There is mucus in the eyes. Features of treatment
Treatment of adults and children includes comprehensive measures to combat ophthalmological disorders.
To determine the root cause, the pathological secretion is taken for analysis. Before going to a specialized facility, treat your eye. Soak a cotton swab with an antiseptic solution and wipe from the outer edge to the inner corner. Depending on the underlying disease, antiviral or antibacterial agents are prescribed. In some cases, the use of systemic drugs may be necessary.
To treat allergic conjunctivitis, it is extremely important to determine the substance to which the body is hypersensitive and to eliminate contact with the allergen. Next, antihistamines are prescribed, as well as rinsing with solutions based on medicinal decoctions
Viral conjunctivitis is treated with antiviral drops and ointments, as well as means to boost immunity. Pathological processes caused by exposure to fungal infections require an integrated approach to treatment. As a rule, this is a long and systematic struggle.
Traditional treatment is an auxiliary therapy
Traditional methods can only be used after a doctor’s permission, otherwise they may harm you. At home, you can prepare compresses and rinsing solutions yourself:
- prepare a regular aqueous solution based on table salt. You only need one pinch of salt, which is diluted in a tablespoon of warm boiled water;
- Use chamomile and calendula infusion as a rinse. Three tablespoons of dry raw materials are diluted in a glass of water. After the solution has cooled, it should be filtered. The resulting decoction can be used as a lotion;
- You can also use black tea leaves. It is used both in the form of lotions and for rinsing.
As they say, a hundred grams of prevention is better than a kilogram of cure.
The following tips will help you prevent the development of eye diseases:
- undergo preventive examinations with an ophthalmologist;
- You should use clean tap water as a wash;
- do not use other people’s decorative cosmetics;
- observe the rules of personal hygiene;
- If possible, avoid contact with substances that can cause an allergic reaction;
- treat somatic diseases in a timely manner;
- if the quality of vision decreases, wear glasses;
- Do not select contact lenses yourself, entrust this choice to a specialist.
Treatment of eye diseases
The treatment regimen is prescribed by an ophthalmologist taking into account the pathogen, stage of the disease, and the presence of complications. Almost all eye diseases require local treatment with medicinal solutions, compresses, and ointments. If eye diseases accompany diseases of the ear, nose, throat, or respiratory tract, then it is imperative to cure them, otherwise a relapse will occur. In such cases, an integrated approach is effective.
For the treatment of viral eye diseases, acyclovir is used in combination with local treatment with furatsilin solution, ophthalmoferon, albucid, and combination drugs.
When a viral bacterial infection is associated, drops containing antibiotics (ciprofloxacin, chloramphenicol) are prescribed. To treat allergic eye diseases, you cannot do without topical antihistamines (drops, ointments) and tablets.
Traditional methods of treatment
Eliminate discomfort and improve vision using lotions with a remedy such as a decoction of eyebright or mistletoe, as well as cornflower. You can also use chamomile, birch leaf, plantain, caraway, nettle, oak bark, yarrow, celandine, calendula (twice a day for ten days) or applications of carrots, cucumber, cabbage, dill, celery, aloe juice and Kalanchoe.
When barley appears at the beginning of the disease, you need to wipe the eyelid (or keep a soaked napkin on the sore spot until dry) with any alcohol-based cosmetic (eau de toilette, cologne) or apply heated (wrapped in cloth) flax seeds, sand, mustard (dry). Compresses made from raspberry, apple, currant, and cherry leaves (each plant separately) are effective. Drink the same decoction as tea for a long time.
When to see a doctor
For any eye disease, you should definitely go to a specialist, because otherwise you can simply lose your sight. You should not engage in self-diagnosis, especially since sometimes the cause can be quite difficult to identify, and a comprehensive examination is required. After this, the ophthalmologist will prescribe adequate therapy.
Strings of mucus in the eyes.
