Reasons for formation
But, unfortunately, the nature of the development of the disease is unknown. The following categories of patients are susceptible to membrane proliferation:
- after ophthalmic surgery, which results in scarring;
- with pathological processes in the blood vessels of the eyes;
- with hypertension;
- with injuries to one of the eyes;
- with this disease in the left or right eye.
Most often, concomitant eye diseases serve as a provoking factor for the appearance of fibrosis:
- diabetic retinal damage;
- thrombosis of the central retinal vein;
- vitreous detachment;
- high degree of myopia (myopia);
- various inflammatory processes.
It should be borne in mind that sometimes, a membrane forms for no apparent reason in completely healthy people.
Most often, cases of epiretinal membrane development are idiopathic in nature, that is, the connection between the onset of the disease and any factors cannot be traced. It has been noted that patients with concomitant ophthalmological diseases are somewhat more susceptible to this pathology:
- retinal tears and detachment;
- vitreous detachment;
- diabetic retinopracy;
- thrombosis of the central retinal vein and its branches.
In addition, inflammatory diseases and hemorrhages in the tissues of the eye can provoke the formation of scar tissue on the surface of the macula. When examined, the epiretinal membrane contains cells of the retinal pigment epithelium and vitreous body, as well as collagen, fibrocytes, and macrophages.
Epiretinal membrane is more often formed in patients with fundus pathology, including vitreous detachment, diabetic retinopathy, retinal rupture, thrombotic complications (central vein thrombosis).
Also, inflammation and hemorrhage into the substance of the eye can lead to the formation of an epiretinal membrane. However, often the cause of the formation of the epiretinal membrane cannot be established, that is, the disease is idiopathic in nature.
The epiretinal membrane contains vitreous cells, macrophages, retinal pigment epithelial cells, fibrocytes and collagen cells.
Epiretinal membrane - the most effective treatment methods, experienced doctors, the best conditions and price
Causes Symptoms Diagnostics Treatment Our advantages Treatment price
Epiretinal membrane is a slowly progressive pathology that usually occurs over the age of 65-70 years.
The membrane is a thin whitish film that forms in the posterior part of the eyeball, namely, in the thickness of the vitreous body in the immediate vicinity of the macula.
As pathological changes progress, the thin, delicate film gradually turns into dense scar tissue, tightening the retina and causing swelling of the tissue in the macula, and sometimes tension, followed by rupture or detachment of the retina.
Causes
Most often, this formation is found in elderly people suffering from other eye diseases, such as diabetic retinopathy, myopia, destruction of the vitreous body, thrombosis of the central retinal vein, etc. In some cases, epiretinal membrane occurs for no apparent reason, i.e. is an idiopathic pathology.
Advantages of the “Moscow Eye Clinic”
To treat and diagnose eye diseases, the clinic uses the most accurate equipment and effective methods recognized by leading clinics in the world. The level of training of the clinic’s specialists allows for interventions of any level of complexity. The Moscow State Conservatory employs recognized world-class specialists, professors and doctors of science with extensive practical experience.
The clinic deals with the treatment of epiretinal membrane and other operations on the posterior segment of the eye, candidate of medical sciences, vitreoretinal surgeon Oleg Evgenievich Ilyukhin.
Over the years of professional activity, he has successfully performed thousands of complex vitreoretinal operations. Dr. Ilyukhin has repeatedly completed specializations in leading domestic and foreign eye clinics.
Operations are also performed by a surgeon of the highest category, the chief physician of the clinic, Fomenko Natalya Ivanovna, who has successfully performed more than 12 thousand operations of various categories of complexity.
The doctors of the Moscow Eye Clinic provide all the necessary assistance seven days a week, from 9 to 21 hours, seven days a week. During treatment, preference is given to minimizing the number of visits and performing outpatient procedures whenever possible.
Epiretinal membrane treatment cost
The cost of treatment consists of diagnostic studies, the volume of therapeutic manipulations and procedures, which is selected individually for each specific patient. Prices for medical services at MGK are affordable and fixed in the contract. The cost of diagnosis and treatment of eye diseases can be found here.
We work for you seven days a week, seven days a week, from 9 a.m. to 9 p.m. You can ask our specialists any questions you have by calling the MGK hotline 8(800)777-38-81 (free for mobile phones and regions of the Russian Federation) and the number in Moscow 8(499)322-36-36 or online, using Skype consultation on the website.
Source: https://mgkl.ru/uslugi/epiretinalnaya-membrana-glaza
Stages of the disease
There are several stages of this pathology in medicine. The first is automatically divided into two periods:
- The peculiarity of the first is that a small yellowish spot is formed inside the central fovea on the inner side in the fundus of the eye.
- The characteristic of the second is the formation inside the central fossa on the surface of a flat contour, reminiscent in its outline of a circular field or circle.
So, it follows from this that the primary stage consists of a violation of the structure of the retina, reaching a size of 400 microns. The second acts as changes having more than 400 microns. But the third one is capable of forming Weiss rings.
Causes of the disease
By origin, ERM can be idiopathic (of unknown origin) or secondary. In the latter case, the formation of a fibrous film has the nature of a concomitant pathology and can accompany such eye diseases as:
- uveitis;
- blunt and penetrating eye injuries;
- retinal tears;
- vascular diseases of the retina;
- oncological formations;
- diabetic retinopathy;
- retinal detachment;
- hemorrhage into the vitreous body.
