Cryptorchidism (undescended testicles) - in pediatric urology, is the most common congenital anomaly, characterized by the absence of one or both testicles in the scrotum at the time of birth in a boy, which occurs as a result of the testicle stopping at any stage of descent along the inguinal canal from the retroperitoneal space.
In full-term newborns, cryptorchidism is found in 3.4% of cases, and in premature newborns - in 30%. In adult men, the prevalence of cryptorchidism is 0.7-0.8%. During the first 6 months of life, 75% of children born with cryptorchidism experience spontaneous testicular descent, probably due to a gradual increase in testosterone levels. By the end of the 1st year of life, cryptorchidism persists in only 1% of boys. In the future, in the absence of medical assistance, the likelihood of spontaneous descent of the testicles into the scrotum is unlikely.
There are false and true cryptorchidism. With false cryptorchidism (migrating testicle), under the influence of muscle tension or cold, the testicle can move into the inguinal canal or abdominal cavity. False cryptorchidism occurs in 25-50% of all cases. It is characterized by symmetry and normal development of the scrotum; migration of the testicle to the area of the inguinal ring or the lower third of the inguinal canal; the possibility of unhindered descent of the testicle into the scrotum during palpation or its spontaneous descent under the influence of heat or in a relaxed, calm state of the child. Testicular migration is a variant of the physiological norm and is explained by the small diameter of the testicle compared to the diameter of the external inguinal ring. Therefore, when the corresponding muscles contract, the testicle is easily pulled up to the inguinal fold.
False cryptorchidism does not require treatment and disappears on its own at puberty.
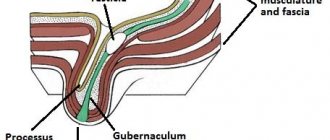
True cryptorchidism is said to occur when it is impossible to manually lower the testicle into the scrotum. In this case, the testicle is most often located in the inguinal ring (40%), in the inguinal canal (20%), and abdominal cavity (10%).
Causes
Most often, the disease is detected in boys immediately after birth. The main cause of cryptorchidism is abnormal development of the fetus in the womb. Factors contributing to the occurrence of an anomaly may be:
- chromosomal and hormonal abnormalities in mother and fetus
- taking drugs prohibited by a woman during pregnancy
- viral infections in the mother
In rare cases, parents ignore the disease in their child. If the boy is not treated in a timely manner, he will independently turn to specialists for help as a man. In adult men, the disease is diagnosed extremely rarely. The causes of pathology are mechanical damage. Thus, the phenomenon can occur against the background of prolonged wearing of medical bandages and corsets after removal of an inguinal hernia. In this case, both testes are pushed into the inguinal canal and cannot move into the scrotum on their own. The patient is experiencing severe pain, so even before the scheduled time to remove the bandage, he goes to the clinic. Men who have suffered injuries to the groin area may face a similar problem.
Undescended Testicle: An Overview of the Disease
Undescended testicle - what is it?
testicles begin to develop while he is still in the womb. Initially they are located in the baby's stomach. Normally, before the baby is born, the testicles descend into the scrotum , a sac that is located under the penis. If this does not happen, the boy is diagnosed with an undescended testicle . In rare cases, both testicles fail to descend.
| Testicles These are two oval-shaped organs in the male body that produce seminal fluid and the male hormone testosterone. They are located in the scrotum, a sac that lies under the base of the penis. Scrotum It resembles the shape of a pouch located under the base of the penis. It contains the testicles (two oval-shaped organs), which produce seminal fluid and the male hormone testosterone. Undescended testicle In most cases, the testicles, which form in the abdominal cavity of a male fetus, descend into the scrotum when the child is born. An undescended testicle (orchipexy) is one that remains where it forms and does not move into the scrotum. Either one or both organs may be affected. This defect is characterized depending on its location and palpation (palpable or impalpable testicles).
|
5 out of 100 newborn boys have this defect. This usually applies to premature babies or those whose birth weight was the minimum acceptable. One of the causes of the disease is a hereditary factor.
In most cases, the testicles still descend on their own within 3 months after the baby is born. If this does not happen before 6 months, the attending physician prescribes appropriate treatment.
Undescended testicle - symptoms
This defect does not cause any pain or symptoms. The scrotum may be less convex or not fully developed on one side, or the part that does not contain a testicle will be smaller and flatter.
Undescended testicle - disease recognition system
During medical examinations of a newborn and growing baby, a specialist will check how the scrotum is developing.
