A disease of the central nervous system, Charcot-Vulpian disease, is quite difficult to treat. Vision is especially affected by multiple sclerosis (MS). Most often, this is what initially brings patients to see a doctor. There are periods of remission and relapse. Experts note that in most cases the disease occurs in young people and may not make itself felt for a long time.
Causes and symptoms of the disease
As a result of the disease, the myelin sheath of nerve fibers is affected and plaques are formed, which are commonly called sclerotic. It affects the brain and spinal cord. The optic nerve is also affected. It is worth noting that experts do not have a consensus on the causes of the development of the disease. Thus, it is believed that multiple sclerosis is caused by a whole complex of factors, such as:
- genetic;
- viral;
- allergic;
- endocrine;
- geographical.
The symptoms of the disease vary from person to person. Patients may complain of symptoms such as lack of coordination of movements, muscle flaccidity, numbness, sudden paralysis and loss of balance. However, most often patients are brought to consult a doctor by visual impairment due to multiple sclerosis. This manifests itself in blurred images, pain and double images.
Multiple sclerosis.
Elena
October 20, 2020
Good afternoon. My name is Elena, I am 50 years old. On September 19, in the morning I experienced severe double vision and loss of coordination of movements. For a week I saw doctors: an ophthalmologist, a neurologist. The ophthalmologist concluded that everything was normal. The neurologist recommended an MRI. As a result, on September 24 she was hospitalized. They did a CT scan and diagnosed a stroke in both hemispheres. 11 days in the hospital, they gave me IVs. He was discharged home, and gradually his vision began to recover. But in the morning everything is still double. I had an MRI with contrast done on the doctor’s recommendation. Conclusion MRI - multiple sclerosis, in your own words, without accumulation. Further, in plain text, it was said that there were no specialists in this diagnosis. I have had type 2 diabetes mellitus (insulin) for 10 years. Please help. Next is the MRI conclusion. Study protocol No. 6704/1 October 14, 2020 Patient: Melnikova E. S. Date of birth: May 25, 1970 Diagnosis upon referral: Description: A series of MRI scans without IV contrast obtained images of sub- and supratentorial brain structures. The cortex and white matter of the brain are developed correctly, the differentiation of gray and white matter is preserved. In the cerebral hemispheres (periventricular, in the deep white matter and cortical-subcortical sections), numerous areas of hyperintense MR signal are detected in T2 and T2-FLAIR modes, hypointense in T1, without perifocal infiltration from 0.5 cm to 1.0x0.8 cm. After intravenous contrast, no accumulation of the contrast agent was detected in these areas. The structures of the brainstem and cerebellum are unremarkable. The pineal region is not deformed. The sella turcica is not changed. The structure of the pituitary gland is homogeneous. Parasellar structures without features. No additional formations were identified in the area of the cerebellopontine angles. The internal auditory canal is of normal width on both sides. The ventricular system of the brain is of normal size and shape, within the age normometry. The subarachnoid spaces and sulci of the brain are not expanded. The basal cisterns are not dilated or deformed. The midline structures are not displaced. The cerebellar tonsils are located at the level of the BZ. The craniovertebral junction is without features. The eyeballs are unchanged. The extraocular muscles are not thickened. The optic nerves are not thickened. Retrobulbar tissue without obvious space-occupying formations. The paranasal sinuses and cells of the mastoid processes of the temporal bones are developed normally, with clear contours. Pneumatization is not impaired. No obvious bone destructive changes were detected at the examination level. Conclusion: The MR picture of the detected changes in the cerebral hemispheres may correspond to the demyelinating process - MR control in dynamics.
Age:
50
The question is closed
stroke
multiple sclerosis
Ophthalmological manifestations of the disease
Rapid uncontrolled eye movements are observed.
The disease leads to various visual disturbances, but vision loss is rare. At the same time, patients often note that they soon begin to see worse. The degree of manifestation is very individual: sometimes a very slight decrease in sharpness, and sometimes almost complete blindness, when the eyes are able to distinguish only light of different brightness. In the first case, the situation is complicated by the fact that a person may not immediately notice the change. As a rule, visual impairment affects only one eye and is temporary. The following symptoms also occur:
- change or deterioration in the field of vision - a feeling of “spots” before the eyes;
- nystagmus - uncontrolled eye movements;
- diplopia - double image;
- increased sensitivity to light - colors become blurry, dull, and glare occurs.
If these symptoms occur, doctors strongly recommend undergoing examinations.
Diplopia
Diplopia (from the Greek διπλόος - double and ὀπός - eye) is a term that is used to refer to visual impairments in which the image of objects at which the patient is looking is double.
With ghosting, the image may shift horizontally, vertically or diagonally. Normally, eye movements are symmetrical, the visual axes of both eyes converge at one point (on the object we are looking at) and one image is formed in the brain. With some eye movement disorders, the visual axis deviates, and as a result, diplopia occurs.
Why is MS dangerous for vision?
