The impetus for writing this article was a tragic incident that occurred not long ago in Moscow: in November 2021, a young woman with two children fell from the window of a nine-story building. The mother and nine-month-old baby died on the spot, and a six-year-old boy in serious condition was taken by ambulance to the hospital's intensive care unit. According to the main version, the cause of the incident was postpartum depression in a young mother.
Diagnosis and treatment of postpartum depression is the responsibility of a psychiatrist. Why is the author of this article an obstetrician-gynecologist? Because often it is the obstetrician-gynecologist who can suspect that the mother is depressed and give recommendations to visit a specialized specialist. And the topic of mental health is stigmatized by our society, so a woman would rather complain about her experiences to her obstetrician-gynecologist than turn to a psychiatrist. This article is aimed not only at mothers and pregnant women, but also at their loved ones, who have a leading role in supporting young mothers.
Postpartum changes
Childbirth is a complex process that requires enormous energy expenditure on the part of the woman. After the birth of a child, global changes occur in the mother’s body (emotional, physical, psychological, hormonal), and this cannot but affect the woman and her relationships with loved ones.
In the postpartum period, a postpartum woman may experience a wide range of irresistible emotions: from excitement, happiness, joy and pleasure to irritability, anxiety, disappointment, confusion, sadness, guilt, tearfulness.
As a rule, negative emotions in a new mother do not arouse the proper attention of loved ones. In modern society, it is not customary to admit the presence of problems, including psychological ones, although sometimes the “special” postpartum mental state becomes so serious that it requires the intervention of specialists.
Currently, it is fashionable to be a “successful mother” who manages to take care of her child and, at the same time, self-development, take care of her appearance, pay attention to her husband, run the household, and at the same time not get tired or complain about life. Therefore, new mothers with psychological problems have a fear of being misunderstood and unaccepted, which makes it difficult to identify women who need help.
Symptoms and signs
The clinical picture of the disease is dominated by signs of a typical depressive episode. These include the following main symptoms that meet the diagnostic criteria of ICD-10:
- Anhedonia – previously pleasant events or activities no longer bring pleasure. In severe cases, a person loses interest in any type of activity.
- Consistently depressed mood.
- Pathologically increased fatigue, including emotional fatigue.
Initially, the mood background may constantly change with episodes of sharp fluctuations in the emotional state. Of course, the episode is not limited to three symptoms. Patients additionally complain about individual disorders that confirm the diagnosis. For example, the emergence of irrational ideas of self-blame or fear, as well as somatic ill-being.
Only a psychiatrist can diagnose the disease, but family members or a local doctor may suspect a problem. Considering the special conditions in which a woman finds herself after the birth of a child, it is not always possible to identify clear criteria that meet the requirements of the International Classification of Diseases (ICD-10). The disease is classified according to sections F3, often supplemented with a second code O99.3.
Among women
The following symptoms of postnatal depression in women occur:
- emotional instability;
- mood is low most of the time;
- spontaneous tearfulness;
- changes in appetite in any form;
- excessive preoccupation with your own child or, conversely, complete loss of interest in him;
- feeling of “loss of strength”;
- sleep disorders - insomnia;
- insomnia;
- outbursts of anger, aggression;
- delusional ideas of guilt, self-abasement;
- pessimism;
- inability to engage in one type of activity for a long time;
- rapid “slipping away” of attention;
- fear of one’s own powerlessness, insolvency;
- increased anxiety;
- panic attacks;
- intentional harm to oneself or a newborn;
- suicide;
- individual somatic symptoms: gastrointestinal disorders, headaches, muscle weakness.
In severe cases, hallucinatory-delusional syndrome occurs. Women cannot adequately care for themselves and their children. In some patients, due to a depressive state, maternal attachment to their own child does not form.
In men
Men can also suffer from depression after the birth of a baby, but not all researchers recognize it as “postpartum.” Neurohumoral changes play a significant role in the development of postnatal mental disorders in women. They are present from the moment of the first menstruation, during pregnancy and lactation.
Symptoms of a depressive episode also meet the ICD-10 criteria, almost no different from those in women. Their appearance among spouses is associated with the following moments:
- Severe depression in a wife who cannot care for a child. The husband begins to blame himself for the problems that have arisen, faced with the need to take care of the baby on his own.
- Social pressure on fathers on maternity leave who are subject to ridicule. Unfortunately, Russian society is still filled with cultural stereotypes. At the same time, men try to hide their anxieties and experiences as much as possible, for fear of appearing weak.
- Lack of correct understanding of what a woman suffered during pregnancy and childbirth. Idealistic expectations are quickly shattered when an unprepared person is faced with the role of a parent.
- The emergence of a crisis in marital relations due to a new addition to the family.
- Individual predisposition to mental illness. The arrival of the baby was the trigger.
However, it is not only mothers who are changing their lifestyle, but also their partners. Increasingly, fathers are taking leave to care for a newborn, since a woman can earn a higher salary. In the European region, the incidence of depressive disorders in men reaches 10-12%.
Postpartum depression
Postpartum (postnatal) depression is the most common mental disorder observed after childbirth. According to official data, the incidence of postpartum depression is about 20%. However, it is believed that the true numbers are much higher due to the fact that often depression is not diagnosed due to the mother's reluctance to disclose information to family members, let alone visit a psychotherapist.