In most cases, epiretinal membrane is idiopathic and has no connection with other eye diseases. The reason for the formation of a film on the surface of the macula in this case is natural (most often age-related) changes in the structure of the vitreous body, which lead to the release of cells from the retina and pigment layer into its cavity. As they settle on the macula, they begin to secrete collagen fibers, forming the ERM.
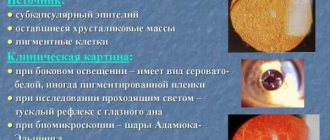
Clinical picture during the development of the epiretinal membrane
The epiretinal membrane is sometimes related to the development of certain pathologies, for example, one of the forms of complications of diabetes mellitus that affects the vessels of the retina, vitreous detachment, retinal tissue defect, obstruction of the central retinal vein and its branches, etc.
Inflammatory processes and occasional hemorrhages can contribute to the formation of a cellophane macula. However, in most diagnosed cases, it is not possible to establish the cause of the appearance of such an eye tumor.
It was revealed that the cellophane macula contains cells of the vitreous body, pigmented skin, macrophages, fibrocytes, and collagen cells.
Epiretinal membrane, or cellophane macula
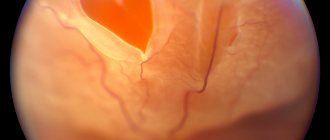
The epiretinal membrane is a thin, transparent film that forms directly above the central region of the retina, the macula. A macula with an epiretinal membrane is also called a cellophane macula because when examining the fundus, the central zone of the retina looks like a wrinkled cellophane film.
At its core, the epiretinal membrane is scar tissue that tightens the retina, causing folding and wrinkling. It is important to note that damage to the photoreceptor cells in the retina that sense light does not occur until the membrane progresses to become thick and rigid, causing retinal edema, fibrotic changes, and in some cases, retinal rupture followed by detachment.
It is usually a slowly progressive disease that occurs in people over 65-70 years of age. Women and men suffer from this pathology equally often.
Reasons for the formation of the epiretinal membrane
The formation of an epiretinal membrane may be associated with the presence of any eye disease in the patient - diabetic retinopathy, vitreous detachment, retinal rupture, thrombosis of the central retinal vein and its branches, etc. Inflammatory processes and hemorrhages can stimulate the formation of the epiretinal membrane. However, in a large number of cases, the epiretinal membrane is idiopathic, that is, of unknown origin. It has been established that the epiretinal membrane contains cells of the vitreous body, retinal pigment epithelium, macrophages, fibrocytes, and collagen cells.
Clinical signs
Because the epiretinal membrane lies above the macula, central vision is affected. As a rule, one eye is affected. There is blurred vision and distortion of the image - straight lines look curved and wavy, there may be double vision, which persists even when the other eye is closed.
Diagnosis of epiretinal membrane
Epiretinal membrane is diagnosed by examining the fundus of the eye - ophthalmoscopy. It shines and resembles cellophane film in appearance. In the initial stage, the thin epiretinal membrane may not be visible. The diagnosis can be confirmed using an ultrasound examination of the eye, which is especially important when the fundus of the eye is not visible due to clouding of the optical media of the eye - the cornea, lens or vitreous body. Optical coherence tomography allows you to accurately determine the size and structure of the membrane; using fluorescein angiography, you can clarify the degree of retinal edema in the central zone.
The effect of epiretinal film on vision is determined using the Amsler grid, when viewed from which straight lines appear curved and wavy.
Treatment
Treatment for epiretinal membrane involves surgical removal. The operation is performed only in cases of severe reduction and distortion of vision, when the risk of possible irreversible damage to the central zone of the retina as a result of the operation is comparable to the visual acuity available before the operation. First, vitrectomy is performed - removal of the vitreous body, then the membrane itself is removed. If the operation was successful, then in 80-90% of cases, over the course of several months, vision gradually improves by 20% or more.
Potential complications of surgery may include: infection, increased intraocular pressure, retinal hemorrhage, detachment, and progression of cataracts. Re-formation of the epiretinal membrane occurs in approximately 10% of operated patients.
There is no prevention of epiretinal membrane formation as such. The only measure may be a periodic scheduled visit to an ophthalmologist, if in general nothing bothers you, and a mandatory examination of the fundus every 6 months if there is a history of any eye diseases - thrombosis, diabetic retinopathy, etc.
The epiretinal membrane is a thin and transparent film that is located above the central zone of the retina. Due to the structural features of the epiretinal membrane in the macular area, it is called the cellophane macula. This is due to the fact that during ophthalmoscopy, the central region of the retina in appearance resembles a wrinkled cellophane film.
By its structure, the epiretinal membrane is scar tissue that tightens the retinal substance and leads to the appearance of wrinkles and folds. It is important to note that the photoreceptors responsible for the perception of light are not damaged until the membrane becomes very hard and thick. As a result of this progression of the disease, retinal edema, fibrous transformation, and sometimes retinal rupture or detachment occur.
This disease usually progresses quite slowly. Patients aged 65-70 years are more likely to get sick. The occurrence of epiretinal membrane does not depend on gender.
Clinical signs
Since the epiretinal membrane appears over a key area of the retina, much of the central vision is lost. Often such a lesion is unilateral, i.e. Either the right or left eye may be affected.
Almost always, when a cellophane macula appears, patients complain of blurred vision and the resulting distorted image. To such patients, straight lines may appear curved or wavy. There is a possibility of diplopia, i.e. double vision, which occurs even if the second eye is closed.
