Causes
The retina consists of 10 layers, thanks to which the visual image is formed. Retinoschisis is a pathology in which retinal separation occurs. As the disorder develops, fluid begins to accumulate between the layers of the retina, which separates the retina, causing vision problems. The development of the problem occurs due to circulatory disorders, which is provoked by:
- the presence of hereditary and congenital diseases;
- degenerative pathologies of the retina;
- problems with the vascular system;
- the presence of eye injuries;
- other eye diseases;
- the presence of farsightedness or myopia;
- development of malignant tumors.
What is retinoschisis
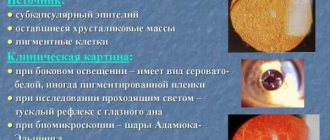
Retinoschisis (retinal detachment) is a pathological degenerative disease of the retina in which the membrane is separated due to the accumulation of fluid between the layers. Characteristic:
- cystic degeneration;
- folding of the retina;
- gap;
- detachment;
- pathological disorders in the structure of the vitreous body.
The mechanism of retinoschisis in the retina is due to the formation of cysts due to impaired blood flow. Small cysts merge with each other to form large cavities that divide the retina into layers.
Classification
Retinoschisis in medicine is usually divided into the following stages:
- The first stage - limited detachment of several layers of the retina occurs. The resulting fluid accumulates around the altered vessels.
- The second stage is the gradual development of delamination. However, there is no particular difference between the affected and healthy retina. Small cystic degenerations appear;
- The third stage - large cystic formations begin to appear between the layers of the retina. Stripes also form, which subsequently provoke retinal ruptures and contribute to complete retinal detachment. In this case, such a lesion is formed over a fairly large area.
Symptoms
Degenerative retinoschisis is characterized by an asymptomatic course. The disorder is most often diagnosed accidentally during the next visit to a specialist, since damage to the outer plexiform layer occurs. Also, most of the area is covered with small cystic changes in the layers.
In the hereditary form of retinoschisis, the first diagnosis occurs between the ages of 7 and 9 years. The pathology primarily affects the macular area, causing visual acuity to decrease. Large oval cystic formations begin to form, causing detachment. Secondary retinoschisis manifests itself as a complication of various eye problems.
The symptoms of retinossis completely depend on the type of underlying disease.
Causes of the disease
In ophthalmological practice, various classifications of retinoschisis are used, incl. built on cause-and-effect criteria. So, in one of them, all options and varieties are divided, in fact, into two large categories: senile/degenerative retinoschisis (age-related, dystrophic), and hereditary retinoschisis (congenital, X-linked). Other sources also consider tractional (“extension”, “avulsion”) and exudative (fluid, effusion) retinoschisis as separate forms.
Age-related retinoschisis is considered the most common form and is found, to varying degrees, in approximately 7% of people over 40 years of age. The etiology and trigger mechanisms are not entirely clear today, but it has been established that they are based on degenerative processes - disorders of blood circulation and nutrition of the retina, which often occur in its peripheral zones and can then spread to the central macular area. A statistical relationship was revealed between senile retinoschisis and vascular pathology, the presence of cystic retinal tumors, and diabetes mellitus (diabetic retinopathy).
The incidence of hereditary retinoschisis is much lower: different sources indicate the probability from 0.004% to 0.02%. There are several variants of inheritance, but the most commonly described is an aberration of the X chromosome (hence the name “X-linked retinoschisis”): males who inherit the pathology through the female line are affected. As a rule, this form of retinoschisis manifests itself and is diagnosed in early school or even preschool age.
In addition, common causes and risk factors for the development of retinoschisis include congenital, idiopathic anomalies of the visual system (for example, Coats disease or optic disc fossa), infectious and inflammatory processes of the eye, and some oncological diseases.