Postpartum depression is a psycho-emotional disorder that occurs in the postpartum period (from several days to six weeks after birth) and is characterized by a pronounced deterioration in mood.
Risk factors for postpartum depression:
- living in an urban area;
- lack of physical activity;
- smoking, drinking alcohol;
- hypovitaminosis of vitamin B6;
- vulnerable personality traits (increased anxiety, perfectionism);
- mental disorders in the past (depression);
- family history of postpartum blues;
- insomnia;
- stressful events during pregnancy;
- first birth;
- surgical delivery (caesarean section);
- traumatic, complicated childbirth;
- complicated course of the postpartum period;
- the birth of a child outside of legal marriage, an unwanted child;
- health problems in the newborn;
- suppressed lactation or inability to feed the baby;
- social isolation, lack of communication with spouse (lack of support);
- having 2 or more children with an age difference of less than 5 years.
What Causes Postpartum Depression?
The reason for these postpartum changes is not entirely clear.
Important! Some of the symptoms that it is associated with and that can cause it or influence its severity include:
- presence of mental disorders in the past,
- presence of mental disorders in close relatives,
- presence of mental disorders, severe stress during pregnancy,
- lack of close relatives or friends who could support you,
- bad relationship with your partner. And it is important how long this relationship lasted before, since this is a serious symptom of general psychological ill-being,
- recent stressful life events such as bereavement,
- the presence of “baby blues”,
- difficult pregnancy and childbirth,
- complications during childbirth, interventions,
- psychologically difficult childbirth and the postpartum period - staff rudeness, cruelty, humiliation, coercion to do something you didn’t want,
Even if you don't have any of these symptoms, having a baby is a life-changing event that can sometimes cause signs of illness.
It often takes time to adjust to becoming a parent. Caring for a baby can be stressful and tiring.
Clinical manifestations of postpartum depression
The main clinical manifestations of postnatal depression are highlighted.
Sleep disorders
A sleep disorder can manifest itself as both insomnia and drowsiness. Usually, mothers and their relatives do not focus attention on such signs, explaining this by the lack of a continuous, full night’s sleep. Changes in sleep are one of the clearest indicators of mental disorder, and they can be both a sign of postpartum depression and its cause. It is important to understand that this is not about the fact that the mother does not have the opportunity to sleep, but that the woman cannot sleep even when this opportunity is available.
Loss of appetite and/or weight change
As with sleep disorders, changes in appetite and weight in a new mother are not emphasized as they may be physiological signs of the postpartum period. However, a weight change of 5% or more in 1 month should alert you.
Depressed mood
Despite the fact that the birth of a baby is a joyful event, mothers without depression can experience sadness. The reasons can be very diverse: fatigue, restriction of freedom, misunderstanding in the relationship with the spouse. However, the hallmark of depressed mood in postpartum depression is that a woman remains in this state for most of the day, regardless of any circumstances.
Loss of interest or inability to enjoy something (anhedonia)
Previous and newly emerged activities and hobbies (housework, hobbies, activities with the baby) do not arouse interest in the mother. Patients’ complaints often sound like this: “I’m tired of everything, I don’t want anything, there’s emptiness inside.”
Psychomotor agitation or lethargy
Psychomotor agitation manifests itself in the form of increased motor and speech (not always) activity.
Feeling tired
Most mothers report fatigue after childbirth, which is associated with an increase in both physical activity and moral responsibility for the baby. We can talk about postpartum depression when a feeling of fatigue occurs after the slightest effort and does not have any dynamics over several days or weeks.
Feelings of worthlessness or guilt, shame, fear
A woman experiences an overwhelming fear of not being able to cope with a newborn; the fear of being left alone with the baby leads to a feeling of shame for her thoughts. The woman feels useless, despite the fact that the mother is the whole world for the baby.
Poor concentration or indecisiveness
Absent-mindedness manifests itself in the form of uncontrolled switching of attention to stimuli, poor concentration, and difficulty switching attention from one process to another.
Suicidal thoughts (or attempts) and recurrent thoughts of death
Thoughts about suicide (and even more so attempts to commit it) are one of the most significant signs of postpartum depression, in the presence of which it is necessary to seek medical help as soon as possible.
The presence of 5 or more of the above signs at the same time is confirmation of postpartum depression.
Every woman experiences any of the above symptoms from time to time. However, we should talk about a depressive disorder when these symptoms change little from day to day and do not depend on circumstances.
