A group of eye diseases in which, along with damage to the optic nerve, an increase in intraocular pressure is observed, experts unite under one name - “glaucoma”. Despite the fact that the disease can be caused by various reasons and be acute or sluggish, all its forms are equally dangerous and often lead to complete loss of vision.
Glaucoma causes blindness in about 15 out of 100 adults and 10 out of 100 in children. Most often, the disease strikes after 40 years of age, but juvenile and infant forms are not uncommon, and boys suffer from it more often than girls.
The name glaucoma is derived from the ancient Greek words γλαυκός - “light blue, light blue” and ομα - “tumor”. It received this name because in the later stages the cornea of the affected eye sometimes acquires a cloudy bluish tint due to swelling and fluid accumulation.
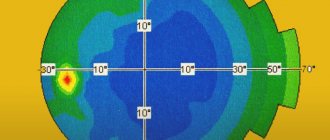
Target pressure for glaucoma
Reducing the IOP level to the required target pressure level is key to the effective treatment of glaucoma.
The treatment tactics for glaucoma are based on identifying risk factors and the fact of progression of GON and the possible impact on them. Since the leading factor in the pathogenesis and death of retinal ganglion cells in GON is recognized to be an increase in IOP levels above an individually tolerable level, the main goal in the treatment of glaucoma is to reduce IOP to a tolerable level, currently referred to as “target pressure”. “Target pressure” is the upper level of the tonometric IOP level (Pt), at which it is possible to slow down or stop damage to the internal structures of the eyeball and the breakdown of visual functions. Since there is no generally accepted method for determining “target pressure”, and we cannot know for sure whether the initially selected level of “target pressure” was adequate for a given patient, it is searched for in the process of monitoring the effectiveness of the treatment used. “Goal pressure” is determined taking into account all the risk factors for each individual patient as a result of a detailed examination and monitoring the dynamics of changes in the optic disc and visual field. The level of target pressure should be re-evaluated during the patient's follow-up and may need to be adjusted if optic disc and visual field changes continue to change at a rate that may pose a threat to maintaining quality of life within the patient's life expectancy.
Source
Modern ideas about the concept of “goal pressure”
Objective: to develop a practice-acceptable method for determining target pressure in patients with primary open-angle glaucoma (POAG) from the perspective of tolerant IOP. Methods: The study included patients with POAG who were divided into groups according to IOP level. A control group was also allocated. All patients underwent a standard ophthalmological examination, tolerant IOP and blood pressure in the brachial artery were measured. Tolerant IOP was determined according to computer tonosphygmography data by normalizing the elasticity index of intraocular vessels (PESG) and according to computer perimetry data with drug-induced reduction of ophthalmotonus. For drug reduction of IOP, drugs were used that do not have a negative effect on the hemodynamics of the eye: betoxolol, brinzolamide, travaprost, diacarb, 20% glyceroascorbate solution. Results: The study included 1310 patients (1638 eyes) with POAG. The control group consisted of 365 healthy individuals (640 eyes). The average value of true IOP in healthy individuals was 14±0.1 mmHg. The average value of tolerant true IOP in patients with POAG was 16.5±0.1 mmHg. The difference between the average values of true IOP in healthy individuals and tolerant pressure in patients with glaucoma is statistically significant (p <0.05). From the perspective of tolerant pressure, in order to achieve the target pressure, it is necessary to reduce the initial level of intraocular pressure in patients with glaucoma with moderately elevated intraocular pressure values by 45%, and with initially high IOP values – by 60%. Conclusions: with increasing age, anteroposterior size of the eyeball, and stage of glaucoma, the level of tolerant IOP decreases. With an increase in diastolic blood pressure, the level of tolerant pressure increases. The target pressure should not exceed the tolerable IOP. Key words: POAG, target pressure, tolerant pressure. Abstract Present–day conceptions of “target pressure” SV Balalin, VP Fokin
Volgograd department of FGU “MNTK “Eye Microsurgery” named after Fedorov SN of Rosmedbiotechnology” Purpose: to develop a practical method of target pressure definition in patients with POAG taking into consideration their tolerant pressure.
Methods: Patients with POAG were distributed into groups according to their IOP level. Also there was a control group including healthy subjects. Standard ophthalmological examination, tolerant IOP level and arterial pressure measurements were performed in all patients. Tolerant IOP was defined by computer tonosphygmography by index of elasticity of intraocular vessels and by computer perimetry during treatment–induced decrease of the IOP level. As local hypotensive therapy there were used drugs not affecting an eye hemo dynamics: betaksolol, brinzolamide, travoprost, diacarb, 20% glyceroascorbate. Results: 1310 patients (1638 eyes) with POAG were included into the study. Сontrol group consisted of 365 healthy subjects (640 eyes). Average level of measured IOP in healthy subjects was 14±0.1 mm Hg. Average tolerant IOP level in POAG patients was 16.5±0.1 mm Hg. Difference between measured IOP level and tolerant IOP was statistically reliable (p<0.05). Conclusions: Taking into consideration tolerant IOP level it is recommended to decrease the initial IOP level in patients with moderately increased IOP level by 45% and in patients with initially high IOP level – by 60%. With age, enlargement of a anterior – posterior size of an eye globe and stage of glaucoma, the level of tolerance IOP decreases. Level of tolerant IOP increases with the raising of a diastolic arterial pressure. Target pressure should not exceed the tolerant IOP level. Key words: POAG, target pressure, tolerant pressure.