- If the testicle is palpable but not in the scrotum, the doctor will examine the child from 3 to 6 months. During this period of time, the testicle should drop into place on its own.
- Sometimes the doctor is unable to feel the testicle at all. It may still be in your baby's belly, too small to feel, or may not be there at all. After following a wait-and-see approach, your doctor will recommend a procedure called laparoscopy (a diagnostic examination of the abdomen and internal organs) to check where the testicle is located. To perform this procedure, you need to make a small incision under the navel, which heals quite quickly. During laparoscopy, the doctor inserts a small light-emitting device into the baby's abdomen and can use it to help the testicle move into the scrotum. After this, in most cases the child does not require additional surgical intervention.
- If both testicles are not descended and cannot be felt in the groin area, the doctor will do a blood test to measure the amount of hormones to determine whether the baby has testicles. It is very rare for boys to have both testicles missing.
ultrasound to find an undescended testicle . These tests are more effective at diagnosing older boys and men than children.
| Laparoscopy This is a surgical procedure in which a lighted viewing device (laparoscope) is inserted into your baby's lower abdomen through a small incision made under the belly button. Using a needle attached to the end of the device, the abdominal cavity is filled with gas, causing the walls to move away from the organs, and the doctor can examine everything in detail. Laparoscopy is used both for diagnosis and for therapeutic purposes. The cuts are made in such a way that devices, such as mechanical devices or lasers, can be used to correct the problems. With this procedure, the doctor determines which organs are affected, takes tissue samples for a biopsy, and removes the abnormal growths. Laparoscopy allows the patient to avoid open surgery, compared to which it is safer, leaves an almost invisible scar and requires less time for the rehabilitation period. This procedure is also often used to diagnose and treat diseases of the female reproductive organs, such as endometriosis, infertility, ectopic pregnancy, or tubal ligation (sterilization). Laparoscopy is used to treat both men and women, for example, to remove the gallbladder. Ultrasound This is a test that uses reflected sound waves to produce an image of a person's internal organs. This procedure does not involve exposure to x-rays or other types of radiation. Before starting ultrasound, gel or oil is applied to the patient’s skin to make the device glide smoother. After this, the doctor begins to move the transmitter along the area that is being examined. The device gradually transmits high-frequency sound waves (a person is not able to perceive them by ear), which subsequently pass through it again. The computer analyzes the received signal and transforms it into a picture displayed on the screen. This image is called an echogram or ultrasound scan. If necessary, it is entered into the registration book. Ultrasound is the most effective way to study both homogeneous organs (liver) and those that have a liquid composition (bladder). However, bones and lungs are not clearly visible on ultrasound. |
There are diseases similar in development to undescended testicles. Therefore, your attending physician will conduct a thorough examination to establish an accurate diagnosis for your baby and prescribe appropriate treatment.
What is the treatment?
Doctors usually recommend taking a “wait and see” approach as your baby grows older. If the testicle has not descended during the first year of the child’s life, the specialist advises to perform an operation, as a result of which the testicle will be in the scrotum. It is done when the child is 9-15 months old. In most cases, the procedure takes about an hour. The baby is given medicine and he falls asleep, and after the operation he is monitored for some time and if everything is fine, he is sent home. Complete recovery soon follows.
When a boy’s testicle cannot be felt (it is not palpable), the doctor uses a surgical treatment method (laparoscopy).
Sometimes the child is given hormones before surgery to see if they help the testicle descend into the scrotum. However, studies have shown that such hormonal therapy is not effective and may cause side effects. It is mainly used if the testicle is already close to the scrotum.
Undescended testicle - why treatment should not be neglected?
Treatment of this defect is very important, since its presence increases the risk of:
- Infertility . Being in the scrotum cools the testicles, which helps them produce sperm. If they remain in the abdomen, the temperature for seminal fluid production is not low enough and this process is inhibited. Thus, a man may develop infertility in the future. The detrimental effect on sperm production in the body begins when the boy is 12 months old. That is why doctors recommend treating this defect in a child up to one year and no later than 2 years.