How to Avoid Postpartum Depression
Postpartum depression is a disorder of a woman’s psycho-emotional sphere that occurs in the postpartum period and is characterized by a pronounced deterioration in mood. According to statistics, from 10 to 15% of women in labor are susceptible to it. Childbirth leads to global hormonal changes in her body, which often causes emotional disorders. Although there is no proven 100% way to avoid the development of postpartum depression, there are several measures that an expectant mother can take to help reduce the risk of this unpleasant “condition”. Motherhood is not only the responsibility for the baby, which falls on you from the moment of his birth. It is an incomparable pleasure to watch his growth and development, to respond to his love and affection with your love and care. Agree, you don’t want your communication with your long-awaited baby to be overshadowed by anything. And among the symptoms of PDD are the following: • weight loss (or vice versa); • constant sad mood, • desire to cry; • guilt; feeling that you are no longer desirable; • permanent state of anxiety, anxious thoughts; • decreased appetite (or, conversely, constantly hungry); • lack of energy, lack of initiative; • paranoia; • insomnia. Such symptoms are not noticeable to the close people around the woman, and only over time, if postpartum depression worsens and the woman begins to have difficulty communicating with her family, constantly cry, lie in bed for hours and at the same time constantly complain of fatigue, lose interest to the child, it becomes obvious that she needs help. If left untreated, it may be necessary to hospitalize the woman. It is difficult to say for sure whether postpartum depression will occur in you. But it is better to take preventative measures before giving birth to help reduce the likelihood of PPD than to do nothing. Modern scientific research in the field of psychology of motherhood suggests that postpartum depression affects women whose expectations associated with motherhood turned out to be too far from reality. In this case, several key points in a woman’s life are important: expectations related directly to the child; a woman’s expectations related to the help of loved ones (husband, own parents, mother-in-law) in caring for a child; willingness to take responsibility for the newborn, personal maturity of the young mother. As for the expectations associated with the help of loved ones in caring for a newborn, they are often too high for young women. For some reason, immediately after giving birth, young mothers begin to feel that all their loved ones will happily take maximum care of the baby, bathe and swaddle him, feed him, do all the housework, get up to see the baby at night... In reality, in most cases, This doesn't happen. My husband needs to go to work every day and, preferably, get enough sleep. Grandmothers have their own plans for life, their own worries and do not pay all their attention to the young mother and baby. And everyone was so happy about the birth of the baby that the mother got the impression that her child was the common concern of the entire family. This is the biggest illusion. The baby is first and foremost the mother’s concern, and it doesn’t matter whether she’s slept well or not, whether she’s tired or full of energy, whether she’s in a good mood or bad. The baby needs a mother. The rest of the relatives can help with deeds, they can help with words whenever they want, and as much as they themselves consider necessary. The only exception is the father. But his primary concern is to ensure the financial stability of the family, and then support his wife - cook food, do cleaning, iron diapers. All that he manages to do in the interval between the working day and night sleep. So it turns out that in order not to face disappointment and related grievances, a woman, while still pregnant, needs to be determined to rely only on herself and not expect help from anyone. It is worth agreeing in advance with your husband on a specific list of his responsibilities that will be assigned to him in connection with the birth of a child. The list below lists the main family chores - invite your husband to choose from this list those that he is ready to take on, the rest will be yours: cleaning the apartment (house), including washing the floors, vacuuming and dusting; preparing food for the whole next day (in the evening); washing and ironing clothes (both children's and adults); grocery shopping trips; walks with the child (when the weather permits). Responsibilities such as feeding the baby, putting him to bed, swaddling and washing, hygienic care - it is better for the mother to take over, and if your spouse offers you help in these matters, you will get real pleasure and Make sure once again that you have a wonderful and caring husband. It is better not to count or hope for the help of grandmothers from the very beginning, and then when they offer you help themselves, it will be real support and a pleasant surprise for you. The correct distribution of responsibilities between spouses and the absence of unreasonable and inflated expectations from others on the part of the child’s mother is an important point in the prevention of postpartum depression. The readiness to take responsibility for a newborn, the personal maturity of the youngest mother is perhaps the most difficult moment in the prevention of postpartum depression. Unfortunately, the desire to have a child and pregnancy are not signs of a woman’s personal maturity and readiness for responsible parenthood. The more infantile a woman is, cared for by her husband and parents, the less experience she has in overcoming life’s difficulties and solving problems independently, the higher the risk of postpartum depression. After all, with the birth of a child, a woman ceases to be a daughter, she becomes a mother. And if you maintain the daughter’s previous position, it turns out that it is impossible to be a mother in relation to the child. The role of the mother, in this case, is automatically transferred to the grandmother. The grandmother rightly believes that the mother of the newborn is not she, but her daughter. And here fertile soil is already ready for conflicts, mutual reproaches, scandals and postpartum depression. If we summarize everything that has been said above about the psychological causes of postpartum depression, we can highlight the most important point: postpartum depression is the result of the collapse of illusions and hopes. Accordingly, prevention should consist of adjusting expectations. Don't fly into the clouds of desires, falling from there is painful! That is, in order not to become a victim of postpartum depression, a woman, even during pregnancy, should correlate her expectations associated with the birth of a child with the real state of affairs in her family, discuss with her husband and family members the distribution of responsibilities, so as not to feel abandoned later fate. And most importantly, prepare yourself psychologically for the birth of a baby and change your lifestyle, because the prevention of postpartum depression mainly lies in the psychological preparation of a woman for the role of a mother. If, however, prevention did not bring the desired results and it was not possible to avoid depressive symptoms after childbirth, you need to know how to get out of postpartum depression. Mild postpartum depression is treated with supportive conversations and psychological education of the woman and her loved ones. As a rule, having received help from relatives in caring for the baby and the opportunity to devote time to herself, a woman quickly returns to a normal psychological state. For postpartum depression of moderate severity, the use of psychotherapy is indicated. And only in severe cases is it recommended to use antidepressants, the dose of which should be selected individually and adjusted as depressive symptoms weaken.