The leading risk factor for the development and progression of glaucomatous optic neuropathy is an increase in ophthalmotonus above the individually tolerated (tolerant) pressure. Currently, the terms “tolerant”, “intolerant”, “targeted” and “individual IOP” are widely used in the literature. For the first time, the determination of tolerant intraocular pressure (IOP) in glaucoma was proposed by A.M. Vodovozov in 1975. The author considered tolerant pressure as the upper limit of the normal IOP inherent in a given patient, above which it becomes pathological - intolerant. Campimetric, perimetric, electrooculographic and tonosphygmographic methods for determining individually tolerable IOP have been developed and proposed for practical use [3–8,14–19]. The target pressure is understood as a conditionally selected by the doctor safe level of IOP for a given patient [5,9–13]. The most common recommendation is to initially reduce IOP by 20–40% below baseline. However, this approach is of an empirical indicative nature and may lead to errors in calculations and, consequently, in the selection of the necessary antihypertensive treatment for a particular glaucoma patient. According to the literature, tolerance and target pressure are sometimes considered as identical concepts [17], as a certain level or range of IOP that does not have a negative effect on the eyeball. This raises questions: 1. What is the difference between tolerance and target pressure? 2. How accurate is the generally accepted formulation: “The leading role in the treatment of glaucoma belongs to the reduction of IOP to a tolerable level”? It is important in the pathogenetic treatment of glaucoma to reduce the increased (intolerant) ophthalmotonus to the target IOP, which should not exceed the tolerant pressure (the upper limit of the individual norm). Introduction into practice of a simple and reliable method for determining target IOP is one of the most important tasks in the pathogenetic treatment of glaucoma. When determining target pressure, risk factors for glaucoma progression should be taken into account. Purpose of the study: to develop a practice-acceptable method for determining target pressure in POAG patients from the position of tolerant IOP, taking into account risk factors for glaucoma progression, and compare it with the standard method for determining target pressure. Material and methods of research 1310 patients (1638 eyes) with POAG were examined. The initial stage of glaucoma was detected in 63.3% of cases - in 866 patients (1037 eyes), the advanced stage was found in 19% of cases, in 254 patients (279 eyes), the advanced stage - in 17% of cases, in 190 patients (320 eyes). eye). According to the IOP level, patients were divided into the following groups: with normal IOP values (from 11 to 21 mm Hg) - 41.9% (686 eyes), with moderately elevated IOP values (from 22 to 32 mm Hg. ) – 47.2% (774 eyes), with high IOP values (over 32 mm Hg) – 10.9% (178 eyes). The control group consisted of 365 healthy individuals (640 eyes). All patients underwent a standard ophthalmological examination, tolerant IOP was also studied, and blood pressure (BP) in the brachial artery was measured. Tolerant IOP was determined according to computer tonosphygmography data by normalizing the elasticity index of intraocular vessels (PESG) and according to computer perimetry data with drug-induced reduction of ophthalmotonus. For drug reduction of IOP, drugs were used that do not have a negative effect on the hemodynamics of the eye: betaxolol, brinzolamide, travoprost, diacarb, 20% glyceroascorbate solution. IOP, at which the maximum improvement in the test function is recorded, is tolerant and is designated as P0 tl. The target pressure in patients with glaucoma was determined by the standard method as a 30% decrease in the initial level of ophthalmotonus. The obtained data were processed using the Statistica 6.0 program on an IBM PC. Based on the results of multivariate analysis, the influence of risk factors (age, diastolic blood pressure level, stage of glaucoma, anteroposterior size of the eyeball) on tolerant pressure was taken into account. Results The average value of true IOP in healthy individuals was 14±0.1 mmHg. The average value of tolerant true IOP in patients with POAG was 16.5±0.1 mmHg. The difference between the average values of true IOP in healthy individuals and tolerant pressure in patients with glaucoma is statistically significant (p <0.05). This means that the tolerance pressure corresponds to the upper limit of the individual IOP norm, which is consistent with the data of A.M. Vodovozova et al. [5,6]. Based on multivariate analysis, a relationship was established between tolerant pressure and risk factors, which was characterized by the following formula: P0tl = 24.8 + 0.07*AD diast. – 0.3*stage – 0.022*age – 0.54*PVR, (1) where: Р0tl – tolerant true IOP, mm Hg; BP diast. – diastolic pressure in the brachial artery, mm Hg; PZR – anteroposterior size of the eyeball; 24.8; 0.07; 0.3; 0.022 and 0.54 are the regression equation constants. All coefficients of this equation are highly significant (p<0.001). The average value of the tolerance pressure calculated using this formula is 16.7 ± 0.12 mm Hg. Calculating the tolerant pressure using the formula allows you to take into account the above factors that affect the level of tolerant pressure. Considering that individual IOP in healthy individuals is on average 2.5 mm Hg lower than the tolerant pressure in patients with glaucoma, the target pressure should also be 2.5 mm Hg lower than the tolerant level. and correspond to individual ophthalmotonus in healthy individuals: P0 targe = P0 tl – 2.5. Table 1 presents the average values of target pressure, which was calculated by the method of 30% reduction in the initial level of ophthalmotonus, as well as the average values of tolerant pressure, which was determined in patients with POAG using formula (1) depending on age and the level of diastolic blood pressure in the brachial artery. It should be noted that only in the group of POAG patients (686 eyes) with initially normal intraocular tone values, the average target pressure value was lower than the average tolerant IOP value by 4.1 mm Hg. This means that the level of target pressure calculated using this method is safe in these patients and contributes to the stabilization of visual functions. In patients with moderately elevated (774 eyes) and high initial IOP values (178 eyes), the target pressure was significantly higher than the tolerant pressure - it was intolerant (p<0.05). This indicates the inaccuracy of the method for calculating the target pressure in these groups, the need for a more pronounced reduction in ophthalmotonus - over 30%, and the advantage of determining the target pressure based on tolerant IOP, taking into account risk factors in a particular patient. From the perspective of tolerant pressure, in order to achieve the target pressure, it is necessary to reduce the initial level of intraocular pressure in patients with glaucoma with moderately elevated intraocular pressure values by 45%, and with initially high IOP values – by 60%. Conclusions. With increasing age, anteroposterior size of the eyeball, and stage of glaucoma, the level of tolerant IOP decreases. With an increase in diastolic blood pressure, the level of tolerant pressure increases. The target pressure should not exceed the tolerable IOP.
