itself is divided into nephrotoxic and ischemic necrosis. Nephrotoxic necrosis is triggered by toxic and chemical compounds entering the paired organ. Ischemic necrosis, as a rule, occurs during shock, sepsis, and also against the background of traumatic injuries. Tubular necrosis is characterized by an intense inflammatory process, under the influence of which the tissue of the paired organ is damaged, its structure changes and failure is formed.
- Cortical necrosis or mercuric bud. This pathology occurs when there is partial or complete obstruction (blockage) of the blood vessels supplying the paired organ. With insufficient blood supply, the functional state of the kidney is disrupted and kidney failure occurs. In no less than 35% of cases of diagnosed cortical necrosis, the pathology arose against the background of septic damage to the body. In addition to sepsis, the disease can be triggered by intoxication with chemical compounds, burns, transplantation procedures and injuries. In newborns, cortical renal necrosis occurs if a pregnant woman is faced with the problem of placental abruption.
- Papillonecrosis. The papillary form of this disease is characterized by the involvement of the renal medulla and renal papillae in the necrotic process. At least 3% of people who have previously had pyelonephritis experience complications in the form of papillary necrosis. Female patients are 2 times more likely to experience this disease.
Treatment
Treatment is aimed primarily at eliminating anuria and acute renal failure. The amount of fluid administered per day should correspond to the amount of urine excreted (for children of the first year of life - no more than 30 ml per 1 kg of weight per day). The administration of fluid is carried out under the control of water-salt balance and acid-base balance. To prevent protein catabolism, lipids and concentrated glucose are administered intravenously. Due to the presence of foci of infection, antibiotic therapy is carried out with non-toxic drugs (oxacillin, methicillin and other penicillin derivatives). To improve renal hemodynamics, heparin (100-120 units/kg intravenously) is indicated. In the absence of effect from symptomatic therapy, they resort to exchange blood transfusion (see), peritoneal dialysis (see), as well as hemodialysis (see).
Symptoms
The clinical manifestations of renal necrosis directly depend on the form of the disease.
In the acute form of papillary necrosis, the patient is bothered by acute pain, severe chills and fever. In addition, when the bladder is emptied, fragments of blood are visible in the urine. If the patient is not provided with timely assistance, then within 3-5 days he will develop acute renal failure. The chronic form of papillary necrosis is manifested by moderate pain in the lumbar region, leukocytosis in the urine, as well as signs of sickle cell anemia.
When a mercuric bud forms, the following clinical symptoms come to the fore:
- Partial or complete absence of emptying the bladder;
- Pain in the area of the projection of the kidneys;
- The appearance of blood fragments in urine, as a result of which it acquires the characteristic color of urine during renal necrosis: brown or red;
- Decrease in blood pressure;
- Increase in body temperature.
The tubular form of renal necrosis is characterized by the following clinical manifestations:
- Swelling in the face, neck and lower extremities;
- Drowsiness;
- Nausea and vomiting;
- Decreased volume of urine excreted;
- Severe damage to the central nervous system, which manifests itself in the form of confusion, even coma.
It is important to remember that failure to provide timely assistance to a person with signs of one or another type of renal necrosis will lead to death in a short period of time.
Forecast
The prognosis is bad. Death usually occurs 10-15 days from the onset of the disease. Recovery is noted in some cases.
See also Kidney failure.
Bibliography:
Kidney diseases, ed. G. Mazdrakova and N. Popova, trans. from Bulgarian, p. 533, Sofia, 1973, bibliogr.; Guide to Clinical Urology, ed. A. Ya. Pytelya, M., 1969; BouissouH. ea La dog corticale sym6trique des reins du nourrisson (fitude clinique, etiolo-gique et th6rapeutique), Ann. P6diat., t. 10, p. 2317, 1963; Juhel-RenoyE. De l'anurie precoce scarlatineuse, Arch. g£n. M6d., t. 17, p. 385, 1886; Sheehan H.L. a. Moore HC Renal cortical necrosis and the kidney of concealed accidental haemorrhage, Oxford, 1953.