So how can you reduce your risk of postpartum depression? 1. Find as much information as possible. Learn everything you can about postpartum depression. This will allow you to detect its onset in time to begin taking some measures. Consult your doctor, read books and articles on the Internet. 2. Get enough sleep and eat right A balanced diet and enough sleep are of great importance for your health and well-being. Do your best to eat healthy and get as much sleep as possible—both during pregnancy and postpartum. The best prevention of this condition and treatment of depression that has already begun is proper rest. For example, a baby’s daytime sleep is almost always sound. At this time, you need to forget about all your affairs and plunge into the same serene sleep. Remember: your child’s health is most important, and you still can’t redo all the housework. Shift some of the worries to your husband, mother-in-law, and mother. But always go for walks with your child yourself, especially on weekends. 3. Water has an excellent calming and anti-stress effect. Therefore, get yourself this habit: after putting your child to bed, take a shower or bath with aromatic herbs. Essential oils from lavender, rosemary, chamomile, fir, and sandalwood are good for relaxing, calming and strengthening the nervous system. 4. Don't forget about free time. Even during this stressful period, try to get out of the house for at least an hour, meet a friend, or wander around the shops. Be sure to pamper yourself with shopping, even a pleasant little thing can lift your spirits. Having received psychological relief and positive emotions, you will return to fulfilling your maternal duty with triple strength. 5. Move! Exercise reduces the risk of PPD. Yes, even the simplest ones! Fifteen minutes of walking a day is enough to lift your spirits and feel better. 6. Avoid making any major life changes during pregnancy and immediately after childbirth If possible, do not make important life-changing decisions during pregnancy or after childbirth. For example, decisions about buying an apartment or changing jobs. Try not to let anything throw you off track. Avoiding the stress of making decisions will make your postpartum recovery faster and easier. 7. Don’t keep the reasons for your anxiety to yourself. Don’t be afraid to talk about your needs and voice your wishes when you are in the maternity hospital or postpartum ward of the hospital. It is important that your recovery takes place in comfortable conditions. 8. Prepare for childbirth. It is better if you attend courses for expectant mothers. Read books, magazines, articles (including on the website kirovmama.ru). On forums you can chat with women who have already given birth and learn about their experiences. The information will not be superfluous. It is better to know about all possible options for the course of labor than to experience shock and deep stress on the spot when hearing about a caesarean section. If you know what you can expect, it will be easier for you to bear any development of events. 9 Enlist the help of your family with housework when you and your baby are discharged from the hospital You will find it difficult to cook, clean, and do some household chores in the first few weeks after the birth of your baby, especially if you had a caesarean section. You must be sure that the family and friends around you will help you. Perhaps your mother (mother-in-law, sister, etc.) will move in with you for a while? If this is not possible, perhaps you should think about hiring an assistant? Even if she only comes a couple of times a week to tidy up the apartment, this will greatly ease your situation and relieve you of worry. 10. Find reliable emotional support - and use it. You need someone to lean on when you're upset, annoyed, or even just tired. Have a heart-to-heart talk with someone, tell them about your feelings, about how your life has changed. You will feel much better when you can talk it out.
Postpartum depression in men
Yes, yes, don’t be surprised, let’s talk about this condition from a man’s perspective. Everyone is accustomed to thinking that postpartum depression occurs only in women, but it has long been proven that one in four men is susceptible to falling into this state. How does it appear and why? What to do if you notice this condition in your spouse? Well, firstly, it can manifest itself in different ways, although the most common symptoms are fatigue, apathy, insomnia, irritability, and isolation. Some men give up their previous hobbies, justifying this by the fact that they are “just tired of it.” The reasons for the appearance of such a mood in men are also different. Some begin to show their selfishness. The husband understands that you have stopped paying attention only to him, and if he seemed to be ready for this during pregnancy, now he knows it more clearly. Now he needs to grow up, and he is not ready for this. There is also another type of young fathers who, on the contrary, become hyper-responsible. This condition can become no less stressful than the previous one. The man worries about the financial side of the issue. He is worried that, as it seems to him, he earns little to provide for the baby, or is rarely at home and cannot pay him due attention. Not all young fathers experience these experiences into depression; many recover from their anxious state quite quickly. But if your spouse has been in a depressed mood for more than two weeks, withdrawn, or something else in his behavior makes you think, then you should sound the alarm. Of course, the most effective way out of depression for both men and women is psychotherapy. But it’s unlikely that any of our young dads will openly declare
"Baby Blues"
The presence of emotional disturbances in the postpartum period is characteristic not only of depression, but also of some other conditions.
First of all, such conditions include “baby blues” (postpartum blues, postpartum melancholy), which is a phase of emotional lability after childbirth with frequent bouts of crying, irritability, confusion and anxiety.
“Baby blues” occurs in 70-80% of new mothers and resolves on its own within a few weeks.
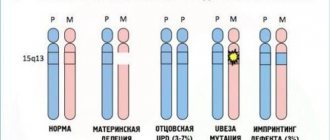
The cause of this condition is physiological changes in the woman’s body. After childbirth, there is a sharp decrease in progesterone and estrogen levels, and this affects the production of serotonin and dopamine, which are responsible for positive emotions.
Symptoms of baby blues occur during the first 10 days after birth, reaching their maximum by day 5.
Typically, symptoms of postpartum blues do not affect the ability to care for the baby and the social functioning of mothers. Baby blues are not pathological and do not require active intervention other than support from family members. However, baby blues that persist for more than two weeks can contribute to the development of more severe forms of mood disorders.