Literature 1. Antonov V.V. and others. Biophysics. M.: Humanite. ed. , 1999. 288 p. 2. Alekseev V.N., Egorov E.A., Martynova E.B. On the distribution of intraocular pressure levels in a normal population // Klin. ophthalmology. 2001. T. 2. No. 2. P. 38–40. 3. Balalin S.V., Gushchin A.V. New opportunities for studying tolerant IOP in patients with primary open-angle glaucoma using automated ophthalmotonosphygmography // Glaucoma. 2003. No. 3. P. 15–20. 4. Balalin S.V. On the issue of tolerant, intolerant, individual and target pressure in primary glaucoma // Glaucoma: reality and prospects: collection. scientific articles. M., 2008. pp. 126–129. 5. Bachaldin I.L., Marchenko A.N. Possibility of increasing the effectiveness of metabolic therapy for glaucomatous optic neuropathy after achieving the “goal pressure” // Ophthalmology of the Black Sea countries: collection. scientific tr. Krasnodar, 2006. pp. 282–285. 6. Boriskina L.N. Determination of tolerant intraocular pressure in glaucoma and its clinical significance: Dis. ...cand. honey. Sci. Kuibyshev, 1985. 139 p. 7. Vodovozov A.M. Tolerant and intolerant intraocular pressure in glaucoma. Volgograd, 1991. 160 p. 8. Vodovozov A.M., Balalin S.V., Mussa Al-Hindi, Frolova N.V. A new method for measuring tolerant intraocular pressure in glaucoma // Ophthalmol. magazine 1997. No. 3. pp. 157–161. 9. Volkov V.V. Glaucoma at pseudonormal pressure. M., 2001. 352 p. 10. Volkov V.V. Intraocular pressure (IOP) and stabilization of glaucoma: Abstract. report VIII Congress of Russian Ophthalmologists. M., 2005. pp. 143–144. 11. Egorov E.A. Rational pharmacotherapy in ophthalmology. M., 2004. 954 p. 12. Zubkova T.G. Target pressure: calculation method and influence on the stabilization of the glaucomatous process: Author's abstract. ...cand. honey. Sci. St. Petersburg, 2005. 16 p. 13. Krasnov M.M. About target intraocular pressure // Klin. ophthalmology. 2003. T. 4. No. 2. P. 49. 14. Makashova N.V. Early diagnosis, features of clinical manifestations and treatment of open-angle glaucoma with myopia: Dis... doc. honey. Sci. M., 2004. 240 p. 15. Moshetova L.K., Koretskaya Yu.M. On the tactics of approach to the treatment of patients with glaucoma // Klin. ophthalmology. 2005. No. 2. P. 78–80. 16. Nesterov A.P., Egorov E.A. Glaucoma: controversial issues, possibilities for consensus: abstract. report VIII Congress of Russian Ophthalmologists. M., 2005. pp. 142–143. 17. Shmyreva V.F., Shmeleva–Demir O.A., Mazurova Yu.V. Towards the determination of individually tolerable intraocular pressure (target pressure) in primary glaucoma // Vestn. ophthalmol. 2003. No. 6. P. 3. 18. Shmyreva V.F. Risk factors and target intraocular pressure in glaucomatous optic neuropathy // Glaucoma: reality and prospects: collection. scientific articles. M., 2008. pp. 105–109. 19. Khadikova E.V., Egorova T.E. On a method for determining individually tolerated intraocular pressure in patients with glaucoma // Klin. ophthalmology. 2004. T. 5. No. 2. P. 51–54.
Normal pressure glaucoma: causes and treatment
Normal pressure glaucoma is quite difficult to determine; during the course of the disease there is no increased intraocular pressure, it is normal. The disease is usually diagnosed in older women.
Glaucoma develops as a result of previous diseases of the visual apparatus or due to age-related changes in the organs of vision, which subsequently lead to disturbances in the blood circulation of the brain. It is necessary to conduct a complete diagnosis to identify the disease and regularly visit an ophthalmologist.
In most cases, treatment will require surgical treatment; medication methods help extremely rarely and have side effects. In this article we will talk about how normal pressure glaucoma occurs, why it occurs and how to treat it.
Normal pressure glaucoma
But there is another condition of this disease - glaucoma without increased intraocular pressure, it is also called “normal pressure glaucoma”. This is a fairly rare phenomenon in which the nerve suffers negative changes, vision deteriorates, but the pressure inside the visual organ remains normal.
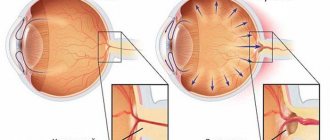
Glaucoma is a disease that affects the optic nerve, which connects the eye to the brain. It allows you to see. This condition usually occurs when intraocular pressure is very high. But normal-tension glaucoma looks different.
There is usually fluid circulating around the eye. In many types of glaucoma, it does not drain as expected. Thus, it accumulates, like water in a clogged drain. As a result, pressure builds up in the eye. Over time, it begins to damage the optic nerve.
In normal-tension glaucoma, the optic nerve is damaged even if the eye pressure remains within normal limits. Doctors call this normal (low) pressure glaucoma.
In normal-tension glaucoma, true intraocular hypertension does not occur. More often this disease is diagnosed in women. Low-tension glaucoma is characterized by the following symptoms:
- During gonioscopy, the angle of the anterior chamber of the eye is open;
- The average pressure level inside the eye does not exceed 21 mm Hg. even with daily use;
- Characteristic changes in the optic nerve fibers and narrowing of the visual fields occur;
- There are no secondary causes for such changes in the optic nerve.
The classification of primary open-angle glaucoma is based on indicators of the epidemiological significance of normal intraocular pressure. However, these data are relatively arbitrary and clinically unreliable.
The incidence of normal and low-tension glaucoma in patients over 40 years of age occurs in 0.2-16% of cases (among patients with open-angle glaucoma). Normal pressure glaucoma mainly affects women aged 60 years.
Normotensive is a type of disease when vision deteriorates due to damage to the optic nerve, while intraocular pressure remains normal. It is also called normal or low pressure glaucoma.
Ocular pressure is also called intraocular pressure or eye tension. Its level is measured in mm of mercury. Most patients suffering from glaucoma have increased intraocular pressure - more than 21 mm Hg.
The same cannot be said about glaucoma without high blood pressure. Here the level is kept within the range of 10-21 mm Hg, that is, the indicator is normal.
This form of the disease occurs predominantly in females. The age at which glaucoma without increased EDH is most often detected is after 40 years. Normal intraocular pressure is also characteristic of the open-angle form of the disease in the first stages, therefore the features of these two types of disease are similar.
Normal-tension glaucoma (or low-tension glaucoma) is more common in women and is characterized by:
- Average level of IOP Causes of development at normal and low pressure
Doctors aren't sure why some people develop normal-tension glaucoma. The optic nerve may be more sensitive or fragile, so even normal pressure can damage it. Or this type of glaucoma may be caused due to a lack of blood in the optic nerve.
Poor blood flow can damage and ultimately destroy the cells that transmit signals from the eye to the brain. A disease such as atherosclerosis, which is a buildup of fatty deposits in the arteries, makes it difficult for blood to circulate well.
This type of glaucoma is most likely to occur if you:
- this disease runs in the family;
- Japanese origin;
- have ever had heart disease.