V. P. Lebedev.
Diagnostics
To correctly formulate a diagnosis, the doctor collects the patient’s medical history and analyzes his complaints. The list of medications used is important, as well as the presence of diseases such as diabetes and heart failure.
It is also important to take into account information about possible contact with poisonous, toxic and other chemical compounds. The following laboratory and instrumental examination options will help confirm the clinical diagnosis:
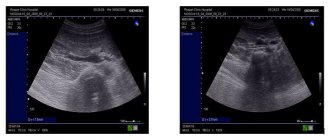
- Ultrasound examination of the kidneys;
- X-ray examination;
- General clinical blood test;
- General and bacteriological urine analysis;
- Computer or magnetic resonance imaging.
Kidney necrosis
Kidney necrosis is a pathological process manifested in swelling, denaturation and coagulation of cytoplasmic proteins, and cell destruction. The most common causes of necrotic kidney damage are interruption of the blood supply and exposure to pathogenic products of bacteria or viruses.
The kidney is a paired bean-shaped organ, its main function is urine formation and regulation of the body's chemical homeostasis (blood filtration). The right kidney is slightly shorter, usually located 2–3 cm lower than the left kidney, it is more susceptible to any diseases. On the upper parts of the kidneys there are adrenal glands that produce the hormones adrenaline and aldosterone, which in turn regulate fat, carbohydrate and water-salt metabolism, the functioning of the circulatory system, skeletal muscles and internal organs.
Symptoms and treatment of kidney necrosis
Kidney necrosis is diagnosed during destructive processes in the tissues of the organ, which are manifested by swelling of protein molecules. Kidney destruction develops as a pathological complication of many diseases or as a result of intoxication of the body. This disease is dangerous because it can initiate kidney failure.
Symptoms and treatment of kidney necrosis.
RENAL PAPILLA NECROSIS
RENAL PAPILLA NECROSIS
(syn.:
papillary necrosis, necrotic papillitis, necrosis of the renal medulla
) - ischemic infarction of the renal medulla with purulent melting, rejection of necrotic tissue and dysfunction of the organ. This disease was first described by N. Friedreich in 1877. Necrotic changes are based on circulatory disorders in the renal medulla and renal papilla due to inflammatory metabolic and vascular changes in the kidney, impaired urine outflow with the occurrence of intrapelvic hypertension and renal pelvic reflux, purulent -inflammatory process in the renal medulla, changes in blood composition. In accordance with this, infectious, angiopathic and vasocompression factors of P.’s pathogenesis are isolated. n. Usually there is a combined effect of these factors. Pyelonephritis (see) is the most common inf. a disease combined with necrosis of the renal papillae, and in most cases is one of its main causes. The unique anatomical and physiological characteristics of the renal medulla under conditions of ischemia (for example, a decrease in the diameter of the vessels towards the apex of the papilla, an increase in blood viscosity and a slowdown in blood flow) predisposes to the development of necrotic changes in the renal papillae.
In accordance with infectious and angiopathic factors, it is customary to distinguish between primary and secondary P. s. n. With primary P. s. n., arising as a result of circulatory disorders, the purulent process is a complication; in the secondary case, necrotic changes are a complication of pyelonephritis. Necrotic processes in the renal medulla can be a complication of diabetes mellitus. However, among patients with P. s. n. Diabetes mellitus occurs in no more than 15% of cases.
With P. s. n. 40% of patients experience the formation of urinary stones (see). This is due to the fact that necrotic masses are easily encrusted to form a calculus.
Along the flow of P. s. n. can be acute or chronic. The acute course is accompanied by severe intoxication and high fever. Since P. s. n. often combined with nephrolithiasis and pyelonephritis; according to the wedge, its manifestations are similar to these diseases. In addition to lower back pain, often in the form of an attack of renal colic (see Kidney stone disease), total hematuria is observed (see Hematuria). The only pathognomonic symptom of P. s. n. - discharge of necrotic masses in the urine, which is observed only in 10% of cases. Bilateral P. s. n., combined with pyelonephritis, quickly leads to renal failure (see).