Myths about postpartum depression
This disease is often misunderstood and superficial by society, and there are many myths surrounding it.
These include:
- Postpartum depression is less severe than other types - in fact, it is just as serious, and perhaps more so, given that it affects not only the mother, but also the child.
- Postpartum depression is entirely caused by hormonal changes - in fact, it is caused by many different factors.
- Postnatal depression will go away on its own - unlike the baby blues, postnatal depression can persist for several months and get worse, and if left untreated, it can become a long-term problem - chronic depression.
- Postpartum depression only affects women - studies have actually shown that on average 1 in 10 new fathers become depressed after having a baby.
Depression as a consequence of somatic diseases
Changes in the emotional sphere are also characteristic of some somatic diseases. Among the variety of diseases accompanied by emotional disorders, thyroid pathology and iron deficiency anemia are the most common in the postpartum period.
Hypothyroidism, characterized by a decrease in the level of thyroid hormones, may be accompanied by lethargy, decreased mood, lethargy, drowsiness, deterioration of memory and intelligence.
On the contrary, hyperthyroidism and, accordingly, high levels of thyroid hormones are characterized by the opposite symptoms: psychomotor agitation, fussiness, mood swings with a rapid transition from laughter to crying.
A decrease in hemoglobin levels, characteristic of iron deficiency anemia, leads to symptoms such as weakness, drowsiness, and lethargy.
Taking certain medications, such as methyldopa, nifedipine, interferon, can also affect the emotional state.
Symptoms of depression
- Your eyes are constantly wet - you cry with or without reason.
- A baby's cry sends you into a fit of rage. You are ready to do anything to make this little tyrant finally shut up.
- You have a strong feeling that all your relatives are watching your every move, and are just waiting for you to do something wrong - then they will have every right to teach you about life.
- You feel absolutely helpless in the face of circumstances. You have nowhere to hide, no one can help you, protect you and take on the burden of maternal care. I’m scared for myself and even more scared for my child. At the same time, you do not experience any joy while caring for your baby, although you regularly follow all the doctor’s instructions. Yes, you gave birth to this baby, but he is still a stranger to you.
- You are afraid of breaking down every minute, so you try to take care of yourself as strictly as possible. But it’s as if some kind of spring is being compressed inside you, stronger and stronger.
- Sex makes you feel deeply disgusted.
- I don’t even want to go to the mirror again. Throughout your pregnancy, you dreamed that after giving birth you would again become slim and light, but reality turned out to be too harsh for you. The tightest jeans still lie on the far shelf, and you have to be content with wide robes, like in the sixth month. Your own appearance annoys you.
Postpartum depression does not necessarily include all the symptoms described, but if you have at least four of them, this is a reason to seriously think about it.
Treatment
Psychotherapy and antidepressants are used to treat postpartum depression. In patients suffering from mild to moderate depressive disorders, without psychotic symptoms and suicidal tendencies, psychotherapy is used. In more severe cases, medications are prescribed.
Don't be afraid to seek help from a psychiatrist!
First of all, it is completely confidential. Secondly, postpartum depression is not a socially dangerous disease. Third, women worry that they will have to stop breastfeeding due to taking antidepressants, but currently most drugs used in this situation are approved for breastfeeding.
An important point is the choice of a competent psychiatrist who respects the mother’s desire not to interrupt breastfeeding. Fear of dependence on antidepressants also stops women from turning to a psychiatrist. Antidepressants do not cause addiction, many of them have a cumulative effect, treatment continues for a certain course with further gradual withdrawal.
How to cope with postpartum depression
It has been noted that depression can last 6-7 months after childbirth and then go away on its own as the woman gets used to the new role and begins to cope better with her responsibilities and improves her relationship with her husband. By this time, infant colic usually goes away, the baby sleeps better, and the mother has learned to understand his needs.
However, postnatal depression can be prolonged, especially if there is no outside support. Therefore, the best solution is to contact a specialist - a psychiatrist or neurologist. Often, only psychotherapy sessions will be enough to improve the condition. In severe cases, it is necessary to take antidepressants. There are medications that are approved for breastfeeding. If a woman wants to maintain lactation, the specialist is obliged to meet her halfway also because breastfeeding improves the psychological connection between mother and child, helping her cope with stress.
If a visit to the doctor is not possible
There are times when a new mother does not have the opportunity to visit a specialist: if the mother is raising a child alone, there are no relatives, or the husband is on a long business trip.
In such cases, you can try to help yourself by following the following recommendations.
Try to get enough sleep
Go to bed every time the child sleeps, ensure co-sleeping and put off household chores (a dirty floor has never made anyone depressed).
Put your baby to your breast more often
During feeding, the hormone oxytocin is produced, which increases the feeling of attachment to the baby.
Think more often about your child’s love for you
Think that your baby has all-encompassing unconditional love for you, and that all difficulties are temporary, and will soon become easier.
Treat yourself to your favorite foods
It has been proven that a nursing mother does not need to follow a strict diet; it is enough to improve her diet.
And:
- walk more in the fresh air;
- organize your day;
- get rid of multitasking, it's exhausting;
- build a hierarchy of things to do with your child and focus only on the most important ones;
- find ways to boost your self-esteem as a mother;
- Don’t try to be a “perfect” mom;
- share your experiences with those who can accept them (friend, online acquaintance, neighbor);
- communicate with other mothers, including those with similar problems (in relevant online communities);
- do not refuse help;
- consult with a specialist online.