The epiretinal membrane is formed in the area of the macula, so mainly central vision is affected. Most often the defeat is unilateral. In this case, there is blurred vision, curvature of image lines, and sometimes there is diplopia, which does not disappear even when the second eye is closed.
In order to diagnose pathology, studies such as ophthalmoscopy, ultrasound, visometry, and fluorescein angiography are necessary. The epiretinal membrane looks like a shiny cellophane film.
At the initial stages of development it is not always possible to detect it. In order to confirm the development of pathology, it is necessary to do an ultrasound examination of the apple of the organ of vision.
This examination for diagnostic purposes should be carried out for the reason that due to clouding of the cornea, vitreous body or lens of the eye, it is not possible to examine the fundus of the eye during an ophthalmological examination.
The exact size and structure of the macula can be determined using optical coherence tomography. Fluorescein angiography makes it possible to determine the degree of swelling.
Vision in pathology
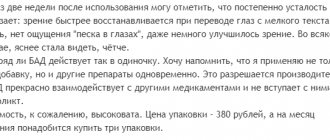
In the initial stage, macular epiretinal membranes appear as translucent, shiny membranes in or near the central macular area (Figure 2-1). A picture of a “pseudo-hole” in the fovea region is possible. As the membrane thickens, it becomes less transparent (Fig. 2-2, A). The epiretinal membrane may be accompanied by superficial hemorrhages or infarctions in the nerve fiber layer.
Epiretinal Membrane + Reliable Treatment Method (2020) in Kyiv: Prices
Epiretinal membrane (epiretinal fibrosis),
also commonly known as cellophane maculopathy. It is rough scar tissue that appears as shiny or cloudy membranes on the surface of the retina.
Most often, the formed membranes are asymptomatic and can remain undiagnosed for a long time. But they lead to a slow loss of vision and, in addition, can cause visual distortions of objects, in other words, metamorphopsia.
Symptoms of epiretinal membrane are more pronounced the stronger the impact on the macula, which is the central part of the retina and helps us distinguish small details.
It is thanks to the macula that we can read and recognize faces.
Symptoms of epiretinal membrane
Most people with epiretinal fibrosis have no symptoms. They learn about them by chance during examinations with an ophthalmologist. In particular, thanks to diagnostic methods such as optical coherence tomography (OCT).
In such cases, the person has normal or almost normal vision and does not understand what the threat is. However, the epiretinal membrane may slowly progress, resulting in visual distortions.
The patient can notice these visual distortions if he looks with his eyes alternately (first with the right and then with the left) - then he can be convinced that “something is wrong,” because with each eye the size, shape or distance to the object will be different.
But in order to track such symptoms, you need to at least suspect them or clearly know about the existence of the epiretinal membrane after confirmation by OCT.
- Visual distortions or metamorphopsia are usually expressed in a distorted vision of a form. For example, everyone knows that window blinds or the doors of any furniture are straight, but a person with epiretinal fibrosis may notice that they look “wavy” or “crooked” to her, especially when compared to other “right” objects up close.
- In common cases, epiretinal membrane symptoms manifest as significant vision loss.
Less commonly, epiretinal fibrosis may cause symptoms such as:
- Doubling or “blurring” of the contours of various objects
- Excessive sensitivity to light or bright images
- Objects appear smaller or larger than they really are.
Causes of epiretinal membrane
The most common cause of epiretinal membrane is a defect in the lining of the retina where glial cells are located. These cells are able to migrate and form a membrane on the surface of the retina, similar to cellophane. Over time, the membrane thickens and causes stretching or folding of the retina, leading to decreased vision and the development of metamorphopsia.
The risk of developing epiretinal fibrosis increases with age. Studies have shown that 2% of patients are people over 50 years of age.
And in 20% of patients diagnosed with cellophane maculopathy are people over 75 years of age. In people who are prone to eye diseases, this disease can be detected at an early age.
However, in this case, the most common cause is retinal detachment.
Risk factors for epiretinal membrane development
Cellophane maculopathy may also be associated with other processes and eye pathologies:
- Retinal detachment or tear
- Retinal vascular diseases such as diabetic retinopathy or retinal vascular occlusion
- Eye surgeries
- Injuries
- Inflammation (uveitis)
- If there is no separate cause, then the origin of the epiretinal membrane is called idiopathic (that is, for unknown reasons).
Epiretinal membrane affects both eyes at once in 10% -20% of cases. But, at the same time, in different eyes it can have different stages of development.
Diagnosis and detection of epiretinal fibrosis
Most cases of epiretinal membrane are diagnosed by ophthalmologists during a routine clinical examination. Optical coherence tomography is used to assess the severity of epiretinal fibrosis. To determine what causes the disease, additional studies are sometimes used, for example, fluorescein angiography.
The Clinical Ophthalmology Center offers services to solve vision problems
Because in most cases, epiretinal fibrosis is a fairly stable age-related process, so unless it significantly affects vision, the condition can be simply controlled. However, if examination shows progression and/or functional deterioration of vision, surgery may be recommended.
There are no eye drops, medications, or dietary supplements to treat epiretinal fibrosis. A surgical procedure called vitrectomy is the only treatment option.
During a vitrectomy, microscopic incisions are made in the sclera (the white part of the eye), and the glassy gel that fills the inside of the eye is replaced with saline.