| Where do purulent threads in the eyes come from? |
| GKos Moderators 50 messages About 3 years ago I came from the sea and I began to have white discharge of pus from my eyes in the form of a stringy thread like a rubber band. At first I thought it was just a sleepy discharge, like everyone has in the morning, but over time it grew into long strings that could be pulled out of the eyes, my visits to doctors did not help, they prescribed different eye drops, but the problem remained the same... I work on the computer a lot, maybe this is the problem? Last year I went to the sea and washed my eyes in salt water, then there was less discharge, when I returned back everything continued. My eyes are tired all the time, sometimes it seems that there is sand in them... In winter I suffered from sinusitis, by spring I was cured, but the discharge remained. What should I do in this case so that “IT” does not develop into a chronic form? |
| DonAtom Administrators 411 messages In your case, there may be two conditions that cause the complaints you described. Persistent discharge from the eyes is a symptom that should be investigated by specialists. Usually, a microbiological examination of discharge from the conjunctival cavity is carried out - inoculation of the discharge on a nutrient medium in order to identify microorganisms and their sensitivity to antibiotics. They also conduct a biomicroscopy of the surface of the eyes and find out if you have concomitant infectious diseases (eg sinusitis, rhinitis, caries). Often this examination needs to be carried out more than once. When the results are received, specific treatment is prescribed. Since the complaints have been present for several years, treatment may also take some time - weeks. Constant work at the computer is a risk factor for dry eye syndrome and computer syndrome. While working at the monitor, the accommodative (focusing) system of the eyes is in constant tension. In addition, involuntarily, through concentration of attention and vision, subconsciously the blinking movements of the eyes thin out, causing the protective tear film to evaporate from the surface of the eye faster. With such daily work, the eyes may become red, itchy, and watery. There may also be a feeling of dryness and foreign matter in the eyes. Therefore, it is recommended to take short but frequent breaks during work, say 5 minutes every hour and a half, get up from your workplace, look into the distance, and the like. Moisturizing drops may also help. They can be purchased without a prescription and used as needed. The best are drops containing hyaluronic acid. In your case, you should start by examining and treating the discharge present, as it may be a source of chronic infection. Conjunctival culture can be performed in any clinical laboratory with a referral from the attending physician. |
| darsi Users 1 message Apparently I have the same “threads”. I went to see many doctors and they thought I was crazy, because... They are not constantly in the eye, but during periods of exacerbation or appear in the evening. I was able to take a photo.
|
| Real Users 1 message I had the same thing. My eyes were festering and I didn’t know what to do. I went to the ophthalmologist, to the infectious diseases department, they did cultures for me and they prescribed me various antibiotics for instillation, more and more powerful (about 10 types). None of the doctors really understood what kind of conjunctivitis I had and how to treat it. I was diagnosed with chronic conjunctivitis. How much money did I spend on medicines... The disease lasted for more than 5 years and nothing helped! Pus poured out and these transparent threads did not let go of me. My vision has deteriorated greatly. It was impossible to work, my eyes itched, I took sick leave... it was a real punishment. I wear lenses, and since all the lenses were infected, I specially switched to one-day lenses and changed them every day. Then I gave up the lenses for a month, dripped and dripped and rubbed my eyes with ointments - nothing helped! And then an accident helped! I went to work in Africa, central western Africa - just where Ebola is now. And there in Africa I picked up a tropical disease - amoeba (like dysentery). And there they gave me metronidazole to drink to treat amebiasis. As a result, I recovered and, strangely enough, both the festering eyes and these terrible threads disappeared!!! Currently, 2 years have passed since the cure, everything is fine with me. If you need details you can contact me. In general, METRANIDAZOLE (a cheap drug) and possibly powerful equatorial ultraviolet helped me. In general, consult your doctor in advance. This is my story. Be healthy. |
| Inna_S Users 1 message Of course, the best way to solve your eye problem would be to go to the clinic, make an appointment with a doctor to get an accurate diagnosis and recommendations from a specialist. In general, there are many remedies for eye inflammation, antibiotics, for example Floxal ointment, or there are other drops. You bury them, they kill all your microbes and heal your eyes. It’s just that when you don’t know what’s wrong with them, it’s not clear how exactly to treat them. |
Approaches to the treatment of pus in the eyes
If you experience pathological purulent discharge in the morning, itching, burning, or difficulty opening your eyes, obaGlaza suggests rinsing them carefully. Popularly, this is done using tea leaves, chamomile infusion, calendula, a weak solution of potassium permanganate, or plain water if there is no antiseptic on hand. Each of the products has natural anti-inflammatory, drying and soothing effects.
The first stage of traditional medicine, notes ObaGlaza.ru, will be to find out the cause of the pus. The second is the choice of treatment, consisting of drugs that act directly on the cause of pus in the eyes, as well as auxiliary drugs. The favorite form of medication is eye drops and ointments. They may contain antibiotics, anti-inflammatory and bactericidal agents, and antihistamines.
Treatment of purulent discharge, according to the etiology of the disease
The main goal of treating pus in the eyes is to eliminate the pathogenic agent:
- Bacteria
. For a bacterial infection, antibiotics should be taken. Usually these are groups of fluoroquinolones (such as Floxal) or aminoglycosides (such as Framecitin). You can apply erythromycin or tetracycline ointment at night; - Fungus
. Fungal agents and other microorganisms that form pus are amenable to Sofradex - a mixture of antibiotic, antiseptic and anti-inflammatory agent; - Allergy
. In the case of an autoimmune disease, where a bacterial infection subsequently appears, it is necessary to treat with both antibiotics and antihistamines.
Adjuvant therapy
Anti-inflammatory drugs, antiseptics and other procedures are used:
- For dacryocystitis, light massage of the eyelids and rinsing of the nasolacrimal duct are appropriate;
- Albucid, Oftomirin, Vitabact have a strong bactericidal effect;
- According to ObaGlaza, hydrocortisone ointment has a good anti-inflammatory effect;
- Ophthalmologists resort to folk remedies if this really helps to quickly get out of the pathological condition and remove pus (for conjunctivitis, blepharitis, dacryocystitis, etc.).