However, all of the above measures can only help with subdepressive conditions or mild depression. In moderate and severe cases, it is impossible to cope without a specialist.
How to overcome postpartum depression
As with many other medical problems, the best treatment is prevention. Specialists from the Moscow Service for Psychological Assistance to the Population have developed a recommended set of measures that will help reduce the likelihood of postpartum depression [A. Khvatskaya, 2020].
Measures to prevent postpartum depression:
- Attend childbirth preparation classes.
- Provide feasible physical activity during pregnancy.
- Avoid perfectionism and don’t think that you need to be a perfect mother.
- Form realistic expectations from life.
- Form trusting relationships in the family.
- Resolve social and domestic issues before the birth of the child.
- Plan your day in advance so that you have the opportunity to rest.
Psychologists note that for women who are forced to spend a significant part of the day alone with their child, the risk of postpartum depression is much higher than if the young mother is actively helped by her husband or nanny [A. Khvatskaya, 2020]. If for some reason the full cycle of prevention failed and now there is a suspicion that the “delights” of postpartum depression are already a reality, it is worth undergoing self-diagnosis.
The main diagnostic method is the 10-question Edinburgh Postnatal Depression Scale, developed by scientists from Scotland in 1987. Since then, enormous positive experience has been accumulated in the use of the Edinburgh scale, including among Russian women [M. Shamanina, G. Mazo, 2015]. This diagnostic method takes 5-7 minutes and allows you to make a reliable express assessment of a woman’s psychological state.
There are also domestic developments in this area. In particular, the test “Do you have postpartum depression?”, authored by psychologist Natalya Oreshkina. The questions cover all aspects of the phenomenon of postpartum depression: the scale contains 48 questions, the answers to which provide a comprehensive picture of the woman’s condition.
If the test results confirm the risk of postpartum depression, it is better to schedule a visit to a psychologist or psychotherapist in the near future. Perhaps the young mother will be helped by traditional forms of psychotherapy: family, cognitive, interpersonal, therapy for taking responsibility.
If depression has affected not only the psychological, but also the physical condition of the mother, the help of a doctor will be required. We have already mentioned many times that postpartum depression may require medication. Therefore, we remind you that self-medication is dangerous to health, and only a person with a medical diploma should carry out a full diagnosis and prescribe medications.
That is why we will not give any names of medications, recipes, or folk remedies here. In such a matter as depression (any kind!) it is very easy to do harm with recommendations without taking into account diagnostic data and the condition of a particular patient. For the same reason, we will not talk about how various drugs affect the ability to breastfeed. This depends on the prescribed drug and the woman’s condition, so you should focus solely on the doctor’s individual recommendations.
However, any woman who has just given birth can do something for herself on her own. Psychotherapist Darina Sorokina has developed a set of measures that you can try to implement in your daily life [T. Koryakina, 2020].
How a new mother can take care of herself:
- Avoid isolation - think through the possibilities of communicating with friends and relatives, ask them to call you regularly and contact you via instant messengers. If your region has a relatively favorable epidemiological situation, do not refuse personal communication while maintaining social distance and other precautions.
- Eat right - give up the temptation to “eat up” stress with sweets and “wash it down” with liters of coffee. Be sure to eat foods rich in vitamins (vegetables, fruits). If there are no health contraindications, it is better to form a complete diet with a reasonable balance of meat, fish, and vegetable dishes.
- Spending time in the fresh air more often is important for both mother and baby, because oxygen saturation of the body depends on it.
- Exposure to the sun more often - if the birth occurred in the summer season, this is an excellent opportunity to regularly sunbathe with your baby, taking precautions. Sunscreen and limited time in the sun are required for your baby.
- Move more - ideally, it is better to resume training at the fitness center as soon as your health allows. The minimum task is morning exercises, evening stretching and daily walking.
- Get more rest - even though the baby wakes up regularly, try to “get” the required 8 hours of sleep during the day.
- Remember your hobbies or start a new hobby - embroidery, knitting, photography, video editing, yoga, cycling, skiing. It is optimal if the hobby is related to physical activity. Let's say you're walking in a picturesque park to find beautiful frames for photos.
From our editors, we would like to add that completing our “Mental Self-Regulation” program, which will teach you how to take control of your psychological state, can be very effective. But what I would like to say separately is the need to be prepared for the currently very aggressive attitude of the Russian average person towards any psychological problems and the interpretation of them as requiring a solution.
It is difficult to find a forum or discussion dedicated to postpartum depression where victims are not doused with tons of slop or, at a minimum, are not indignant at the “far-fetchedness” of the problem. Thus, at the height of the 21st century, many consider postpartum depression “a Western nonsense that has nothing to do with Russia”, which “develops from idleness”, and advise “not to breed under maternity capital” and remember “the 19th century, when women gave birth in the field.” For some reason, it is not recommended to remember the nuance that only a few of those born in the “field” survived.
Why does such an uncivilized attitude towards the topic of postpartum depression flourish in our society? Here it is worth recalling the previously cited statistics that today, depending on the diagnostic criteria, from 0.5% to 61% of women who recently gave birth can be considered victims of postpartum depression [Yu. Dudkina, 2019]. In other words, at least 39% of the female population have no idea what postpartum depression is, or do not attribute the difficulties that spoiled their mood immediately after childbirth to a state of depression.