This allows access to the surface of the retina and removal of the epiretinal membrane with delicate forceps. This helps the macula take its shape and straighten out the folds.
Factors influencing vision recovery after vitrectomy
- Duration of existence of macular fibrosis
- The degree of tension of the retinal membrane
The Center for Clinical Ophthalmology draws your attention! Surgery for cases of epiretinal fibrosis, without concomitant other ocular pathology, has a better prognosis than in cases with previous retinal detachment or retinal vascular diseases.
We want to reassure you that vitrectomy for the treatment of epiretinal fibrosis has a good success rate. Most patients after vitrectomy experience an improvement in visual acuity and a decrease in metamorphopsia. It is important not to waste time, but to undergo examination on time and agree to surgery if it is a necessary measure to preserve your vision!
Source: //cco.com.ua/poslugi/vitreoretinalna-hirurgiya/epiretinalna-membrana.html?lang=ru
Symptoms of the disease
The main signs of proliferation of the epimacular area are:
- sudden deterioration of vision;
- duality in one of the eyes;
- "veil" before the eyes.
Typically, one eye is affected first. If treatment of the epiretinal membrane of the eye is not carried out in a timely manner, then the disease progresses to the second.
There is a concept of primary and secondary degrees of the disease. As a rule, the primary form occurs in the latent phase for a long time.
As membrane proliferation progresses, the patient may experience swelling in the eye. If a retinal tear occurs, the patient may complain of the appearance of black spots in front of the eyes.
The latest manifestation is considered to be swelling of the macula in the eye. In this case, surgical intervention is inevitable.
Live video of the operation
In approximately 10% of cases, the epiretinal membrane appears again after surgery. There are no preventive measures to prevent its formation. However, people who have had surgery need to undergo routine examinations with an ophthalmologist every six months, even if there is no concern for the current period.
The specialists of our clinic have extensive experience in the surgical treatment of epiretinal fibrosis, including those with concomitant eye pathology. The skill of vitreoretinal surgeons and the latest modern equipment for the operating room allow us to minimize the risks of complications and guarantee each patient the best possible postoperative results.
Diagnostics
Membrane proliferation can be diagnosed by examining an ophthalmologist who will perform ophthalmoscopy, ultrasound and other examinations of both eyes of the patient.
Visualization using ophthalmoscopy helps to identify the disease due to the characteristic luster of the membrane, which is why it is also called “cellophane retinopathy”.
If a patient is diagnosed with concomitant ophthalmological diseases in the form of cataracts or opacities, then an ultrasound examination is performed as an additional diagnosis. It is thanks to it that a hypoechoic type formation can be identified, its density and size can be determined.
If the eyes are swollen, fluorescein angiography is performed, which helps to identify possible changes in the membrane, the presence of blood clots and other abnormal processes in the retina.
In order to determine the extent to which the patient has lost vision, visometry is performed; intraocular pressure measurement is also a prerequisite. It is important to note that the disease affects both men and women equally.
Most often, a “cellophane macula” is detected during examination of the fundus. The film on the macula glitters and looks like crumpled cellophane.
However, in the early stages, it is quite difficult to diagnose it during ophthalmoscopy, since the layer of scar tissue is still thin and transparent. If pathology is suspected and an age factor is present in combination with appropriate symptoms, an ultrasound examination of the eye is prescribed.
It is all the more indispensable if the fundus of the eye is poorly visible, when there is age-related clouding of the optical media of the eye (lens, cornea and vitreous body). The following diagnostic techniques can also provide additional information:
- OCT (optical coherence tomography) – allows you to assess the size, structure and thickness of scar tissue;
- fluorescent tomography – makes it possible to detect macular edema of the retina;
- study using the Amsler grid - reveals the degree of influence of pathology on visual acuity (when examining the grid, straight lines appear curved to one degree or another depending on the severity of visual impairment).
Epiretinal membrane can be diagnosed by ophthalmoscopy. It has a characteristic appearance, glitters and resembles cellophane film.
In the initial stage of development of the epiretinal membrane, it may not be noticed. To confirm the diagnosis, an ultrasound examination of the eyeball is performed.
This diagnostic method is especially relevant for clouding of the transparent optical media of the eye (lens, cornea, vitreous body). Optical coherence tomography may be required to determine more precise membrane dimensions and structure.
Fluorescein angiography is performed to assess the degree of retinal edema in the macula area.
https://www.youtube.com/watch?v=kMlDsJ8mH3o
To determine the degree of influence of the epiretinal membrane on visual function, the Amsler grid is used. If the lines in the grid become curved instead of straight, then there is a visual impairment.
Treatment of epiretinal membrane of the eye always begins with a detailed diagnosis. Such a diagnosis should include not only an examination of the fundus by an ophthalmologist, as well as a detailed survey, but also ultrasound, autofluorescence testing, coherence tomography, and radiography.
Additionally, the patient may be scheduled for consultations with other specialists: cardiologists, therapists, neurologists.
The widest range of studies to identify the present pathology is used in the early stages of the disease, when the membrane remains quite thin, and it is almost impossible to discern it during examination of the fundus. The most important role in diagnosis in the cases presented is given by ultrasound examination of the eye.
If the membrane turns out to be stable and does not cause vision impairment for a long time, the patient may be prescribed general therapy, which involves the use of local agents, as well as general strengthening drugs.
Also, the patient will need to be constantly monitored by a doctor in order to promptly determine the progression of the membrane, since the doctor cannot guarantee the stability of such a formation for years to come.