Diagnostics
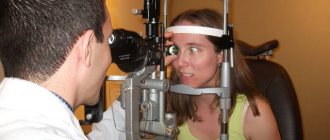
Diagnostic methods for retinoschisis are determined by a specialist. First of all, a test is performed to determine visual acuity, after which the border of peripheral vision is diagnosed and ophthalmoscopy is performed. Additionally, there may be a need for an electrophysiological study, which will determine how well the retina is performing its functions. Optical coherence tomography helps determine how badly the retinal structure is damaged.
In cases of genetic origin of pathology, it may be necessary to study heredity. To do this, molecular genetic tests can be performed to identify predisposition to the disease. All this contributes to the differential diagnosis of the existing disorder.
Retinoschisis
Manifestations of X-linked congenital retinoschisis are usually detected by 10 years of age, although there are early cases of the disease before the age of 3 months. Signs of the disease are found in both eyes and, as a rule, symmetrically. In the natural course of the disease, that is, without adequate medical care, as a rule, vision decreases already in the elementary grades of school, and vision decreases gradually over decades and can lead to complete blindness.
Senile retinoschisis
Senile retinoschisis is a disease that most often occurs over the age of 40 years. Its causes are peripheral dystrophic changes - accumulations of fluid in the retina, that is, cysts. They most likely occur when local circulation is impaired, like most other peripheral dystrophies, which is why senile retinoschisis occurs more often in the older age group.
Manifestations of retinoschisis
Since retinal dissection occurs, not only its structure is disrupted, but also its functions. First of all, this applies to the peripheral areas of the retina, where retinoschisis often begins, due to which areas of peripheral vision are lost, in accordance with the location and prevalence of retinoschisis. With significant damage to the retina, patients begin to navigate worse in poor lighting.
If retinoschisis continues to spread to the central region of the retina, which provides good quality vision, there is a risk of damage to it with irreversible loss of vision, as with retinal detachment.
In some cases, with X-linked congenital retinoschisis, retinal separation initially occurs in the central region of the retina, and in this case, decreased vision will be the first manifestation of the disease.
Retinoschisis can lead to some complications; most often, when a retinal tear occurs, retinal detachment occurs, and hemorrhages into the eye cavity, that is, hemophthalmos, are also less common.
Diagnostics
A thorough ophthalmological examination is carried out, and first of all, visual acuity, the boundaries of peripheral vision are checked and an examination of the fundus is carried out with the obligatory dilation of the pupils.
Also, to clarify the diagnosis, an electrophysiological study is performed to determine the function of the retina, as well as optical coherence tomography to clarify the nature of the damage to the retinal structure.
A distinctive feature of X-linked congenital retinoschisis is that the genetic material located on the X sex chromosome that causes the disease is inherited. Therefore, the child’s heredity is thoroughly studied, and there are now special molecular genetic tests that make it possible to establish a genetic predisposition to the disease or confirm the diagnosis.
Treatment of retinoschisis
When making a diagnosis of retinoschisis, careful monitoring of the condition of the fundus of the eye is necessary, that is, observation by an ophthalmologist.
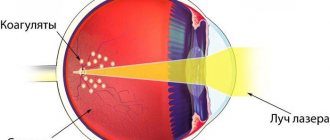
Retinoschisis can remain stable for quite a long time without spreading further along the fundus. However, in case of a threat to visual acuity and the spread of retinoschisis to the central region is detected, preventive laser coagulation of the retina is indicated. The barrier created using a laser serves as a barrier to further spread of retinal dissection into the central region and maintain good vision.
In the case of retinal dissection in the central zone with the spread of retinoschisis from the peripheral parts, initial dissection of the central region, or the appearance of complications, primarily retinal detachment, there is a need for surgical treatment. An operation is performed - either filling the retina by suturing a silicone seal to the outside of the eyeball, mainly when a retinal rupture and detachment occurs, or, most often, vitreoretinal surgery with the removal of the vitreous body from the eye cavity and straightening the retina from the inside. In addition, in this case, laser photocoagulation of the retina is also performed to further strengthen it.