The advice to “pull yourself together and cope with all difficulties” is, of course, relevant, but resisting the transformation of the TTC9B and HP1BP3 genes does not always help. To understand that postpartum psychological processes proceed differently for everyone, you need a certain level of culture and education, which is steadily falling as the availability of free higher education decreases. And in order to simply sympathize with a woman in a difficult situation, you need a certain human potential and warmth, which is in short supply these days.
Therefore, the problem of postpartum depression is, in today’s realities, a problem exclusively of the woman herself and her immediate environment. That is why it is so important to provide the young mother with full support and refrain from any critical comments, ranging from excess weight gained to regrets about the gender of the child born.
Comments like “they wanted a girl, but a boy was born” will not change anything, but will once again spoil the woman’s mood and increase the risk of developing a severe form of postpartum depression. Here are the recommendations of psychotherapist Darina Sorokina for families in which a newborn has just appeared [T. Koryakina, 2020].
Recommendations for family members:
- Provide emotional support and show empathy towards the young mother.
- Take on some of the household chores so that the young mother can rest more often.
- Free up a few hours a day for the young mother, which she can spend on herself at her own discretion (sleep, rest, hairdresser).
- To give the young mother confidence that when she is resting, the child is under supervision and in good hands.
- If possible, support the young mother in her endeavors (hobbies, leisure, communication).
- Refrain from arguments and conflicts both with a woman who has just given birth, and simply in her presence.
- If possible, take turns getting up at night with the child (so that not only the young mother does this).
- Try to make the young mother feel that she is still loved, beautiful and charming as a woman, and not just as a mother.
If you follow all the recommendations given, the likelihood of postpartum depression will be much less, and it will pass faster and easier. And finally, the conversation about postpartum depression in men announced at the beginning of the article. Yes, this happens, and special research by American scientists has been devoted to this.
Help from loved ones is like medicine
Family plays an important role in the life of every person. Close people can both help a mother with a newborn and aggravate emotional problems. How many modern young mothers have heard the following words from women of the older generation: “How did we live before? Three children, a household, could only dream of a multicooker, an automatic washing machine and a robotic vacuum cleaner. And nothing, they coped and didn’t complain.”
If a new mother complains that she is tired, wants to sleep and doesn’t have time to do anything, there is no need to think (let alone tell her) that this is due to laziness and selfishness.
Postpartum depression is a disease. Care, understanding and support from loved ones will help women with similar disorders overcome this illness.
So, if you notice changes in behavior in your wife, daughter, sister, who recently became a mother, that correspond to any of the above signs of postpartum depression, then take part:
- let your mother know that you understand her condition and are ready to help;
- listen to her experiences and support her;
- have confidential conversations;
- be careful and patient;
- provide mom with free time (for example, a walk with the baby) so that she can relax, take a leisurely bath or do something that will bring her pleasure;
- arrange help with household chores (cook food, wash the floor, go to the store);
- do not criticize, educate or make harsh comments;
- advise you to contact a specialist.
Postpartum depression: how long does it last?
So how long does postpartum depression last? Everything here is very individual and largely depends on both the form of depression and the typological characteristics of the woman. Women 20-30 years old who are optimistic and prosperous in material and family terms will experience this condition faster and easier than infantile individuals who gave birth out of wedlock and have barely reached adulthood.
In the most general terms, it is customary to distinguish between the so-called “transistor depression”, called by the beautiful name “baby blues”, and postpartum depression itself in severe form [J. Moldenhauer, 2020]. The very first guideline to distinguish one from the other is the time of onset of depression.
Transient depression vs Severe postpartum depression:
- Transistor depression - begins during the first week after birth and lasts a maximum of 2 weeks.
- Severe postpartum depression - begins a month after birth or later, lasts more than two weeks, in especially advanced cases up to 2 years.
In other words, how postpartum depression will proceed, how long it will last and whether it can go away on its own depends on many factors. Mild forms may well go away on their own in a couple of weeks with a favorable home atmosphere and the support of loved ones. It is important for a young mother not to be shy about asking for help with household chores, child care, and sharing her experiences with loved ones.
It is equally important to build a trusting relationship with your partner and the child’s father, then his support will have a real psychotherapeutic effect. This is emphasized by the author of the book “What are baby blues and how to cope with them in the first months of motherhood” [D. Mogilnikova, 2018]. Severe forms require the intervention of a psychotherapist and, possibly, drug treatment. This is worth talking about in more detail.
Prevention of postpartum depression
- Rejection of bad habits.
- Birth control (number of children, interval between births).
- Pregnancy planning.
- Adequate physical activity during pregnancy and after birth (as soon as the mother's health allows).
- Normalization of nutrition, additional intake of vitamin and mineral complexes for pregnant and nursing mothers.
- Attending courses for expectant mothers, which will allow you to learn self-regulation techniques and prepare for life changes.
- Normalization of sleep (increasing the time of night sleep, daytime sleep while the baby is sleeping).
- Use of epidural anesthesia during childbirth. Despite the fact that childbirth is a physiological process, this process is often accompanied by significant pain. It has now been proven that the use of epidural anesthesia during childbirth reduces the risk of postnatal depression.