The process of further deterioration of the patient's vision can begin at any time.
Diagnosis for suspected ocular membrane
Treatment of epiretinal membrane of the eye always begins with a detailed diagnosis. Such a diagnosis should include not only an examination of the fundus by an ophthalmologist, as well as a detailed survey, but also ultrasound, autofluorescence testing, coherence tomography, and radiography. Additionally, the patient may be scheduled for consultations with other specialists: cardiologists, therapists, neurologists.
The widest range of studies to identify the present pathology is used in the early stages of the disease, when the membrane remains quite thin, and it is almost impossible to discern it during examination of the fundus. The most important role in diagnosis in the cases presented is given by ultrasound examination of the eye.
If the membrane turns out to be stable and does not cause vision impairment for a long time, the patient may be prescribed general therapy, which involves the use of local agents, as well as general strengthening drugs. Also, the patient will need to be constantly monitored by a doctor in order to promptly determine the progression of the membrane, since the doctor cannot guarantee the stability of such a formation for years to come. The process of further deterioration of the patient's vision can begin at any time.
In the same case, if the patient’s membrane progresses and provokes permanent deterioration of vision, he will be prescribed surgical treatment. It involves vitrectomy of the vitreous, as well as further removal of the membrane. The cost of surgery for epiretinal membrane of the eye is determined individually for each patient, depending on the complexity of his case; the price for it in various clinics ranges from 25 thousand rubles to 130 thousand rubles.
It is important to know! An effective way to effectively restore vision, recommended by the country's leading ophthalmologists! …
The presented operation is successful in approximately 80% of cases. Some time after such a surgical intervention, a person’s vision is restored by approximately 20% (sometimes doctors manage to achieve better results with such a surgical intervention). Complications with such surgery are extremely rare, but can occur. These may be: the formation of cataracts in the operated eye, retinal detachment, infection in the tissue.
Treatment with folk remedies for the epiretinal membrane of the eye is not carried out, especially at those stages of the disease that are accompanied by significant deterioration of vision, double vision, and also curvature of the visible image. The use of traditional methods for this disease instead of timely surgical intervention can lead to complete irreparable loss of vision.
How to restore vision without surgery
We all know what poor vision is. Myopia and farsightedness seriously spoil life by limiting ordinary activities - it is impossible to read something, see loved ones without glasses and contacts. These problems begin to manifest themselves especially strongly after 45 years. When you are face to face with physical weakness, panic sets in and it is hellishly unpleasant. But there is no need to be afraid of this - you need to act! What means should be used and why is described..."
The epiretinal membrane is a thin, transparent film that lies just above the macula, the most sensitive area of the retina. The appearance of a membrane means the occurrence of a pathology called a cellophane macula. This name is by no means accidental: during an examination of the fundus, you can see that the macular region of the retina is like crumpled cellophane film.
Based on its structure, the membrane can be classified as scar tissue, tightening the retina into wrinkles and folds. This pathology does not affect light-sensitive receptor cells immediately after its appearance. Damage to the photoreceptors occurs only when the epiretinal membrane becomes rigid and thick enough to cause swelling of the retina. When the pathology develops to this stage it can also lead to fibrotic changes, in most cases leading to retinal rupture and detachment.
In most people suffering from this eye pathology, the disease develops very slowly. Cellophane macula affects people of both sexes equally often. As a rule, pathology begins to develop at the age of 65–70 years.
In many cases, the epiretinal membrane appears due to some kind of eye disease. For example, pathology can develop in connection with diabetic retinopathy, vitreous detachment, thrombosis of the central vein or its branches of the retina, retinal rupture and some others. Inflammation and hemorrhages inside the eye can also provoke the formation of a cellophane macula.
However, in the vast majority of cases, the epiretinal membrane is formed without any apparent reason that makes it possible to determine its nature, in medical terms, idiopathically. Studies of the structure of the cellophane macula have shown that it contains cells of various structures of the eye: the vitreous body, pigment cells of the retinal epithelium. The presence of collagen cells, fibrocytes and macrophages was also confirmed.
As we said above, the epiretinal membrane forms directly above the macula. Its manifestations are directly related to the location of the pathology. First of all, central vision deteriorates. Most often, only one eye is affected, only in rare cases - two eyes. In addition to the actual deterioration, patients note a distorted perception of images. Thus, straight lines may appear curved or wavy, or double, even if the other healthy eye is closed. A frequent accompaniment of pathology is blurred vision.
The main method to detect a cellophane macula to this day is ophthalmoscopy, that is, examination of the fundus of the eye. During examination, the epiretinal membrane is slightly shiny, like cellophane film. At an early stage of the development of the disease, it is very difficult to notice. If the ophthalmologist doubts the occurrence of this pathology, the patient is given a referral for an ultrasound scan to confirm or refute the ophthalmologist’s suspicions. Ultrasound examination is especially important if there are factors complicating ophthalmoscopy (opacity of the cornea, lens and/or vitreous).
To accurately determine the structure of the cellophane macula and its size, optical coherence tomography is used. The degree of retinal edema accompanying the disease can be determined using fluorescein angiography.
The effect of the epiretinal membrane on visual performance is tested using the Amsler grating test.
The epiretinal membrane cannot be treated conservatively; it can only be removed surgically. However, the decision to operate is made only in the case of severe deterioration/distortion of vision, and also if the risk of irreversible damage to the macula during surgery is high and comparable to the existing visual acuity.