For chronic P. s. n. less violent manifestations are characteristic in the form of episodically recurrent macrohematuria, bacteriuria (see), leukocyturia (see).
In the diagnosis of P. s. n. What matters is the wedge, the symptoms of the disease (hematuria, renal colic, fever) and laboratory data. urine tests. Microscopic examination reveals necrotic masses in the urine, in which the contours of the stroma of the renal papilla are sometimes visible.
Retrograde pyelogram with necrosis of the renal papillae: cavities in the pyramids of the kidney (indicated by arrows) formed as a result of papillary necrosis.
The main method of diagnosing P. s. n. is rentgenol, research. A survey image of the abdominal cavity may reveal shadows of calcification caused by calcifications of necrotic masses of the renal papilla, as well as the shadow of a triangular-shaped calculus with areas of rarefaction in the center. With excretory urography (see) and retrograde pyelography (see), which must be performed in different projections, two types of P. s. n. (fornical and papillary) with characteristic rentgenol, signs - blurred contours of the papilla and fornix, erosive changes, the formation of fistulas with the flow of contrast agent into them, amputation of the calyx, rejection of the papilla, as well as the formation of cavities communicating with the calyces (Fig.). Renal angiography, isotope renography, scintigraphy, and ultrasound scanning have no independent diagnostic value.
Differential diagnosis
carried out with kidney tuberculosis (see Extrapulmonary tuberculosis) and kidney tumors (see).
Treatment
P.S. n. conservative and surgical. Conservative treatment of patients with acute course of P. s. n. (catheterization of the ureter to restore urine passage, antibacterial and hemostatic therapy, etc.) mainly symptomatic; it is more often carried out not so much about P. s. n., how much due to its complications. In the absence of effect from conservative treatment of acute P. s. n. Surgery is indicated within 24 hours from the onset of the disease. Considering the frequency of bilateral lesions, organ-preserving operations are mainly used - nephropyelostomy or kidney resection. Nephrectomy (see) is performed only in case of unilateral total papillary necrosis with irreversible purulent-inflammatory changes.
Treatment of patients chronic. P.S. n. aimed at improving blood circulation in the kidney; Heparin, venoruton, and also saluretics (furosemide) are prescribed; in the presence of a purulent-inflammatory process, antibacterial drugs are prescribed.
Forecast
largely depends on the severity of the wedge, manifestations. Even with timely diagnosis and therapy, mortality in the acute course of P. s. n. is 10% (previously approx. 50%).
Prevention
consists mainly in the fight against purulent-inflammatory diseases of the urinary tract.
Bibliography:
Murvanidze D. D. About the clinical features and course of necrosis of the renal papillae in children, Tbilisi, 1973; Pytel Yu. A. Necrosis of the renal papillae, in the book: Pytel A. Ya. et al. Izbr. chapters nephrol, and urol., part 2, p. 165, L., 1970; Hultengren N. Renal papillary necrosis, Acta chir, scand., suppl. No. 277, 1961; Jones LW a. Morrow JW Renal papillary necrosis, management by ureteral catheter drainage, J. Urol. (Baltimore), v. 106, p. 467, 1971; Lindvall N. Renal papillary necrosis, Acta radiol. (Stockh.), suppl. jvft 192, 1960; L udvik W. Die Papillennek-rose, Urologe, Bd 7, S. 36, 1968; R e-nyi-V£mos F. a. Balogh F. Pyelonephritis, p. 129, Budapest, 1979; Tauber t W. u. Prager W. Zur
Genese von Nierenpapillennekrosen, Radiobiol. Radiother. (Berl.), Bd 11, S. 381, 1*970.
Yu. A. Pytel.