To get quick results with “pus drops,” you need to use them correctly:
- A drop or two is enough, since the lacrimal sac still only holds one, no more. Everything else is wasted.
- If the patient wears lenses, ObaGlaza.Ru recommends limiting their use during the treatment of pus.
- Also, in the outer corner of the eye, and not in the inner (in the direction of the tear flow).
- When treating one eye, prevent suppuration of the other, it is important to separate the treatment procedure: use different tampons for rinsing and massage, and wash your hands thoroughly before touching a healthy organ.
Crusts in the corners of the eyes. Squamous blepharitis
Scaly blepharitis (seborrheic) is a disease in which the edges of the eyelids are affected.
A characteristic feature is that a white or yellow crust appears at the base of the eyelashes, similar to seborrhea. Usually inflammation occurs in both eyes.
The disease can affect not only the eyelids, but also the eyebrows and scalp.
Children and people with weakened immune systems are at risk. Blepharitis can also be a consequence of other eye diseases. Scaly blepharitis can appear at any age.
Forms of the disease
Classified according to the location of blepharitis:
- anterior marginal - the mildest form of seborrheic blepharitis, a person’s eyelids are affected only along the ciliary line;
- posterior marginal - pathology affects the meibomian glands;
- angular (angular) - blepharitis is localized in the corners of the eyes.
According to the nature of blepharitis:
- spicy;
- subacute;
- chronic.
Stages
In medicine, there are three stages of the disease:
- Stage 1 - manifested by slight redness and itching of the eyelids;
- Stage 2 - flaky scales appear on the eyes, swelling and itching intensify. A person may feel pain, burning;
- Stage 3 - pus and blood are found under the crusts, discharge from the eye sticks together, forming bunches.
Causes
There are many factors for the development of the disease, the main ones are:
- decreased immunity;
- infectious and viral diseases;
- unfavorable living conditions;
- failure to comply with hygiene rules;
- endocrine pathologies.
You should know that the scaly type of blepharitis is usually accompanied by seborrheic dermatosis, which affects the scalp.
Additional causes of the disease:
- visual defects (myopia, farsightedness);
- dry eye syndrome;
- diseases of the oral cavity (caries, periodontal disease);
- long exposure to unfavorable weather conditions (rain, wind);
- chronic diseases of internal organs;
- lack of vitamins;
- allergy.
Signs and symptoms
The main symptom of the disease is the appearance of flaky scales on the eyelids. At the same time, the scales are very firmly adhered to the skin, so it is difficult to remove them from the eyelids.
It is also worth noting that experts categorically prohibit removing crusts that have formed on the eyelids; this action can lead to the formation of ulcers and erosions.
The following symptoms are also characteristic of scaly blepharitis:
- swelling and redness of the eyelids;
- burning and itching;
- photosensitivity;
- eyelash loss;
- rapid eye fatigue;
- cloudy discharge from the sebaceous glands.
Most people with scaly blepharitis have keratoconjunctivitis, which is characterized by symptoms such as a sensation of a foreign body in the eyes.
Diagnostics
All types of blepharitis are treated by an ophthalmologist.
Diagnosis includes eye examination and slit lamp examination. In some cases, a biopsy is necessary.
Treatment
Blepharitis is treated comprehensively, using physiotherapy, prescribing medications, and massage.
Drug therapy
The following drugs are used in drug therapy:
- drops to moisturize the mucous membranes of the eyes;
- antibacterial agents (tetracycline or erythromycin ointment);
- hormonal drugs - hormonal drugs (hydrocortisone, gentamicin) are prescribed by a doctor only if antibiotic treatment has not brought the desired result, the duration of treatment is no more than 20 days;
- medications for rapid wound healing - usually the ophthalmologist prescribes solcoseryl gel;
- immunostimulants.
If the patient is identified with concomitant diseases, then therapy is carried out to eliminate them.
Physiotherapy
Physiotherapy is one of the main components in the complex treatment of the disease; it has a restorative, antibacterial effect on the human body.
The following procedures are usually indicated for the patient:
- UPF - this therapy improves blood circulation in the tissues of the eye and eyelids, relieves the inflammatory process;
- Microwave therapy - has a similar effect on the human body as UHF;
- Electrophoresis - to eliminate scaly blepharitis, electrophoresis of penicillin or synthomycin, the area of the eyelids and eyes, through a pad. Then, after 1–2 months, electrophoresis with vitamin B1 and ascorbic acid is prescribed;
- Darsonval - used for mild forms of seborrheic blepharitis. Session duration is 2 minutes.
Massage
For the scaly form of blepharitis, doctors recommend a course of massage not only during the treatment period, but also to prevent and prevent relapses.