- Testicular cancer . Although rare, this disease is the most common form of cancer in men aged 20 to 34 years. If you have an undescended testicle, you are at risk of developing the above disease. However, testicular cancer is curable, especially if it is diagnosed early. By treating an undescended testicle, you increase the chance of detecting this disease in time. If you are young and are faced with the problem of an undescended testicle, seek advice from a specialist. More detailed information on this issue can be obtained in the section “Medical examination or examination of your body if you have an undescended testicle.”
| Infertility This is a diagnosis that is made if a couple is unable to have a child within a year after stopping the use of contraception. Among the most common causes of infertility are irregular sexual intercourse between partners, problems with ovulation in women and the production of seminal fluid and ejaculation in men, diseases associated with damage to the fallopian tubes and uterus. However, sometimes there are also cases of unexplained infertility. Testicular cancer This disease develops when cells in the testicles with an abnormal structure begin to progressively divide. Although testicular cancer is a rare disease, it is the most common type of cancer in men aged 20-34 years. In addition, it responds well to treatment, especially if diagnosed at an early stage of development. The testicles are two male reproductive organs (glands) that produce and store seminal fluid. They also produce the male hormone testosterone. These formations are located in a pouch located under the penis (scrotum). Symptoms of testicular cancer include painless changes in the size and shape of one or both testicles and a feeling of heaviness in the scrotum. There may also be a dull pain in the lower back, abdomen or groin. Testicular cancer is considered the most common disease among Caucasian men and is rare among men of African American and African descent. |
Symptoms
As a rule, a qualified doctor can already discern signs of cryptorchidism in a patient by the appearance of the genital organs. Symptoms of the disease in men 1. External changes in the scrotum. Asymmetry and underdevelopment of the scrotum is revealed by palpation; 2. Nagging pain in the lower abdomen. Causes particular discomfort in the patient during coughing, sexual arousal, and defecation; 3. Deterioration in the quality and quantitative parameters of sperm. The number of active sperm decreases, sperm motility decreases; 4. Testicular torsion. The consequence of twisting of the spermatic cord is the infringement of its constituent arteries, nerves, and lymphatic vessels. The final stage may be testicular necrosis.
Diagnosis and treatment
Diagnosis of cryptorchidism in adults is carried out by a specialist urologist-andrologist. He finds out the nature of the patient’s pain and clarifies whether the patient’s family has relatives with similar pathologies. By palpating the scrotum, groin and pubic area, the doctor determines the location of the testicle. If it is discovered that the testis is in the abdominal cavity, the patient will be prescribed an ultrasound examination. Using ultrasound, the structure of the tissues and their size are examined. Additional diagnostic methods can be used: computer or magnetic resonance imaging, laparoscopy. If, as a result of examinations, bilateral cryptorchidism is detected in the patient, the latter will be given a referral for blood tests. Through laboratory tests, chromosome data is clarified and hormonal indicators are determined (testosterone, dihydrotestosterone, hCG). Drug therapy is not used in adults. The situation can be corrected surgically.
Types of operations
One-step
The Schumacher-Petrivalsky operation involves lengthening the spermatic cord. To provide access to the male gland, the surgeon makes two incisions: on the scrotum and in the inguinal canal. Using a biopsy, the structure of the underdeveloped testicle is examined. If concerns about the presence of malignant formations in the cells and tissues of the gland are confirmed, the testicle will be removed.
Two-stage
The spermatic cord is too short and does not allow the testicle to descend into the scrotum. In such cases, its movement takes place in two stages. At the first stage, the spermatic cord is lengthened and the testicle is fixed to the fascia lata of the thigh. A few months later, the tissue is moved to the scrotum area.
Laparoscopic method
Special tubes are inserted into the abdominal cavity of the patient through neat incisions, on the basis of which surgical instruments are installed. During the operation, amputation of the damaged testicle is possible. If necessary, a male gland implant will be placed in the scrotum area. The main advantage of the method is a noticeable reduction in the patient’s recovery process. After surgery, it is important to follow the doctor's recommendations. To prevent complications, the operated patient will be prescribed antibiotics and painkillers. During the first 10 days, bandages should be changed and sutures treated. Complete rehabilitation of the patient occurs in about a month. After this period, the man is allowed physical activity and sexual activity. In general, the prognosis for a patient diagnosed with cryptorchidism can be quite favorable. Even if one of the testicles is removed from the patient, the reproductive function can be performed by another male gland.
Cryptorchidism in children
Treatment methods for cryptorchidism in children:
- hormonal (non-operative)
- surgical
Hormonal treatment
This treatment method uses human chorionic gonadotropin. With bilateral cryptorchidism, there is a chance of recovery, but it is less than 30%. The child is given the hormone 2 times a week, the course is 4-5 weeks. If the drug is given to a boy in high doses, there is a risk of side effects:
- pubic hair
- skin pigmentation
- scrotal enlargement
- penis growth
- prostate hyperplasia
The phenomena listed above can be transient if the dose of the drug is selected adequately. Gonadotropin is in some cases combined with gonadotropin releasing hormone. But in some cases this combination is not indicated.