For a disease to occur, a combination of many factors is necessary. The most important of them are:
- personal peculiarity of the eye structure;
- heredity;
- problems with the endocrine system;
- abnormalities in the cardiovascular system;
- nervous system failures.
Doctors tend to believe that the progression of the disease depends on a number of different reasons that activate the processes of occurrence and development of the disease.
Impaired visual function in glaucoma consists of impaired fluid circulation with its subsequent accumulation, which causes an increase in intraocular pressure (IOP).
Content:
- 1 Stages of glaucoma
- 2 Level of intraocular pressure
- 3 Dynamics of the glaucomatous process
- 4 Congenital primary glaucoma
- 5 Diagnostic methods:
Description
Glaucoma refers to chronic eye diseases that lead to irreversible loss of visual function.
Globally, up to 105 million people suffer from glaucoma; 5.2 million people are blind in both eyes, 1 patient goes blind every minute, and 1 child goes blind every 10 minutes. In Russia, glaucoma is the main cause of visual disability (28%).
Today in Russia there are more than 850,000 patients with glaucoma. Every year, 1 in 1,000 people develop glaucoma again. The overall incidence of the population increases with age: among people over 40 years of age it is 1.5%, and among people over 80 years of age it is 14%. More than 15% of blind people have lost their sight as a result of glaucoma.
The concept of “glaucoma” unites a large group of eye diseases of various etiologies. All these diseases include:
• increase in intraocular pressure above the level tolerant for the optic nerve (TVOP);
• development of glaucomatous optic neuropathy with subsequent atrophy (with excavation) of the optic nerve head;
• occurrence of typical visual field defects.
In the pathogenesis of glaucoma, the most important is a violation of the hydrodynamics of the eye, the ratio of production and outflow of intraocular fluid.
Intraocular fluid is produced in the posterior chamber of the eye by processes of the ciliary body, and then enters the anterior chamber of the eye through the opening of the pupil. Previously, moisture passes through the structures of the vitreous body, which thus carries out trophic and metabolic functions.
In the anterior chamber, intraocular fluid is directed to the angle of the anterior chamber of the eye, where the anterior and posterior outflow tracts are located.
Intraocular fluid from the posterior chamber through the opening of the pupil enters the angle of the anterior chamber, then flows away, overcoming the resistance of the trabecular tissue, through the cavity of the scleral sinus, collector canals, intrascleral plexus, flowing into the aqueous veins.
Intraocular fluid from the posterior chamber through the opening of the pupil enters the angle of the anterior chamber, then flows along the fibers of the ciliary muscle into the suprauveal and suprachoroidal space and then through the thickness of the sclera to the outside.
In recent years, new data have been obtained on the pathogenesis and clinical picture of glaucoma, which required changes to the existing classification of the disease.
Below is the classification of glaucoma developed by A.P. Nesterov and E.A. Egorov (2001).
Glaucoma is divided into:
• by origin - primary, secondary and combined with developmental defects of the eye and other structures of the body;
• by patient’s age – for congenital, infantile, juvenile and adult glaucoma;
• according to the mechanism of increasing intraocular pressure - into open-angle, closed-angle, with dysgenesis of the anterior chamber angle, with pretrabecular block and with peripheral block;
• according to the level of intraocular pressure - into hypertensive and normotensive;
• according to the degree of damage to the optic nerve head - initial, developed, advanced and terminal;
• downstream - stable and unstable.
In primary glaucoma, pathogenic processes that occur in the UPC, the drainage system of the eye or in the head of the optic nerve, preceding the onset of the disease, have no independent significance. They are the initial stages of the pathogenesis of glaucoma.
In secondary glaucoma, the mechanisms of glaucoma development are caused by independent diseases and do not always cause glaucoma, but only in some cases. Secondary glaucoma is a possible complication of other diseases.
↑ Stages of glaucoma
The division of the continuous glaucoma process is conditional. When determining the stage of glaucoma, the state of the visual field and optic nerve head are taken into account.
Stage I (initial) - the boundaries of the visual field are normal, but there are changes in the paracentral parts of the visual field (individual scotomas in the zone of 5-20°, Bjerum's arcuate scotoma, widening of the blind spot). The excavation of the optic nerve head is expanded, but does not reach its edge.
Stage II (developed) - pronounced changes in the visual field in the paracentral region in combination with a narrowing of its boundaries by more than 10° in the upper and/or lower nasal segment, marginal excavation of the optic nerve head.
Stage III (far advanced) - the border of the field of vision is concentrically narrowed and in one segment or more is located less than 15° from the point of fixation, marginal subtotal excavation of the optic nerve head.
Stage IV (terminal) - complete loss of vision or preservation of light perception with incorrect light projection. Sometimes a small island of the visual field is preserved in the temporal sector.
↑ Level of intraocular pressure
When making a diagnosis, intraocular pressure is indicated by:
• letter “a” - within normal values (P0 below 22 mm Hg);
• letter “b” - moderately increased intraocular pressure (P0 below 33 mm Hg);
• letter “c” - high pressure (P0 equal to or higher than 33 mm Hg).
↑ Dynamics of the glaucomatous process
There are stable and unstable glaucoma. With a stable course of the disease and long-term observation (at least 6 months), the condition of the visual field and optic nerve head does not deteriorate. In the case of unstable flow, such changes are detected upon repeated treatment. When assessing the dynamics of the glaucomatous process, one pays attention to the correspondence of the IOP level to the target pressure.
Diagnostic examination scheme
• Daily tonometry for (3-4 days);
• Biomicroscopy (aqueous veins, anterior chamber depth, angle profile, iris atrophy, pseudoexfoliation, pigment dispersion);
• Determination of the boundaries of the field of view (perimetry);
• Direct ophthalmoscopy (state of the optic disc and retina).
There are 5 main groups:
• congenital primary glaucoma;
• congenital glaucoma, combined with other developmental defects;
• primary open-angle glaucoma (POAG);
• primary angle-closure glaucoma (PACG); • secondary glaucoma.
↑ Congenital primary glaucoma
Symptoms of glaucoma may appear immediately after the baby is born or after some time. Depending on the age at which the disease begins, congenital, infantile and juvenile glaucoma is distinguished.
Primary congenital glaucoma (hydrophthalmos) manifests itself before 3 years of a child’s life. The disease is inherited in a recessive manner, although sporadic cases are possible.
The pathogenesis of this type of glaucoma is associated with dysgenesis of the anterior chamber angle, which causes disruption of the outflow of aqueous humor and increased intraocular pressure.