Massage speeds up the healing process and improves metabolic processes.
Removing mucus from the eyes
If you experience any unusual discharge from your eyes, you should immediately consult a doctor. This is especially true for those who begin to worry about yellowish lumps of mucus in their eyes.
Severe yellow or white discharge from the eyes often indicates the progression of ocular or non-ophthalmic diseases, which are important to diagnose and treat as quickly as possible. For therapy to be effective, it is important to find out the exact reasons why a mucous white or yellow liquid forms in the corners of the eyes. Self-medication in this case can be harmful, so taking medications at your own discretion is strictly contraindicated.
Mucus in the eyes treatment. Mucus in the eyes causes and treatment
Mucus in the eyes: causes and treatment
Discharge from the eyes is a protective reaction of the body. They come in different colors and consistency. Mucus in the eyes can be temporary or permanent. This should not be ignored; it is necessary to identify the cause of this phenomenon, and then begin the treatment prescribed by the doctor.
Why does mucus occur?
The causes of mucus in the eyes vary. This is usually associated with:
- with eye diseases;
- allergies to cosmetics, eye creams, food;
- severe strain on the visual organs.
White mucus in the eyes occurs when there is excess dust. It accumulates and is removed during sleep. Mucus in the eyes causes discomfort, but timely measures will quickly eliminate it.
Possible ailments
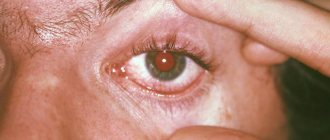
The nature of the mucus in the eyes can determine eye disease. If white discharge periodically occurs in the morning, but there are no symptoms of inflammation, then this is normal. With the regular appearance of mucus and the presence of other complaints, there may be ophthalmological ailments:
- If white mucus comes out of the eyes, this may be a symptom of viral diseases. For example, this happens with viral conjunctivitis. Still white, stretchy mucus is released from the eyes after an acute respiratory viral infection. Redness of the mucous membrane and sclera, lacrimation, photophobia, swelling, and cold symptoms also appear. When the virus occurs, first one visual organ is damaged, and then the second.
- Mucus in the eyes also appears with dry eye syndrome. Dryness and fatigue of the visual organ occur. Appears after long hours of hard work at the computer or with small objects.
- Liquid discharge is considered a symptom of allergies. Usually both eyes are affected. With this phenomenon, severe itching occurs. There is redness of the eyelids and swelling. When the allergen is eliminated, the symptoms subside.
- Liquid transparent discharge occurs from dust and foreign bodies. This is a protective reaction of the body. In this case, it is necessary to remove foreign particles mechanically.
- Yellow, profuse discharge occurs due to inflammation of the lacrimal sac - dacryocystitis. The mucus is thick and abundant. It intensifies when massaging the affected area.
- The appearance of greenish or yellowish foamy discharge is associated with blepharitis - inflammation of the eyelid. This disease causes itching, peeling, and swelling of the eyelids. The discharge is sticky, occurs in the morning, and sticks the eyelashes together. They create dense scales and crusts.
- Thick yellow, green discharge is a symptom of inflammation that appears when white blood cells accumulate. It occurs with bacterial conjunctivitis, viral and fungal infections of the cornea, trachoma, and barley opening. Dense crusts also form, which are difficult to remove. A film appears on the eye, interfering with the clarity of vision. There is redness, swelling, lacrimation, photophobia. In difficult cases, pain in the eyes, headache, and high fever are observed.
- Thread-like discharge appears with filamentous keratitis. This disease occurs when the function of the lacrimal glands is reduced. Dryness, burning, thread-like discharge, and redness of the sclera occur. This causes dystrophic changes in the cornea.
Accompanying symptoms
Considering the main cause of the appearance of eye discharge, the patient may experience additional symptoms consisting of:
- Blurred vision.
- Burning sensation in the eyes.
- Itching in the eyes and eyelids.
- Excessive drying of the mucous membranes.
- Soreness in the eyes.
- Profuse lacrimation.
- Hyperemia of the sclera and skin of the eyelids.
- Photophobia (photophobia) is increased sensitivity of the eyes to light.
- In some cases, eye discharge occurs in parallel with signs of general malaise, fever, coughing and sneezing, body pain, and rhinitis. Similar symptoms are typical for infections of bacterial or viral origin.
Thread-like discharge from the eyes. Diagnosis of the disease that caused the discharge
Depending on the cause of the inflammatory process, discharge from the eyes may have different structures and shades. Based on their appearance, it can be assumed that ailments should be treated. However, the diagnosis must still be made by a doctor, based on examination of the contents and other tests.