First of all, during the operation, the vitreous body is removed (vitrectomy), after which the surgeon excises the membrane. The success rate of operations is 80–90 percent. When the eyes are restored, an improvement in vision is observed, sometimes reaching up to 20%.
Possible complications:
— infections;
- increased pressure inside the eye;
- hemorrhages on the retina;
- retinal detachment;
- rapid progression of cataracts.
Unfortunately, there is no prevention for this pathology. We can only advise you to undergo regular examination by an ophthalmologist, which includes checking the condition of the fundus.
The epiretinal membrane of the eye is a thin film that forms above the macula.
When examining such a pathology during the examination, it seems that there is cellophane on the retina.
For this reason, the disease has another, less well-known name - cellophane macula.
When exposed to a number of factors, above the macula - a thin sensitive zone of the eyeball - the structure of which is a transparent film.
Reference! This film consists of scar tissue, which, when tightened, causes the retina to wrinkle and wrinkle.
As a result, the photoreceptors of the eye are negatively affected , but it is possible to notice the consequences of these effects long after the development of the disease.
The membrane becomes rigid over time, and then retinal edema may occur.
This leads to damage to the photoreceptors, and subsequently, if left untreated, even retinal detachment and rupture are possible.
This disease occurs only in older people.
The average age of patients with epiretinal membrane is about 70 years, and the pathology is equally likely to develop in both men and women.
Progressing over time, such a pathological neoplasm can lead to loss of vision, but with timely treatment such consequences can be easily avoided.
First of all, the disease is characterized by such a subjective symptom as blurred vision.
Depending on the stage of the disease, it can drop quite noticeably. Usually only one eye is affected .
The following signs affecting the affected organ of vision are observed:
- the appearance of flashes and lightning before the eyes;
- the presence of scotomas (areas of loss of the visual field);
- spots before the eyes;
- there may be a feeling of fog or veil obscuring the view;
- distortion of the contours the objects in question ;
- Sometimes patients experience double vision .
If such symptoms are present, urgent examination and subsequent treatment are required.
In general, this disease is considered relatively safe and does not require emergency surgery.
But the sooner the procedures begin, the higher the likelihood of complete restoration of impaired vision.
Cellophane macula is not an independent disease, but a formation that occurs as a result of certain ophthalmological defects and diseases.
These include:
- detachment in the vitreous region;
- diabetic retinopathy;
- retinal tears;
- thrombosis in the blood vessel system of the eye.
Attention! But the pathology is not always due to these reasons, and most often membranes of an idiopathic nature are diagnosed (a neoplasm whose origin cannot be explained).
In them, in addition to the scar tissue itself, one can often find particles of the vitreous body and retina, as well as a small amount of collagen cells, fibrocytes and macrophages.
The only way to treat this pathology is surgery.
Conservative medicine is inappropriate in this case.
Also, any traditional medicine ineffective against the disease
The operation usually requires certain indications: if vision does not deteriorate during the formation of the membrane, such an intervention is not performed.
If the quality of vision deteriorates and there is a threat of irreversible changes in the “macula,” vitrectomy is performed.
This is the process of removing the diseased vitreous followed by the process of excision of the membrane.
This operation is considered simple , and in nine cases out of ten it is successful.
During recovery after such an intervention, significant restoration of vision is possible, the quality of which can sometimes reach twenty percent.
It is important to know! The cost of such an operation, unlike many other procedures, can vary significantly. It depends on the region, the degree of “eliteness” of the clinic, the qualifications of the doctor and the availability of modern equipment.
The cheapest operations to remove the epiretinal membrane range from 25-30 thousand rubles. The maximum cost of such a procedure can be almost 90,000 rubles.
On average, you should expect a price within 60,000 rubles (all prices are indicated for one eye).
Mainly, the disease can be diagnosed after undergoing an ophthalmoscopy procedure .
During such an event, a detailed examination of the fundus of the eye is performed, and if an epiretinal membrane forms on the vitreous body, it is easy to notice by its characteristic shine, similar to the shine of a plastic bag.
But the disease can be detected in this way in the later stages of its development, since in the initial stages such shine is absent.
If it is not possible to diagnose the disease using ophthalmoscopy, but there is a suspicion of this particular pathology, an additional ultrasound of the eyeball can be performed.
This procedure is also performed if, due to opacities that form on the lens, cornea or vitreous body, it is difficult to view the membrane.
Carefully! Opacities can affect one or more elements and can occur in all three organs - in such situations, ophthalmoscopy becomes ineffective.
As soon as the ophthalmologist determines the presence of a membrane, it is necessary to determine its structure and find out its size. This is necessary to prescribe optimal treatment and is performed by performing coherence tomography.
If swelling appears on the retina as the disease progresses, the degree of its intensity can be determined by performing fluorescein angiography.
Additionally, the patient must undergo an Amsler test to determine the effect of the membrane on the quality of vision.
The disease requires mandatory treatment , since if the membrane is ignored, complications such as:
- increased intraocular pressure;
- retinal detachment;
- the appearance of rapidly progressing cataracts;
- hemorrhages affecting the body of the retina.
In the video you will see a presentation on the topic of types of epiritinal membranes:
It is impossible to talk about measures to prevent the disease, since at present all the factors influencing the development of the membrane have not been established.
The only thing ophthalmologists can advise is to undergo regular examinations, especially for people over 40 years old (they need to visit a specialist at least 1-2 times a year).