Treatment
Retinoschisis can be treated with medications and surgery. With conservative treatment, as a rule, drugs are prescribed that accelerate blood flow and metabolic processes, preventing the retina from delaminating. For this we use:
- B vitamins – Milgamma, Riboflavin, Thiamine chloride;
- vitamin E – Aevit, Alpha-Tocopherol acetate;
- drugs with antiplatelet action - Pentoxifylline, Trental;
- angioprotectors – Nicergoline, Thiotriazoline.
Laser correction can be used to stop existing retinal dissection. Using laser coagulation, adhesions are made between the layers of the retina. A laser beam is used to solder the healthy part of the retina to the damaged areas around the circumference.
In the final stages of pathology, when there are ruptures and detachments, surgery is used. This treatment includes 2 types of operations:
- removal of the vitreous;
- scleral filling.
In some cases, after surgery, there may be a need for additional laser correction to enhance the result obtained.
Complications
In the absence of timely treatment, the disease develops into severe forms that lead to complete blindness. It is difficult to choose the right therapy for the congenital form of the disease, since it provokes hemorrhages in the retina. When the disease provokes retinal dissection, not only violations of its integrity arise, but also problems with the normal performance of its functions.
With severe damage to the retina, signs of complications such as loss of orientation in space with insufficiently strong lighting may occur. The quality of vision is significantly reduced, as a result of which a person can become completely blind. Retinoschisis can also provoke complications, such as:
- retinal tears;
- retinal detachment;
- development of hemorrhage in the eyeball.
Types and types of disease
Experts usually distinguish two types of retinoschisis:
- X-linked congenital.
- Degenerative, senile.
X-linked congenital retinoschisis is a genetically determined hereditary disease that results in retinal separation. Its cause is called a certain gene that is connected to the X chromosome, so the disease occurs exclusively in boys. This type of retinoschisis cannot develop in girls, but they are carriers of the disease gene and pass it on to their children. X-linked retinoschisis is a rather rare congenital pathology that is detected in one in 15 thousand people.
Symptoms of congenital retinoschisis, as a rule, appear by the age of ten, although in practice there are also earlier cases (in infancy). Manifestations of the disease are detected symmetrically in both eyes. Without adequate therapy, the natural course of the disease leads to serious visual impairment by school age. Further progression of retinoschisis over decades gradually leads to absolute blindness.
Senile retinoschisis is an age-related pathology that most often affects people of mature age (after 40 years). It is caused by peripheral degenerative changes in the retina, accompanied by the accumulation of fluid in its layers - retinal cysts. Presumably, the occurrence of cysts is caused by a violation of local circulation, by analogy with most other peripheral dystrophies. Therefore, older and elderly people are more often susceptible to the disease.
Forecast
Depending on the different forms of retinoschisis, the prognosis for the development of the disease may differ:
- with a hereditary form - a high risk of vision loss;
- in the degenerative form there is a low risk of cure;
- in the secondary form, the result directly depends on the course of the underlying disease - the root cause.
In order not to cause the risk of complications after surgery for retinoschisis, you should limit sports and other strength activities, and lifting heavy objects is prohibited. The specialist prepares a dietary plan that should be followed.
For a positive prognosis, it is necessary to follow all the specialist’s recommendations during the rehabilitation period and continue treatment until visual functions are completely restored.
Prevention
For the purpose of prevention, the following recommendations must be followed:
- Avoid eye strain. Provide mandatory rest for the visual organs.
- Protect eyes from harmful effects.
- Perform gymnastic exercises for the eyes.
- Increase the amount of vegetables and fruits, vitamins and microelements consumed.
- Include drugs and foods containing vitamins A, E and B in your diet. Also increase the amount of zinc in the body.
In any case, you should follow all the recommendations of a specialist to prevent deterioration in the quality of vision. You can save your vision by identifying the pathology in time and starting to treat it.