What do different discharges from the eyes indicate:
| Structure and shade | Why do they arise? | Additional symptoms | Possible disease |
| Purulent - thick, viscous, yellow-gray, greenish or brownish in color. | Due to the accumulation of leukocytes as a reaction of the body to the activity of pathogenic bacteria. | They form hard crusts that make it difficult to open your eyes in the morning, or a film on the front of the eyeball. | Bacterial conjunctivitis, ocular herpes, trachoma, fungal keratitis. |
| Foamy structure, yellowish or green with the formation of crusts and scales. | The reasons are different: from a reaction to dust mites to infection with pathological microorganisms. | Swelling and itching of the eyelids appear, discharge usually occurs in the morning. | Blepharitis. |
| Mucous white | Due to exposure to viruses. | Redness, increased tearing, first there is discharge from one eye, then the second one joins. | Viral conjunctivitis, colds. |
| Abundant yellow | It is provoked by congestion in the organs of vision. | The component flows out strongly when pressed. | Dacryocystitis. |
| Transparent, liquid | The body's reaction to an irritant from the external environment: pollen, animal hair, etc., as well as severe eye fatigue. | Both eyes are affected at once. They disappear after eliminating the irritating factor. | Allergic conjunctivitis, dry eye syndrome. |
Traditional methods of treatment
If desired, parents can resort to traditional methods of treatment to rid the child’s eye of accumulated purulent formation. Let's look at the most popular methods.
If parents notice that the baby’s eyes are very festering, under no circumstances should they hesitate. It is necessary to do several of the above procedures at home as quickly as possible (for example, use breast milk) and make an appointment with your doctor. After receiving the test results, the factor causing the eyes to fester is identified, and complex treatment can begin.
Even careful care and attention cannot protect children from various diseases. What parents don’t face: colic, constipation, rashes, prickly heat, and the like. Another problem is conjunctivitis, where the child’s eyes fester.
Conjunctivitis is often caused by various microorganisms.
- Among the bacteria that cause illness in a child, streptococci, staphylococci, pneumococci, etc. are observed.
- Viruses include pathogens of herpes, measles, ARVI, influenza, adenoviruses, etc.
- Sometimes there are allergic conjunctivitis - to pollen, dust, animal hair, medications.
- Chlamydia.
White discharge from the eyes in an adult and a child: mucus and pus in the eyes
Tear ducts can secrete liquid contents that appear as mucus in the eyes. The most intense cleansing process occurs during sleep, when external irritants do not act and the muscles are relaxed.
In case of infection, irritation by adverse factors or fatigue, white discharge appears in the corners of the eyes. Usually they are noticed in the morning. Dried crusts on the upper or lower eyelashes cause discomfort.
The mechanism of the appearance of discharge
Regardless of color, any discharge from the eyes occurs for specific reasons. They are divided into internal (endogenous) or external (exogenous). Internal factors indicate a weakened immune system, a general or local inflammatory process. External causes include exposure to eye irritants and pathogenic microorganisms (bacteria, viruses).
The main causes of white eye discharge:
- diseases of the upper respiratory tract (ARVI, influenza, sore throat, sinusitis, otitis media);
- conjunctivitis of bacterial or viral origin;
- infection of the lacrimal canals, mucous membrane of the eyes, cornea (blepharitis, meibomitis of the upper or lower eyelid, keratitis, trachoma, chalazion, dacryocystitis);
- diabetes type 1 or 2;
- contact with allergens (washing products, decorative cosmetics);
- overwork;
- poor quality lenses or improper care of them;
- eye surgery;
- prolonged exposure to direct sunlight;
- anatomical features of the structure of the ocular canal;
- seasonal vitamin deficiency.
Often eye infections spread from one person to another. Therefore, from the very beginning of the onset of unpleasant symptoms, the sick person should be attentive to his belongings, toiletries, and cosmetics.
They need to be washed thoroughly, disinfected if possible, or use disposable products. Otherwise, the risk of infection to the patient’s relatives and friends increases.
Especially if these are infants or small children.
Clinical manifestations of the symptom
Discomfort occurs immediately after an irritant or infection enters the organ of vision. Initially, one eye may be affected; after a short time, discharge appears on both.
Their intensity increases at night when the patient is sleeping. After sleep, the eyes open with difficulty because of the crust that dries on the eyelids. During the day you feel a burning sensation and your eyes turn red.
Tears flow profusely from them, a white or transparent liquid. In advanced cases, purulent clots appear.
White discharge from the eyes is accompanied by the following common symptoms:
- Edema.
- Redness of the whites.
- Accumulation of secret.
- Hyperemia of the area around the eyes.
- Irritation, itching.
- Dry mucous membrane.
- Sensation of sand in the eyes, foreign body.
- Sticky eyelid after sleep.
- Tearing.
- Photophobia.
If the symptom is provoked by an infectious or viral disease, then pus and intoxication additionally develop. It is expressed in a nagging headache, low-grade fever, and general weakness. With diseases of the respiratory tract, the malaise is complicated by nasal congestion, snot appears, and the throat may hurt.