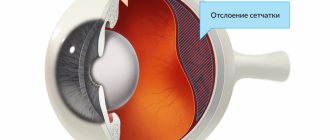
A common ophthalmological manifestation of the disease is inflammation of the optic nerve, which is experienced by more than half of patients. In medicine it is called retrobulbar neuritis. Often this symptom occurs several years before other complaints appear. At the same time, one should not draw premature conclusions and certainly associate neuritis with MS, since it may have other causes. Inflammation can be suspected in case of severe loss of vision, dyschromatopsia, or pain when moving the eyes. This condition lasts no more than 3 months, after which an improvement in well-being follows. However, in case of relapse, optic nerve atrophy may occur. Therapy for this disease is extremely complex and requires the intervention of more than one doctor.
Diagnostics
Therapeutic therapy from the conclusion of several highly specialized specialists.
For MS, consultation with a therapist, neurologist and ophthalmologist is necessary. You should submit your urine for laboratory testing, as well as a blood test: general, to determine sugar levels, and the Wasserman test. In case of neuritis, a “nicotine test” is used. The patient is administered nicotinic acid in a personally selected dosage. After this, a temporary improvement in vision by 0.3-0.5 parts is observed. This helps to show the “redness reaction” of the integumentary skin. Diagnosis of the state of the visual organ in case of disease is carried out by studying the topography of the spatial, light and color contrast sensitivity of the eye. Stereoscopic vision is tested, and a comprehensive electrophysiological analysis is performed. In addition, it is worth undergoing fluorescein angiography of the fundus and electroretinography.
The central nervous system and optic nerves are affected already in the early stages of MS. To identify the disease in the early stages, when there are still no symptoms, it is possible to check the topography of the spatial sensitivity of the eye. At the same time, the course of the disease, in which damage to the visual organ occurs, often has a more comforting scenario than the option when there are no ophthalmological manifestations.
Treatment methods
Drug treatment is carried out under the supervision of a doctor.
Some vision problems with MS go away on their own over time. So, for example, nystagmus can be a consequence of stress or the use of medications. And diplopia is characteristic of the exacerbation phase of the disease. Sometimes corticosteroid drugs are prescribed. In case of emergency, you can use an eye patch or special lenses. But, as a rule, after eliminating the cause, the symptom also disappears. However, retrobulbar neuritis necessarily requires therapy prescribed by doctors: a neurologist and an ophthalmologist. Specialists can prescribe the medications presented in the table.
Drugs for the treatment of neuritis
| Name | Features of use |
| "Methylprednisolone" | Used in the acute stage of the disease |
| Course of treatment 3-7 days | |
| Administered intravenously at 20-40 mg | |
| The drug can also be taken orally | |
| "Dexazon" | Prescribed in cases of severe disease |
| Injected retrobulbarly 1 ml once a day | |
| Treatment period: 7-10 days | |
| "Diprospan" | Apply retrobulbar 1 ml |
| Repeated administration no earlier than 5 days later | |
| "Dicynon" | Prescribed 0.5 ml retrobulbar |
| Duration of treatment - 5 days | |
| After the main course, it can be prescribed in the form of tablets and injections | |
| "Dalargin" | Helps improve microcirculation in the inflamed area |
| 1 mg intramuscularly for 30 days |
Treatment of diplopia
If the appearance of diplopia is associated with an exacerbation of multiple sclerosis, corticosteroid therapy can speed up the restoration of normal vision.
Along with therapy related to stopping exacerbations of MS, ophthalmologists and orthoptists have a number of tools and techniques that can help in treatment and adaptation: wearing special prisms, occlusion, botulinum toxin injections, as well as surgical interventions.
Prismatic correction
Wearing glasses with special prisms allows you to deflect the path of the rays and, thus, shift the image.
Another option for prismatic correction is Fresnel prisms - thin overlays on the lenses of ordinary glasses. The great advantage of Fresnel lenses is that as normal vision is restored, they can be replaced with prisms with a different refractive power.
Occlusion
In cases of severe exacerbation of MS, where multiple nerves are affected, occlusion may be one of the most practical options for adapting to the changes that have occurred. And while occlusion (forcing one eye to turn off) results in a loss of 3D perception, it doesn't mean you have to wear a pirate's eye patch. An alternative is special contact lenses, the use of a thin opaque tape on the lens of regular glasses or sunglasses.
Unfortunately, prismatic correction or occlusion does not always help to completely solve the problems associated with the appearance of diplopia. In this case, more active interventions should be considered:
Botulinum toxin injections
The use of botulinum toxin injections leads to temporary and sometimes permanent relief of the patient's condition with symptoms of diplopia. Botox is injected into one of the eye muscles under local anesthesia, which in most cases helps to achieve the desired effect and prevent the development of contractures.
Surgical intervention
If less invasive methods for correcting diplopia do not produce significant results and the patient continues to experience double vision for a long time (usually more than a year), surgical intervention may need to be considered as a method to help restore the symmetry of the eye positions. This operation is performed under general anesthesia and in most cases leads to the restoration of binocular vision.
Source