The epiretinal membrane is a loose, colorless film located above the main area of the inner lining of the eye and is called the macula or cellophane macula. In essence, this is a kind of scar structure that tightens the retina and provokes the formation of folds and wrinkles.
It must be emphasized that the epiretinal membrane protects the photoreceptor cells responsible for the susceptibility of light rays. The protection of these cells is provided by the designated membrane until, due to the development of pathological changes, it acquires a thicker and more rigid structure, which provokes swelling of the retina of the organ of vision, as well as fibrous deviations, which in a certain situation causes a rupture of the retina with its further detachment.
In fact, the pathology is one of gradually progressive ones, occurring mainly in elderly patients from 65 to 70 years old. Both men and women are susceptible to pathology.
The epiretinal membrane is sometimes related to the development of certain pathologies, for example, one of the forms of complications of diabetes mellitus that affects the vessels of the retina, vitreous detachment, retinal tissue defect, obstruction of the central retinal vein and its branches, etc.
Inflammatory processes and occasional hemorrhages can contribute to the formation of a cellophane macula. However, in most diagnosed cases, it is not possible to establish the cause of the appearance of such an eye tumor.
It was revealed that the cellophane macula contains cells of the vitreous body, pigmented skin, macrophages, fibrocytes, and collagen cells.
Epiretinal membrane
Treatment
When making such a diagnosis, patients are interested in whether it is necessary to remove the epiretinal membrane. What consequences can there be for the eye, how is the operation performed? In most cases, doctors recommend removing the epiretinal membrane.
However, it is worth noting that surgery is performed only in case of severe deterioration of vision and the possibility of complications. The most popular method is vitrectomy, during which the vitreous body and areas of membrane proliferation are removed.
Removal of the epiretinal membrane without vitrectomy is impossible. After removal of the vitreous body, a section of the membrane is excised, the retina of the eye is freed, and the patient begins to see better.
This operation is not complicated, it is performed under local anesthesia, and the patient is sent home the same day. After surgery, the patient must be prescribed special anti-inflammatory and antimicrobial eye drops, which help relieve swelling and possible inflammation during the rehabilitation period.
It is important to note that the removal of the vitreous body occurs subject to the presence of the patient’s own lens in the eye. If the lens is foreign, then it is removed to prevent the development of adhesive processes. Is it possible to perform retinal coagulation after excision of a scarred area on the membrane? Yes, laser coagulation helps strengthen the retinal walls and improve the healing process.
Due to the fact that the drugs used to treat cellophane macula have a strong toxic effect on the organ of vision, preference today is given to surgical intervention. Indications for surgical intervention include an excessive decrease in visual ability and a high risk of injury to the central region of the retina.
The operation at stage 1 is limited to a procedure such as vitrectomy, during which the posterior and central parts of the vitreous are removed, provided that the patient has his own lens. If the patient does not have a lens or it is artificial, then an additional resection of the anterior region of the vitreous body is performed along with an artificial lens.
At the 2nd stage of the surgical intervention, the epiretinal membrane is excised, during which it is slightly lifted, taking it by the outer edge, above the inner membrane of the eyeball.
To remove the cellophane macula, thin tweezers are used. The limiting inner membrane is stained with special dyes before excision. Finally, a thorough examination is carried out to identify possible damage to the retina.
As a rule, the operation is performed as planned. However, if severe swelling of the macula is observed, then hospitalization and urgent surgery are necessary.
There are no preventive measures to prevent the occurrence of epiretinal membrane. Preventive measures of a nonspecific nature are aimed at eliminating the pathogenetic mechanisms of development and consist of monitoring hormonal balance, preventing thrombosis and embolism, as well as observing safety rules during the production process.
After surgery, patients must be examined by an ophthalmologist at least 2 times a year. This is necessary because 10% of patients experience a relapse of the pathology.
If you diagnose the disease in a timely manner by visiting your doctor for examination and undergo surgery, the prognosis for curing the disease will be favorable. Moreover, in case of severe loss of visual acuity, the treatment received will only partially restore it.
Epiretinal fibrosis progresses rather slowly, so its treatment depends directly on the degree of the disease and the general condition of the body. If the patient’s visual acuity remains within normal limits, then it is enough to periodically be observed by an ophthalmologist to monitor for possible visual impairment.
Drug therapy, as well as treatment with folk remedies, can only support general eye health, but do not get rid of the epiretinal membrane. But, first, before prescribing any medications, a number of diagnostic studies such as ophthalmoscopy, visometry and tonometry are still carried out.
Additionally, doctors can send the patient for an ultrasound examination, OCT, which stands for optical coherence tomography, or a fluorescein angiography procedure.
As mentioned above, despite the complexity of the operation, most patients respond positively to this treatment.
“I’ve had myopia since I was young, I wasn’t even accepted into the army. Although, in general, my health is good. At the age of 72, I felt that my vision began to decline again, and double vision appeared. Doctors diagnosed him with epiretinal fibrosis of the left eye. They said I had to operate, otherwise I would go blind. Of course, at first I refused, because of my age.
Epiretinal membrane can only be treated surgically. Surgery is indicated only in case of significant loss of visual acuity.
At the same time, it is worth taking a serious approach to assessing possible risks. If the loss of visual function significantly affects the quality of life, then the risk of surgical treatment can be considered justified.