Determining the cause using diagnostic methods
The doctor does this through visual or laboratory examination of the secretion. Each ophthalmological disease will bring its own characteristics to the nature, color, location and structure of the excreted fluid.
When white, stretchy mucus is released from the eyes, a viral effect on the body in general or the eyes in particular can be suspected. Usually, it collects on the inner edge and is localized near the lacrimal canal, the lower eyelid.
First, conjunctivitis affects one eye, then the infection is transferred to the second. Timely treatment of colds and relief of ophthalmic symptoms quickly alleviates the patient’s condition.
Tearfulness, redness or abscess disappear without consequences.
Transparent or whitish discharge indicates an allergic reaction to external irritants. It occurs in the off-season period during active flowering. Mucus is also provoked by pets, whose fur often causes allergies.
The eyeball can become dry due to prolonged stress and prolonged exposure to the monitor. In these cases, both eyes are affected at the same time, and the discharge will be thin.
The doctor diagnoses dry eye syndrome or conjunctivitis of allergic etymology.
Sometimes dysfunction of the glands that produce tears leads to keratitis. This is a type of inflammatory process in the cornea. The discharge is thread-like and white or transparent. Additionally, irritation occurs in the eyes, the mouth and nose dry out. The eyes react sharply to light and water.
The ophthalmologist prescribes general blood and urine tests, the indicators of which will indicate inflammatory processes. This differentiates infectious diseases, for example, of the ear, from allergic reactions on the skin and will help determine the course of treatment.
Serious ophthalmic ailments at an early stage are manifested by white discharge. Their presence in itself does not prove pathology until they begin to fester.
Without treatment, the discharge from the eyes changes color from white to yellow, green, or brown.
Drug therapy
Treatment with medications is aimed at removing and washing away germs, bacteria, as well as eliminating the mucous film and allergic reaction. To do this, use solutions, drops or ointments:
- Antibiotics - Levomycetin, Tobrosopt, erythromycin ointment, Fluconazole solution. Indicated for keratitis, blepharitis, conjunctivitis. They quickly penetrate the blood through the eyes. A small amount of the drug should be instilled directly into the area of the tear ducts or applied to cotton pads. They carefully wet each eye separately from the outer edge to the inner. It is imperative to treat both eyes, regardless of the severity of the symptoms of infection.
- Antiviral - Oftalmoferon, Virgan gel. For the treatment of keratitis and conjunctivitis of any etiology. Used in case of eye infection with herpes simplex virus. Povisep is used as a prophylactic agent before and after ophthalmological operations and is prescribed to newborns.
- Antibacterial - Sulfacyl sodium, Albucid, Oftaquix. The products are released in the form of drops. The active substance effectively copes with strains of microorganisms that cause bacterial conjunctivitis with sticky secretions.
- Antimicrobial - Okodek, Okatsin. Drops help with acute and chronic inflammation of the eyes, to prevent infection in adults and blenorrhea in children. The eyeballs may turn red. Drops are used to treat contact lenses.
- Antihistamines - Allergodil, Opatanol, Cromohexal. Relieves symptoms of allergic conjunctivitis in the acute stage. The drops prevent its development during seasonal exacerbations if the allergen is the smell of flowers or pollen.
It is not recommended to take medications on your own, especially for infants. The same applies to traditional methods. The drug, dosage regimen and duration are prescribed by the doctor after making an accurate diagnosis. Uncontrolled treatment reduces the sensitivity of pathogenic microflora, which develops immunity to the components.
Eye inflammation leads to serious complications, both local and general, and suppuration. In advanced cases, the pupil narrows, vision deteriorates, cataracts and blindness develop.
Discharge in childhood
A child's tear ducts do not develop immediately. Sometimes fluid stagnates in them, or the liquid secretion begins to come out too actively.
In this case, the discharge from the eyes of a newborn may become thick, abundant, and form crusts. This phenomenon is not considered a pathology in infants.
Their eyes should be washed regularly, additionally using disinfectant solutions or drops.
The pediatrician will prescribe medications that are approved for use from birth. Dr. Komarovsky emphasizes that it is important to follow the instructions and not use them for longer than the specified time.
Typically, antibacterial and antimicrobial drops are recommended. They moisten a cotton pad and carefully treat the baby's eye.
Additional symptoms such as redness of the whites, swelling, purulent discharge from the eyes require immediate contact with your pediatrician.
Treatment
Therapeutic tactics involve influencing the source of the problem and the mechanisms of pathology development. Basically, this can be achieved using conservative methods. They cannot do without medications:
- Antiseptics (Albucid, Vitabact).
- Antibiotics (Tsipropharm, Tobrex, tetracycline ointment).
- Non-steroidal anti-inflammatory drugs (Indocollir).
- Antiallergic (Lecrolin, Visallergol).
- Glucocorticoids (hydrocortisone ointment).