The clinical picture includes photophobia, lacrimation, blepharospasm, enlargement of the eyeball, enlargement and swelling of the cornea, excavation of the optic nerve head, and conjunctival hyperemia.
The stage of the glaucomatous process is determined by the degree of increase in the diameter of the cornea, expansion of the excavation of the optic nerve head and decrease in visual function (Table 1).
Table 1. Stages of the glaucomatous process in primary congenital glaucoma
↑ Diagnostic methods:
• tonometry (in children under 3 years of age, P0 = 14-15 mm Hg is normal. In primary congenital glaucoma, P0 exceeds 20 mm Hg or an asymmetry of more than 5 mm Hg is detected);
• measurement of the diameter of the cornea (normally in a newborn the diameter is 10 mm, by 1 year it increases to 11.5 mm, by 2 years - to 12 mm. With congenital primary glaucoma, the diameter of the cornea is increased to 12 mm or more already in the 1st year of life);
• biomicroscopy (swelling and clouding of the cornea, ruptures of Descemet's membrane, deepening of the anterior chamber, atrophy of the iris stroma with exposure of its radial vessels);
• ophthalmoscopy (normally, in a newborn, the fundus of the eye is pale, the optic disc is paler than in an adult, physiological excavation is absent or weak. In primary congenital glaucoma, excavation quickly progresses, but in the early stages, with a decrease in intraocular pressure, excavation is reversible. An approximate assessment of excavation can be made , knowing that an increase in corneal diameter by 0.5 mm corresponds to an increase in excavation by 0.2);
• gonioscopy.
Differential diagnosis should be carried out with megalocornea, traumatic lesions of the cornea, congenital dacryocystitis, combined congenital glaucoma (Peters syndrome, Marfan syndrome, sclerocornea, etc.).
Table 2. Principles of differential diagnosis of primary congenital glaucoma.
General principles of therapy.
Drug treatment of primary congenital glaucoma is ineffective and is used only before surgery. For this purpose, drugs are prescribed that inhibit the production of aqueous humor: beta-blockers, 0.25-0.5% solution of timolol maleate 2 times a day by drip, local carbonic anhydrase inhibitors, 2% solution of dorzolamide 3 times a day by local drip, 1% solution brinzolamide 2 times a day. According to indications, systemic use of carbonic anhydrase inhibitors and osmotic diuretics is possible.
The choice of the type of surgical intervention depends on the stage of the disease and the structural features of the UPC. In the early stages, goniotomy or trabeculotomy is performed; in later stages, fistulizing operations and destructive interventions on the ciliary body are more effective.
The prognosis with timely surgical intervention is favorable. Persistent normalization of intraocular pressure is achieved in 85% of cases. If the operation is performed in the early stages, then in 75% of patients it is possible to maintain visual functions throughout life. If the operation was performed late, then vision is preserved in only 15-20% of patients.
Primary infantile
Glaucoma occurs in children aged 3 to 10 years. Inheritance and pathogenetic mechanisms are the same as for primary congenital glaucoma. However, unlike primary congenital glaucoma, the cornea and eyeball are not enlarged. The principles of therapy are similar to those for primary congenital glaucoma.
Primary juvenile glaucoma
occurs between the ages of 11 and 35 years. Inheritance is associated with abnormalities in chromosomes 1 and TIGR. The mechanisms of impaired outflow of intraocular fluid and increased intraocular pressure are associated with the occurrence of trabeculopathy and/or goniodysgenesis. An increase in intraocular pressure and progressive glaucomatous atrophy of the optic nerve head are noted. Changes in visual functions occur according to the glaucomatous type. The principles of therapy are similar to those for primary congenital glaucoma.
Blood pressure readings
The IOP of a healthy person ranges from 10 to 22 mm Hg. Art. Depending on its increase, there are 4 stages of disease development:
- Initial stage. Typically, IOP is within normal limits - 20-22 mm Hg. Art.
- Moderate glaucoma. A slight increase in eye pressure - up to 26 mm Hg. Art.
- Far gone. The pressure increases to 33 mmHg. Art.
- Terminal stage. Indicators exceed 35 mm Hg. Art.
It must be remembered that eye pressure may change throughout the day. In the morning it is higher, and in the evening it decreases. A fluctuation between values of up to 3 mm Hg is considered normal. Art.
Characteristic symptoms of the disease
As nerve fibers die, blind spots will begin to appear in your visual perception. But they may not be noticed until most of the optic nerve fibers die.
As the condition worsens, the field of vision narrows. It's as if you are looking through a tunnel. If all the fibers in the optic nerve die, blindness occurs.
Normal tension glaucoma progresses slowly. It is important to have regular eye exams with an ophthalmologist. This is a doctor who specializes in providing ophthalmic care and performing eye surgeries. Screenings can help detect the disease before vision loss occurs.
The IOP value is usually 16-19 mmHg. Art., but in some cases its level is below 15 mm Hg. Art. Asymmetry in the manifestation of the disease is characteristic: the more severe the damage to the optic nerve, the higher the intraocular pressure.
- Changes in the optic nerve and parapapillary zone are identical to the characteristic changes in primary open-angle glaucoma.
- Streak-shaped hemorrhages along the edge of the disc are more typical for normal (low) pressure glaucoma and may indicate the progression of changes in the nerve fibers of the retina.
- Characterized by more frequent visualization of the cribriform plate area at the bottom of the excavation.
Visual field defects do not differ from changes in primary open-angle glaucoma, although it has been found that in normal (low) pressure glaucoma they are localized closer to the center and are more pronounced.
In some cases, even without treatment, these changes do not progress. However, often due to late diagnosis of normal (low) pressure glaucoma, the tendency to more pronounced damage is more pronounced than with primary open-angle glaucoma.
Other differences between normal (low) glaucoma and primary open-angle glaucoma:
- Peripheral vasospasm during cooling (Raynaud syndrome).
- Migraine, which is more common with normal (low) pressure glaucoma, although this has not been confirmed by any mass population surveys.
- Systemic nocturnal hypotension and untreated systemic hypertension.
- A decrease in blood flow velocity in the ophthalmic artery, confirmed by transscleral Doppler ultrasound.
- Paraproteinemia and the presence of autoantibodies in the blood serum.
Open-angle glaucoma and normal-tension glaucoma are characterized by the absence of symptoms. If a drop in ophthalmotonus occurs over a long period (several years), the only sign of the disease is a gradual decrease in vision.