However, it should be taken into account that with surgical removal of the epiretinal membrane, the likelihood of loss of central vision and the development of the following complications is quite high:
- infection;
- increased IOP;
- hemorrhages, ruptures and retinal detachment;
- development of cataracts.
The surgery involves a vitrectomy (removal of the vitreous) followed by removal of unwanted scar tissue. In the case of successful removal, in the vast majority of cases, vision improves by 20 percent or more.
In 10% of cases, after successful removal of the membrane, it forms again. Unfortunately, due to its unclear genesis, there are no effective measures to prevent such developments.
It is recommended to undergo a preventive examination with an ophthalmologist twice a year. In the presence of ophthalmological diseases (especially diabetic retinopathy and thrombosis of the ocular veins), as well as over the age of 60 years, it is necessary to include an examination of the fundus in the appointment plan.
The only way to remove the epiretinal membrane is to perform surgery. Surgery should only be performed in cases of severe distortion or decreased visual function. In this case, the risk of irreversible damage to the retinal macula during surgery and the vision that was available at the time of the proposed intervention should be assessed.
At the first stage, a vitrectomy is performed, that is, the vitreous substance is removed. Only after this the membrane is removed. With successful surgical intervention, most often (80-90% of cases) visual function gradually improves (by 20 percent or more).
Medicines have a toxic effect on eye tissue, so only surgical treatment is permissible.
The operation begins with vitrectomy. During surgery, the posterior and medial parts of the vitreous tissue are removed. When the patient does not have a lens or it is replaced by a prosthesis, an additional stage of the operation is resection of the anterior part of the vitreous.
The second stage of the operation is to rid the patient of the cellophane macula. During its course, the film is picked up by the outer edge and rises slightly above the internal tissues of the eye. To remove the tumor, the surgeon uses tweezers. The inner border part of the film is cut off. Before this, it is marked with special coloring compounds.
The final stage of surgical intervention is a revision of the condition of the fundus. Its task is to detect defects in the retina on its back or peripheral areas. If tissue detachments that are not complicated by the presence of exudate in the subretinal cavity are detected, the retina is glued to the vitreous body. This is done using laser retinopexy or cryoretinopexy.
Typically, removal of the epiretinal film is planned. However, if the patient’s macula is severely swollen, the patient is hospitalized with immediate resection of the pathological tissue.
Surgical therapy does not affect the clinical picture of the disease. Based on this, sometimes with the proliferation of pathological cells, the epiretinal film can grow again.
Preventive measures
Epiretinal membrane of the eye: treatment, how the operation is performed
Epiretinal membrane (premacular fibrosis, macular fold) is an ophthalmological pathology in which a thin transparent film is formed in the area of the macula (the central zone of the retina).
The macular area covered with this film is commonly called the cellophane macula. This name arose as a result of the similarity of the central part of the retina of the eye with wrinkled cellophane film.
Premacular fibrosis is usually diagnosed in people over 60 years of age and is accompanied by significant visual impairment.
Diagnosis and treatment
To diagnose the problem, it is necessary to consult an ophthalmologist when the first signs of the disease occur. In the initial stages of development, the transparent film is so thin that it is quite difficult to notice. To detect the epiretinal membrane, the first step is to examine the fundus, during which a characteristic shine can be noticed.
To confirm the diagnosis and identify the characteristics of the development of pathology, it is additionally necessary to carry out the following research methods:
- Ultrasound of the eyeball;
- coherence tomography;
- fluorescein angiography;
- perimetry;
- tonometry;
- biomicroscopy;
- visometry;
- Amsler test.
Once the pathology has been detected, it is necessary to carry out effective therapy. If the cellophane macula is secondary, then the first step is to cure the underlying disease. If visual impairment is minor and there are no complications, then treatment is not carried out. In this case, it is enough to be regularly examined by an ophthalmologist.
In severe cases, when vision is significantly reduced or distorted, surgery is performed. How is the operation done? Surgical treatment is carried out in 2 stages:
- Removal of the vitreous body (vitrectomy).
- Removal of the epiretinal membrane.
Surgical treatment is carried out only in extreme cases, after first assessing the risk of irreversible damage to the macula during the operation. With successful surgical intervention, vision is restored by more than 20% in 90% of cases.
Possible complications after surgery and its price
If the retina grows or changes, the membrane is removed surgically. To date, vitrectomy is the only effective treatment method.
The operation takes place in several stages. First, microsurgeons perform a revision of the operable area, then, using several incisions, they perform vitrectomy (removal of vitreous glass). And only then do they begin to excise the membrane itself. Its outer edge is lifted with a tool and then carefully removed.
Important! The removed vitreous is replaced with a special compound, usually silicone oil. To avoid infection, antibiotics are injected into the eye and a sterile dressing is applied over the eye.
Prevention of the appearance of epiretinal membrane
No special preventive measures have been developed to prevent the formation of a cellophane membrane.
However, patients diagnosed with this ophthalmological disease should be regularly examined by a doctor.
Epiretinal membrane is an ophthalmic disease that most often occurs in old age, progresses slowly and is not treatable with medication. If the quality of vision decreases to 0.1-0.2 or another need for surgery arises, there is a significant risk of complications in the form of retinal breaks, progression of cataracts and intraocular bleeding. After surgery, vision improves by 20% or more.
The epiretinal membrane of the eye is a thin film that forms above the macula.
When examining such a pathology during the examination, it seems that there is cellophane on the retina.
For this reason, the disease has another, less well-known name - cellophane macula.