When you have a cold, it is important to increase the activity of the body's defenses, for which interferon preparations (Nazoferon), immunomodulators (Anaferon, Polyoxidonium), and vitamins (ascorbic acid) can be used. Dacryocystitis during the period of infiltration is also treated with physiotherapy (UHF therapy, dry heat). And if an abscess forms, surgical methods will have to be used, because the pathological exudate must be removed from the lacrimal sac. This is done by creating an anastomosis between it and the nasal cavity (dacryocystorhinostomy). Currently, the operation is performed minimally invasively (endoscopically or laser).
If there is discharge from the eyes, then the only correct solution is to seek help from a doctor. Only a specialist can understand the cause of the changes and how to eliminate the pathology. And the patient should refuse even the thought of self-medication, and rely on medical recommendations in everything.
Symptoms
Any symptoms require analysis and detail. First, the doctor interviews the patient to identify complaints and find out how the disease began and progressed. When examining discharge from the eyes, one should note their characteristics. The main characteristics of the symptom include:
- Color: white, yellow, greenish.
- Type: mucous, purulent.
- Consistency: liquid, viscous, thick.
- Volume: abundant or scanty.
- Frequency of occurrence: in the morning or throughout the day.
- Provoking factors: rubbing the eyes, pressing on the lacrimal sac.
At the same time, a physical examination is carried out, which includes inspection and palpation. This allows us to establish objective signs of pathology. The complex creates a general picture of the disease, allowing a preliminary conclusion to be made.
If the eyes are running, then diagnosing the problem begins with finding out all the symptoms that are present in the patient.
Conjunctivitis
Inflammation of the conjunctival mucosa is the most common cause of eye discharge. Based on the type of pathology and its origin, the symptoms may have some differences. The most common signs of conjunctivitis are:
- Sensation of a foreign body, cutting.
- Redness of the eye.
- Swelling of the mucous membrane and eyelids.
- Tearing.
With bacterial inflammation, purulent discharge appears, which mainly collects after sleep. Due to the viscous and cloudy secretion, the eyelids stick together and plaque forms on them. First, one eye is affected, but due to poor hygiene, the infection spreads to the second.
Quite often, conjunctivitis appears to be a sign of a general respiratory disease. A viral infection is characterized by signs of general intoxication: fever, weakness, malaise, body aches. A runny nose occurs, and patients are bothered by a sore throat and cough.
Conjunctivitis with adenoviral infection is a sign that allows you to distinguish it from other colds. It can occur immediately or after some time from the beginning. The discharge is often scanty, enlarged follicles are visible on the mucous membrane, and sometimes a filmy coating forms. Inflammatory phenomena in the eye persist even after the temperature normalizes.
Small mucous discharge also appears in the allergic form of conjunctivitis. But in this case, severe redness and swelling of the eyelids, burning and itching in the eyes come to the fore. The addition of secondary bacterial flora leads to suppuration of the exudate, the mucus becomes white-yellow or greenish.
In addition to viral infections, conjunctivitis can be one of the manifestations of Reiter's syndrome. This is a condition caused by chlamydia. It is characterized by damage to the urethra, mucous membrane of the eyes and joints. Conjunctivitis is often combined with keratitis, iridocyclitis, and uveitis. Its manifestations can be scanty, but concomitant urethritis and arthritis are unlikely to go unnoticed.
Blepharitis
When the eyelids become inflamed, viscous fluid may also be released from the eyes. But most often this is observed with demodectic blepharitis, which occurs due to tick-borne infestation. The outer edge of the eyelids itches a lot, especially in the morning, and sometimes the itching becomes almost unbearable. Stinging occurs in the eyes, sticky secretions collect, which stick together the eyelashes, further transforming into scales and crusts. The eyelids thicken and turn red. The disease has a chronic course; demodicosis can also affect other areas of the face: eyebrows, smooth skin.
Dacryocystitis
In cases where sticky fluid flows from the eye, it is necessary to think about a disease such as dacryocystitis. It occurs due to obstruction of the lacrimal canal (with ARVI, rhinosinusitis, nasal polyps, congenital anomalies, after injuries). Tears stagnate in the bag, which leads to the addition of secondary flora and the development of an inflammatory reaction. The secretion turns from transparent to cloudy mucopurulent.
The clinical picture of dacryocystitis is quite typical. The main symptoms of the disease include:
- Severe lacrimation.
- Swelling below the inner corner of the eye.
- When pressed, pathological exudate is released from the lacrimal openings.
The acute process is characterized by more striking signs. The skin turns sharply red, the swelling becomes painful, the eyelids are swollen, and the palpebral fissure does not close completely. Swelling may spread to the cheek and nose. Patients complain of pain in the orbital region, fever and other signs of intoxication. And after a certain time, a fluctuation forms in the center of the swelling, then pus breaks through the fistula outward or into the nasal cavity. The danger is that phlegmon of the orbit may form.