With inflammation, dehydration and infections, a sharp decrease in pressure occurs. The patient's eyes dry out and lose their shine, and sometimes the eyeballs become sunken. Sharp pain in the eyes is a symptom of angle-closure glaucoma.
Only angle-closure glaucoma has severe symptoms.
It is characterized by:
- sharp pain in the eyes and accompanying migraines;
- redness of the eyeballs, dilation of the pupils, swelling of the cornea;
- discomfort when reading texts written in small print; while working at the computer; in rooms with poor lighting;
- “flies” before the eyes;
- noticeable visual impairment;
- with exacerbation of glaucoma, IOP levels reach 70 mm Hg, dizziness, vomiting, nausea and acute pain in the eyes.
Low pressure glaucoma has the following symptoms:
- The value of intraocular pressure in most cases is 16-19 mmHg. Art., but sometimes its level can be below 15 mm Hg. Art. A characteristic feature of the disease is the asymmetry in the manifestation of symptoms: the higher the degree of damage to the optic nerve, the higher the intraocular pressure.
- Changes in the parapapillary region and optic nerve are the same as in the case of primary open-angle glaucoma. The presence of streak-shaped hemorrhages along the edge of the disc is more typical for glaucoma with normal or low intraocular pressure.
- The peculiarity of visual field defects is that they, in fact, do not differ from those in primary open-angle glaucoma. However, with glaucoma accompanied by normal or high blood pressure, they are more pronounced and located closer to the center.
- Spasm of peripheral vessels during hypothermia (Raynaud's syndrome).
- Migraine headaches (although this symptom is considered to be a distinctive feature of normotensive glaucoma, the data require additional statistical studies).
- Fluctuations in general blood pressure (both hypertension and hypotension occur, in particular systemic nocturnal).
- Blood circulation disorders in the ophthalmic artery.
- Biochemical and immune disorders (paraproteinemia, autoantibodies in the blood serum).
Signs
1. The pressure inside the eye increases slightly - up to 18-20 mmHg - but often remains within 15-16 mmHg. Typically, with more severe optic nerve abnormalities, intraocular pressure is higher.
2. Optic nerve:
- the optic nerve and peripapillary zone are changed as they usually change in primary open-angle glaucoma;
- with increasing pathological changes in the retina, hemorrhages (hemorrhages) may be observed in the form of peculiar streaks along the edge of the disc - this sign is more characteristic of normotensive glaucoma;
- Often, when examining the fundus, one can observe the internal structures of the sclera - the so-called. cribriform plate;
3. Visual field defects.
Visual field impairments in normal-tension glaucoma are specific to any primary open-angle glaucoma. However, these disorders are usually shifted to the center and more pronounced. In some patients, visual field defects are quite stable even in the absence of treatment; in others, on the contrary, they tend to progress despite therapy.
4. Spasm of peripheral vessels during hypothermia (Raynaud's syndrome).
5. Migraine headaches (although this symptom is considered to be a distinctive feature of normotensive glaucoma, the data require additional statistical studies).
6. Fluctuations in general blood pressure (both hypertension and hypotension occur, in particular, systemic nocturnal).
7. Blood circulation disorders in the ophthalmic artery.
8. Biochemical and immune disorders (paraproteinemia, autoantibodies in the blood serum).
1. The IOP value is usually 16-19 mm Hg. Art. but in some cases its level is below 15 mm Hg. Art. Asymmetry in the manifestation of the disease is characteristic: the more severe the damage to the optic nerve, the higher the intraocular pressure.
2. Optic nerve
• Changes in the optic nerve and parapapillary zone are identical to the characteristic changes in primary open-angle glaucoma.
• Streak-shaped hemorrhages along the edge of the disc are more characteristic of normal (low) pressure glaucoma and may indicate the progression of changes in the nerve fibers of the retina.
• Characterized by more frequent visualization of the cribriform plate area at the bottom of the excavation.
3. Visual field defects do not differ from changes in primary open-angle glaucoma, although it has been found that in normal (low) pressure glaucoma they are localized closer to the center and are more pronounced.
In some cases, even without treatment, these changes do not progress. However, often due to late diagnosis of normal (low) pressure glaucoma, the tendency to more pronounced damage is more pronounced than with primary open-angle glaucoma.
With unilateral perimetric changes, the chance of developing similar changes in the fellow eye within 5 years is 40%.
• Peripheral vasospasm during cooling (Raynaud syndrome).
• Migraine, which is more common with normal (low) pressure glaucoma, although this has not been confirmed by any mass population surveys.
• Systemic nocturnal hypotension and untreated systemic hypertension.
• Decrease in blood flow velocity in the ophthalmic artery, confirmed by transscleral Doppler ultrasound.
• Paraproteinemia and the presence of autoantibodies in the blood serum.
Performed only on patients with documented progressive changes in visual fields. It consists of reducing intraocular pressure by 30% of the initial level.
1. Medication. Betaxolol may be the drug of first choice as it improves blood supply to the optic nerve along with a hypotensive effect. It is known that prostaglandin analogues have a greater hypotensive effect in normotensive eyes.
2. Trabeculectomy is necessary in at least one eye if visual fields progressively deteriorate despite low intraocular pressure values.
3. Systemic calcium channel blockers (nifedipine) are prescribed to young patients, as well as in the initial stage of the disease. Before treatment, it is desirable to diagnose peripheral vasospasm using capillaroscopy. Long-term therapy will be successful only if the visual fields do not have negative dynamics after short-term (2-3 months) treatment.
4. Daily monitoring of blood pressure. If nocturnal hypotension is reliably detected, it is necessary to stop taking general antihypertensive drugs, especially before bedtime.
It was stated above that the disease is dangerous because it has no symptoms in the early stages of development. People may attribute the feeling of burning in the eyes, heaviness, and dryness to general fatigue and not assume that the disease has begun to develop.
A little later, the pathology manifests itself more acutely: sharp pain in the eyes, severe headaches (especially in the temples and eyes), the whites of the eyes acquire a red tint. All of the above indicates the effect of IOP on the optic nerve.
And if it is not normalized in time, you can go blind.
An increase or decrease in pressure, as well as the development of other symptoms, will be caused by the causes of the development of the pathology.
At low pressure
The eyeballs become sunken, lose their shine and look dry. There are no painful sensations, visual acuity gradually decreases and atrophy of eye tissue occurs. If the necessary therapy is not carried out, these changes will be irreversible.