- Breastfeeding helps improve the quality of sleep in the mother and, as a result, reduces the likelihood of developing postpartum depression. A significant connection has been proven between artificial feeding of a child, sleep disturbances and the likelihood of developing depression after childbirth and its severity in the mother.
- Family support. It is impossible to overestimate the role of the family for breastfeeding women. The opportunity to share experiences with loved ones, as well as their help with the child and at home, reduces the likelihood of the mother developing postpartum depression.
- Normalization of relations with your spouse.
- Socialization (communication with other mothers on forums, playgrounds, clubs).
Postpartum depression in men
Yes, this happens too. The main reasons for this condition in fathers are considered to be lack of sleep, difficulties in understanding their new role, and postpartum depression in their wives. Compounding the problem are social attitudes that effectively prohibit men from talking about their emotional problems. But it is necessary and important to talk about the problem, ask for help from friends and relatives. And if it doesn’t get any easier, go together to a specialist. Otherwise, the brain will find another solution to the problem - divorce, betrayal or alcohol.
Clinical case
Since I am an obstetrician-gynecologist, in my daily practice I have not had to treat women with postpartum depression. However, I had the opportunity to take part in the fate of such patients. The result of Olga’s pregnancy is the birth of a long-awaited, long-suffering and desired daughter as a result of IVF, 8 years from the start of her planning. The pregnancy proceeded without complications. The birth was long and traumatic.
From Olga's story:
“My daughter is already 2 months old, but I have not been overwhelmed with the all-encompassing love for her that I was waiting for. Instead of joy and a feeling of my life being filled with new meaning, I cry every day and feel empty. I am very ashamed of my emotions, I feel sorry for both myself and the baby. The thought that I will never have that past life again, that I no longer belong to myself, that my whole life is subordinate to a little man, depresses me even more. I stopped making plans and dreaming. I have a hard time coping with the endless swaddling, washing and feeding. When I tried to complain to my sister, I heard that being a mother is hard work. No one around me warned me that breastfeeding is very difficult and needs to be prepared for it in advance. And here is the result: lactostasis, temperature, pain. I want to fall asleep and not wake up.”
This is the monologue I heard from Olga when she addressed the problem of lactostasis. Having listened carefully to her, stopping the manifestations of milk stagnation, she explained to Olga what was happening to her emotional state. I told the patient about postpartum depression and that she should not be afraid to visit a psychotherapist. Olga turned to the recommended doctor. In her case, it was enough to use psychotherapy, which lasted about 3 months. All this time I kept in touch with Olga and I know that breastfeeding was established, her emotional state was stabilized, Olga learned to plan her day and not forget about herself. Now Olga is a happy mother of a wonderful baby.
Forms of how postpartum depression is expressed
Not all mothers in labor feel the same. Our bodies are unique, and therefore their manifestations are different.
Neurotic depressive disorder
This type occurs in those mothers who, to some extent, had signs of the disease already during pregnancy. Exacerbations occur due to severe hormonal stress. The above symptoms may include:
- aggression;
- dissatisfaction with sex life, lack of desire;
- increased sweating;
- poor appetite.
Postpartum psychosis
The main features of this state are a constant feeling of guilt and the need to justify oneself, along with loss of orientation and some lethargy. If the stage is advanced, suicidal thoughts appear: “I am bad and cannot be a good mother and wife.” This is not the most common form; fortunately, it is rare.
What is prolonged postpartum depression?
Every second woman in labor suffers from it, but due to the fact that the symptoms are “masked” as ordinary everyday problems associated with the birth of a baby, it is difficult to identify.
Blues is the first stage; it can appear already in the maternity hospital, and then worsen when you get home. Common signs are irritability and tearfulness, and feelings of guilt. The duration of the condition is up to 10-12 months without assistance.
Who is prone to the disease:
- Women who are very worried by nature are afraid of doing something wrong, as well as girls with low self-esteem.
- Those who did not receive enough maternal warmth in childhood, and therefore want to give the maximum to their child.
Why is postpartum depression dangerous?
Postpartum depression can lead to disruption of the relationship between mother and child, refusal of breastfeeding, family discord, and disruption of the physical and psychological development of the child.
Children of mothers who have not treated depression may develop behavioral and emotional problems: delayed speech development, sleep disorders, eating problems, attention deficit, hyperactivity.
One of the goals of this article is to support women and inform their environment about everything related to the postpartum period in general and breastfeeding in particular, about possible problems and ways to solve them. Timely identification of mothers in need of support and provision of adequate assistance are key factors for happy motherhood. Sometimes help is very close.
Postpartum depression and antidepressants
In cases of moderate or severe postpartum depression, doctors recommend taking antidepressants. If a woman is against taking medications, then you can replace them with psychotherapy. If she has nothing against it, then you should think about stopping breastfeeding.
It has been established that approximately 3-10% of the daily dose of antidepressants taken by the mother passes into breast milk. In infants under one year old, the liver cannot yet cope with medicinal substances, so a fairly large amount of medicine is retained in the child’s body.
Studies show that at 12-18 months, children whose mothers took antidepressants and continued to breastfeed experienced developmental delays. However, it is worth weighing the pros and cons, because sometimes it is better for the mother to get rid of depression faster than to continue breastfeeding.