At what age is surgery performed for cryptorchidism?
Cryptorchidism, which appeared at birth, can be cured with surgical methods when the baby is 12 months old. very rarely the operation is performed earlier. The testicle may descend on its own within 6-8 months of the baby’s life. The operation is performed before 1 year of age for those who have a high position of the testicles (when they are in the abdominal cavity), as well as for those children who do not have movement of the testicles over time in the desired direction. In cases of secondary cryptorchidism, surgery may be performed between 3 and 7 years of age, depending on how early the diagnosis was made.
What happens after surgery?
- Observation of the testicle is facilitated, its diseases are detected in time
- Improves male reproductive function
- Prevents testicular torsion
- Abnormalities that develop in parallel with cryptorchidism (for example, inguinal hernia) are eliminated
- The risk of injury and limitation of testicular development is reduced to zero
What is the surgical treatment of cryptorchidism in children?
The surgical method is called orchiopexy and is performed in most cases, as stated, at the age of 1 year. Typically the method includes:
- Isolation of the testicle from surgical access in the groin area
- Removal of inguinal hernia (in 60-80% of cases)
- Reduction of the testicle into a “pocket” specially created from an additional incision on the scrotum
- Fixation of the testicle inside the above-described pocket
Surgery for cryptorchidism lasts from half an hour to 90 minutes. General or combined anesthesia. After the procedure, the child must remain in the hospital for 1-3 days. The patient must remain on strict bed rest for 3 days after surgical treatment. For further 30 days, you cannot make sudden movements or play outdoor games (football, catch-up, etc.).
Surgical treatment of cryptorchidism in children is quite complex, the implementation must be delicate, and there are technical subtleties. But the operation is not difficult for a child; in most cases, patients tolerate it well. The operation becomes more complicated when the testicle is high; the lower it is, the easier it is for the surgeon.
Complications after surgery are rare. Among them are the following:
- inflammation
- hematomas
- atrophy of the descended testicle (if the blood supply is impaired)
Treatment of abdominal form of cryptorchidism
In this form of the disease, the testicle is located as high as possible - in the retroperitoneal zone of the abdomen. The operation is usually performed using laparoscopy. Treatment is carried out in 2 stages, with a break between them of at least half a year.
Laparoscopy is an endoscopic examination of the abdominal cavity, in which small punctures are made in the anterior abdominal wall. This method allows you to find the testicles located above the inguinal canal in the retroperitoneal space. Laparoscopy makes it possible to sufficiently prepare the testicle for relegation to the scrotum or to remove an undeveloped testicle.
Anesthesia during surgery
In most cases, combined pain relief options are used: sedatives and local anesthesia. This allows you to significantly reduce the required dose of drugs used for anesthesia. Also, the described combination ensures the absence of mental trauma and good pain relief in the period after surgery.
What happens to the child after the operation?
The child may be discharged the day after testicular prolapse surgery. Pain relief may be needed for two days as the scrotum and incision area may be sore and restless. It is advisable to examine the child 1 week, 30 days, 6 months after surgical treatment. Then the examination is carried out before entering school at the age of 6-7 years and at the age of 16-17 years before entering a university.
A high location of the testicle can lead to pathological changes. The higher it is, the worse the prognosis. . Changes in the testicle and its reduced function are the main causes of infertility. With the intra-abdominal and upper-inguinal location of the testicles, changes begin by 1 - 1.5 years. Changes also occur in the false form of the disease in question, but they appear at the age of 6-8 years.
Results of orchiopexy in children
The operation is called orchiopexy. The sooner it is performed, the higher the chance that the testicle will function normally. But it is more difficult to perform an operation on a small child than on an older child; in such cases, tissues must be handled several times more carefully and carefully. Therefore, some surgeons send young patients with complex forms of cryptorchidism to specialized clinics where the qualifications of specialists are higher.
A timely and professionally performed operation allows you to restore fertility (the ability to reproduce) in most cases. The outcome of the operation depends on the experience of the surgeon and his knowledge of various techniques that allow the testicle to be lowered carefully and without tension. If primary cryptorchidism is not treated at an early age, then it is almost impossible to restore reproductive function.