With high blood pressure
Diagnosis of glaucoma without increased IOP
Drops will be placed in your eyes to dilate (or enlarge) your pupils. The doctor will then use a special magnifying glass to check the color and shape of the optic nerve. He will also inspect for any damage or defects.
The ophthalmologist will measure the intraocular pressure as well as the thickness of the cornea. In addition, your doctor will test your visual field to look for any changes in the periphery that you may not notice.
Some people with normal-tension glaucoma have symptoms related to blood vessel problems, such as migraines, cold hands and feet, and low blood pressure.
With glaucoma of any type, circulation is disrupted, excess fluid accumulates, and there is an increased load on the optic nerve and other components of the visual organ.
There is also a disruption in the blood supply to tissues. These processes are determined through vision diagnostics - observation of the optic nerve and identification of negative changes. There are three ways to diagnose glaucoma without EDH. Let's take a closer look at them.
Method number 1. Ophthalmoscope
This procedure is carried out using a device for visual examination of the fundus of the eye. It's called an ophthalmoscope. The examination takes place in a dark office, where, using a light beam emanating from the device, the ophthalmologist examines defects in the visual organ through the pupil.
During the procedure, he determines the state of the disease by the shape and color of the nerve. If a curled nerve and a not very healthy pink tint are observed, a diagnosis is made: the disease is present and it is developing.
Method number 2. Test
The second way in which glaucoma is diagnosed in the presence of normal eye pressure is through a visual field test. Thanks to it, a map of the patient’s complete vision is established.
This test helps identify any area of vision loss resulting from damage to the optic nerve. Those changes that a person does not notice are determined using tested diagnostics.
Method No. 3. Differential diagnosis
There is another way to detect glaucoma without elevated IOP. Its essence is to conduct daily eight-hour monitoring of intraocular pressure. After all, the reason for the progression of open-angle glaucoma with normal intraocular pressure indicators is pronounced fluctuations in them.
And with the help of differential diagnostics, it is quite possible to identify peaks of “jumps” in pressure above normal (21 mm Hg).
With a normal level of intraocular pressure, primary open-angle glaucoma can progress, which is associated with pronounced fluctuations in this indicator during the day. Only by monitoring intraocular pressure can one determine the presence of peaks of ocular hypertension, at which the pressure exceeds 21 mmHg.
Open-angle and closed-angle glaucoma, normal-tension or low-tension glaucoma are all the most common forms of a very dangerous and irreversible eye disease - glaucoma or “blue clouding of the eye”.
If it is not diagnosed and treated in time, it will subsequently lead to blindness.
Diagnosis of normotensive glaucoma
To make a correct diagnosis of low-tension glaucoma, it is necessary to differentiate the disease from other types of glaucoma, for which pressure monitoring is carried out for 8 hours. Regular measurements of the level of intraocular pressure during such a study make it possible to detect peak-shaped pressure rises above 21 mm at the general normal level. Hg Art., which is one of the diagnostically significant features of normotensive glaucoma.
The most reliable and effective diagnostic method is optical coherence tomography of the optic nerve (OCT) in dynamics.
Treatment options for normal pressure glaucoma
Although the damage caused by glaucoma cannot be cured, your doctor will try to stop the worsening and slow or prevent vision loss.
He may prescribe eye drops, suggest laser treatment, or talk to you about surgery. Initially, pharmaceutical drugs are used to treat the organs of vision, and only if their action does not have the desired effect, doctors recommend surgery. Medications mainly include eye drops, the purpose of which is to reduce intraocular pressure.
Locally acting drugs are also used, which not only reduce ophthalmotonus, but also improve blood flow to the eyes and normalize metabolic processes in the eye tissues.
With the help of drops, eye tension is reduced to approximately 30%, and if you do not allow it to increase again, the glaucoma stabilizes and vision becomes better. When glaucoma is a consequence of another disease, both diseases are treated simultaneously.
When drug therapy does not help, the patient is recommended to undergo surgery. It can be of two types: using laser and eye microsurgery.
Like other types of glaucoma, normal tension glaucoma is treated in two ways:
Drug therapy
In addition, prostaglandin analogues help reduce the level of intraocular pressure precisely in this type of glaucoma, that is, against the background of normotension.
Systemic calcium channel blocking drugs, such as nifedipine, are usually prescribed to young people at the initial signs of the disease. Peripheral vasospasm is first diagnosed using capillaroscopy.
The effectiveness of such therapy will remain for a long time only if perimetry does not show negative dynamics during the first 2-3 months of treatment.
If daily monitoring of the level of intraocular pressure reveals a significant decrease in it at night, then the evening intake of antihypertensive drugs should be discontinued.
The most popular drug for glaucoma without increased intraocular pressure is Betaxolol. As mentioned earlier, with glaucoma without intraocular eye pressure, “jumps” in intraocular pressure may occur during the day.
Treatment with medications is aimed at stabilizing this pressure. In addition, it blocks further damage to the optic nerve, due to which the condition returns to normal.
The most popular drug for glaucoma without increased intraocular pressure is Betaxolol.
Taking this medicine promotes active nutrition and blood supply to the nerve. Thanks to this drug, as well as prostaglandin analogues (Xalatan, Travatan), IOP decreases precisely in this type of glaucoma, that is, against the background of normotension.
Also, if initial signs of the disease are detected, systemic drugs that block calcium channels are prescribed. These include "Nifedipine". But such medications are recommended mainly for young people.
How effective such therapy will be, and how long the effect of taking the drugs will last, depends on the presence or absence of negative dynamics during perimetry. If it is not observed within 2-3 months, it means that the disease has stopped and this method of treatment can be used further.
Only patients who show progressive visual field changes require treatment. First of all, using the following methods, intraocular pressure is reduced by 30% from the initial level:
- Betaxolol has a hypotensive effect. It is also the first choice drug for improving blood supply to the optic nerve. Prostaglandins have a more pronounced hypotensive effect in eyes with normal blood pressure.
- If there is a tendency towards progressive deterioration of visual fields, then, despite low levels of intraocular pressure, trabeculectomy is performed on at least one eyeball.
- In the initial stage of the disease, as well as in young patients, systemic calcium channel blockers, for example, nifedipine, are prescribed. Before starting treatment, peripheral vasospasm is diagnosed using capillaroscopy.