Discharge of pus from the eyes during dacryocystitis is a fairly characteristic sign, which, in combination with other symptoms, suggests a diagnosis.
Pathological discharge from the organs of vision
Discharge from the eyes is a fairly common problem, which often leads to an unpleasant condition manifested by sticking of the eyelids in the morning after waking up. In adults, these discharges may have a different character (in color and consistency), taking into account the root cause of their appearance.
Most often, they appear temporarily, and disappear as unexpectedly as they appeared, after just a couple of days. But there are cases when such problems may indicate the presence of a serious pathology in a person, and he needs help and advice from a specialist.
By themselves, discharge from the eyes represents a specific protective reaction of the body to the influence of various environmental factors. These include: pathogenic microorganisms, allergens, mechanical damage, etc. Most often they indicate eye damage due to some disease.
Diseases that provoke discharge
- Blepharitis is a chronic inflammatory process of the edges of the eyelids, which occurs against the background of infection by Staphylococcus aureus.
- Conjunctivitis is an inflammatory process of the outer membrane of the organ of vision (conjunctiva), which can have different etiologies.
- Ophthalmoherpes.
- Keratitis of fungal etiology.
- Corneal ulcer.
- Dacryocystitis is an inflammatory process in the lacrimal sac, from which green or yellow pus is released.
- Chalazion or Stye.
- Dry eye syndrome is a pathological process that develops due to insufficient tear production.
Often, the cause of pathological discharge from the eye in an adult is infection of an organ that has been weakened after surgery during rehabilitation. Inappropriately sized or dirty contact lenses can also cause this symptom.
In some people, discharge appears after accidental chemical exposure or UV irradiation, as well as due to prolonged work at the computer.
Classification of discharge
Considering the type of infection that caused the development of the inflammatory process, the discharge takes on a different character: purulent (yellowish or green), simply white, transparent, etc. Their presence occurs in the same way in both adults and small children, but the treatment plan in each individual case is prescribed individually.
Purulent inflammation of the eyes manifests itself as yellow or greenish inflammatory substrates protruding in the corners of the organ - pus with a thick consistency.
This symptom is explained by the presence of a huge number of leukocytes (white blood cells), which play a very important role in the human body - they fight pathogenic microorganisms, removing them from the body in the form of pus.
Gluing of the eyelids is considered a common protective reaction of the organs of vision to progressive pathologies, such as conjunctivitis.
- White (mucous) discharge
White or whitish discharge from the eyes, or completely liquid and transparent, does not form crusts and does not stick together the eyelids. They do not bring much trouble to the patient.
The main cause is considered to be a cold, allergies, drying out of the eye membranes or excessive friction of the eyelashes on the eyeball.
Often, discharge of this type disappears as soon as the irritating factor has been eliminated.
In children, in addition to all of the above pathologies, the cause of discharge from the eyes can be a disease called dacryocystitis (an inflammatory process in the lacrimal ducts). Very often it is diagnosed in newborns, due to the anatomical features of the structure of the lacrimal organs.
Accompanying symptoms
Considering the main cause of the appearance of eye discharge, the patient may experience additional symptoms consisting of:
- Blurred vision.
- Burning sensation in the eyes.
- Itching in the eyes and eyelids.
- Excessive drying of the mucous membranes.
- Soreness in the eyes.
- Profuse lacrimation.
- Hyperemia of the sclera and skin of the eyelids.
- Photophobia (photophobia) is increased sensitivity of the eyes to light.
- In some cases, eye discharge occurs in parallel with signs of general malaise, fever, coughing and sneezing, body pain, and rhinitis. Similar symptoms are typical for infections of bacterial or viral origin.
Possible complications
Against the background of pathological discharge from the eyes of an adult, certain complications may arise:
- Decrease in visual acuity up to blindness.
- Further spread of infection throughout the body.
- Corneal damage.
- Dryness or severe itching in the eyes.
- Inability to open eyelids independently in the morning.
Therapeutic measures and prevention
To get rid of discharge, the doctor prescribes certain procedures to the patient, based on the nature of the discharge and the reason that caused it.
Some manipulations need to be carried out in a hospital, while others can be carried out at home.
If the discharge is severe, your doctor may prescribe antibacterial medications in the form of eye drops or oral medications to relieve symptoms.
Methods for eliminating eye discharge at home consist of using a sponge moistened with warm water, which is applied to the eye to soften the sticky eyelids. For women, it is important to promptly remove old eye makeup, which is one of the main causes of eye infection.
Caring for contact lenses, as well as replacing them, should be carried out strictly according to the advice of the attending physician. The lens case also needs to be changed regularly to a newer one. Traces of fat from the eyelids can be washed off very well with baby shampoos or other detergents. Avoid sharing personal hygiene products (towels, washcloths, etc.).
Source: https://zdorovglaz.ru/raznoe/vydeleniya-iz-glaza-u-vzroslogo/