- Daily monitoring of blood pressure is carried out. If nocturnal hypotension is detected, it becomes necessary to discontinue taking antihypertensive drugs before bedtime.
Symptoms of glaucoma
To prevent the negative consequences of IOP, you need to be examined by an ophthalmologist on time.
Due to the absence of symptoms for a long time, glaucoma is difficult to diagnose in the initial stages. Often the first signs of an onset of illness are blurred and are attributed to other diseases.
For timely detection of the disease, you should be regularly examined by an ophthalmologist. Changes in intraocular pressure are difficult to notice by yourself.
When symptoms are detected on your own, the disease is often already in a very advanced state. The table shows signs of increased and decreased intraocular pressure.
Open-angle glaucoma and normal-tension glaucoma are characterized by the absence of symptoms. If a drop in ophthalmotonus occurs over a long period (several years), the only sign of the disease is a gradual decrease in vision.
With inflammation, dehydration and infections, a sharp decrease in pressure occurs. The patient's eyes dry out and lose their shine, and sometimes the eyeballs become sunken.
Sharp pain in the eyes is a symptom of angle-closure glaucoma.
The eyeball is a spherical body that consists of a hard shell and liquid contents.
Maintaining a correct, spherical shape, supply of nutrients, and normal functioning of the vision system is ensured by a certain level of intraocular pressure. In this article you will learn about the symptoms of changes in eye pressure and methods of treating it. Eye pressure is normal with balanced outflow and flow of fluid into the eyeball.
The pressure created by the vitreous body and intraocular fluid on the sclera and cornea is called ocular pressure. You can feel it by pressing your finger through the eyelid to the eye.
Quite often there is confusion between the concepts of fundus and eye pressure. These are completely different concepts, so there is no need to confuse them.
Eye pressure
Both adults and children have almost the same level of pressure. It is measured in millimeters of mercury.
The normal level is considered to be from 17 to 27 mm. Hg
Art. During the day, slight deviations in the indicator are possible. In general, the rates in the morning and afternoon are slightly higher than at night and in the evening.
There may also be a difference in the readings in the eyes, but normally it should not exceed a level of up to 5 mm. Hg
Art.
There are two main forms of glaucoma.
To prevent the negative consequences of IOP, you need to be examined by an ophthalmologist on time.
- blurred vision;
- rare blinking;
- atrophy and retraction of the eyeball;
- lack of shine;
- change in field of view.
- pain in the forehead, throbbing in the temples, migraine;
- destruction of the vitreous body;
- severe pain, stinging in the eyes;
- deterioration, blurred vision;
- decreased peripheral vision and field of vision;
- blurry rainbow circles when looking at the light;
- worsening dark adaptation, tearfulness;
- heaviness, fatigue in the eye sockets;
- redness of the eyes.
With this type of disease, intraocular pressure is usually 16-19 mm Hg. Art., in some cases it can decrease to 15 mm Hg.
Art. and below. As a rule, the higher the level of intraocular pressure, the more severe the damage to the optic nerve.
The picture of pathological changes in the area of the optic nerve does not differ from those in ordinary open-angle glaucoma, accompanied by an increase in intraocular pressure.
In normal pressure glaucoma, visual field defects are usually more pronounced and localized closer to the central region. Sometimes pathological changes of this kind do not progress even in the absence of proper treatment.
But because glaucoma with low intraocular pressure is diagnosed late, damage to the optic nerve is often significant. The probability of developing negative changes in the fellow eye over a five-year period is 40%.
Laser treatment
Has a varied character. In one case, a laser is used to create a hole for better movement of fluid inside the chambers of the eye, which helps reduce pressure.
This type of operation is used to eliminate angle-closure glaucoma, after first reducing the pressure with medications. Another type of laser intervention is the removal of blockages in drainage channels, which restores the outflow of fluid.
The operation lasts about 20 minutes, but to get the full effect you will have to wait several weeks.
Operation
If medications and laser treatments have no effect on your eye pressure, your doctor may talk to you about surgery.
There is a procedure called trabeculectomy, which creates a hole in the white (or sclera) of the eye to allow fluid to drain out. Or a drainage tube may be implanted to lower the pressure.
Researchers are working to find the best treatment for normal-tension glaucoma that will help protect the optic nerve and improve blood flow.
Microsurgery also has several intervention options. One of the most common is to remove a small part of the blocked drainage system of the eye chamber and create a bubble for new drainage of eye fluid, which reduces the pressure inside the eye.
They also use a method of implanting a device into the eye to improve the outflow of ocular fluid. Removal of part of the sclera is considered not the most effective operation. As a result, the intraocular fluid flows through a small amount of tissue remaining.
Only those patients who have registered progressive changes in visual fields require medical intervention. At the same time, they try to reduce the level of intraocular pressure by a third of the initial values.
Performed only on patients with documented progressive changes in visual fields. It consists of reducing intraocular pressure by 30% of the initial level.
If the medication method does not produce noticeable results, then resort to the help of a surgeon. Basically, the patient is offered to undergo trabeculoplasty. It is performed using a laser by photocoagulation of the trabecular network of the visual organ.
This type of surgery is also performed for other types of glaucoma, when medications are unable to cope with high blood pressure.
The operation is carried out as follows:
- The laser beam is projected onto the trabecular meshwork of the eye (which is a moisture filter), thus applying pinpoint coagulants.
- The laser creates additional holes in the trabecular area, which facilitate the rapid “flow out” of fluid.
As for the issue of self-medication of glaucoma at home, it can only be done with the permission of the attending physician. To ensure that the condition is stable and does not worsen, it is necessary to strictly follow the prescribed instructions. It is not advisable to experiment with pharmaceutical drugs, as well as with folk remedies.
Mechanism of fluid synthesis/outflow
Moisture is produced by the processes of the ciliary body and accumulates in the cavity of the posterior chamber. Most of it is directed through the lumen of the pupil into the cavity of the anterior chamber. After this, it is filtered by the drainage system, passing through the trabeculae/Schlemm's canal. After them, the liquid is discharged through collectors further into the superficial vessels of the sclera. This completes the fluid migration cycle.
To assess the quality of the drainage system, gonioscopy is practiced. The specialist can find out the patency of the trabecular system and Schlemm's canal, including the width of the anterior ocular chamber. The information obtained allows us to establish the clinical form of glaucoma. In the case of open-angle, all components of the angle of the anterior eye chamber are visible. In the case of a closed-angle form, it is difficult to analyze the state of the anterior chamber.