Symptoms of testicular torsion
In infants, signs of pathology increase gradually, over several hours: anxiety appears, monotonous crying, and body temperature rises. In some cases, regurgitation and even vomiting are observed.
In children over 2–3 years of age, the symptoms of the disease are more pronounced; the problem can be suspected based on the following signs:
- intense groin pain, often radiating to the lower abdomen;
- pale skin;
- the appearance of cold sweat;
- severe nausea;
- bouts of vomiting;
- general weakness;
- fever;
- change in the appearance of the scrotum: swelling, cyanosis.
In the absence of timely treatment for testicular torsion, the child has a high risk of developing tissue necrosis, which will entail removal of the damaged organ and possible infertility in the future.
Symptoms of the disease
The clinical picture depends on age. Symptoms of testicular torsion in adults include sudden pain in the scrotal area radiating to the corresponding groin area and lower abdomen.
Due to possible irritation of the solar plexus, some patients (especially young children) experience dyspeptic disorders: nausea and vomiting.
Noteworthy is the change in the location of the affected testicle; it is located higher than usual. Locally, there may be hyperemia (redness) of the skin of the scrotum.
On palpation, the gonad is compacted, painful, and increased in size due to increasing swelling.
If proper measures are not taken in the early period (up to 6 hours), local symptoms (swelling, redness of the scrotum, testicular enlargement) will increase, and the temperature may rise to 38 C.
In newborns with this pathology, palpation of the scrotum is painless (testicular torsion without pain), its size is increased, the color of the skin of the scrotum is variable: from severe hyperemia (redness) to a pale, bluish tint. Some boys are diagnosed with hydrocele.
Infants have increased excitability, tearfulness, breast refusal, and visual changes in the scrotum.
In childhood and adolescence, when testicular torsion occurs in boys, acute pain is noted in the scrotum area, lower abdomen; upon palpation, a heavy formation is felt in the groin or in the upper third of the scrotum.
Diagnostics
The diagnostic algorithm for surgical pathologies includes:
- collection of complaints and medical history;
- visual inspection;
- lab tests;
- Ultrasound.
If testicular torsion is suspected, the doctor carefully examines the scrotum, assesses the condition, size and color of the tissue, and determines anomalies of the anatomical position. During a visual examination, the doctor can record:
- change in the height of the testicle;
- limited mobility of the organ;
- redness and swelling of the scrotum;
- displacement of the testicle to the side;
- compacted tissue consistency.
Sometimes the symptoms of the disease are similar to signs of inflammation. To accurately determine the pathology, an ultrasound examination of the scrotum is performed. Additionally, Doppler ultrasound is performed - scanning of blood vessels, which helps to assess the blood supply to damaged tissues. In some cases, a diagnostic puncture followed by analysis of the liquid contents may be necessary.
Diagnostic measures
Differential diagnosis is made between acute inflammation of the testicle (orchitis), epididymis (epididymitis), strangulated inguinal hernia, hydrocele, allergic edema of the scrotum.
In order to determine testicular torsion, surgeons use the following technique: the patient is asked to stand up and the scrotum is lifted slightly upward. With inflammation, the pain syndrome decreases, but with volvulus, it remains unchanged. Additionally, the cremastor reflex is checked: with pronounced rotation, it is weakened or absent.
Clinical blood and urine tests may show no pathological changes.
A significant method in diagnosing testicular torsion is to perform an ultrasound examination with Doppler sonography, which allows one to assess the degree of blood flow disturbance, which will be a sign of existing testicular torsion.
Sometimes testicular scintigraphy is used to diagnose torsion, but this technique has not found widespread use due to low availability.
In emergency and unclear situations, diagnostic surgery can be performed: the skin of the scrotum, the lower part of the inguinal canal is cut, and an inspection is performed.
How is testicular torsion treated?
In most cases, the only treatment for this disease in children is surgery. It needs to be carried out as quickly as possible: already 6 hours after the first symptoms, the chance of preserving a full-fledged, healthy organ is reduced to 50%. 24 hours after the onset of the disease, in almost 100% of cases the testicle completely dies and must be removed.
Preparing for surgery
Before surgical treatment of testicular torsion, preoperative preparation is carried out:
- general blood and urine tests;
- clotting test;
- ECG;
- blood chemistry;
- consultation with a cardiologist, anesthesiologist and pediatrician.
How is the operation performed?
The intervention is performed under general anesthesia. The choice of access to the damaged area depends on the type of volvulus and the age of the child.
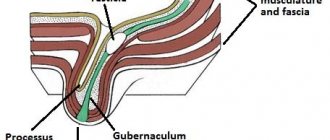
- In newborns and babies up to one year old, extravaginal torsion most often occurs, when the testicle twists outside the outer membrane. In this case, surgeons use the inguinal approach.
- Children over 1 year of age mainly encounter the intravaginal type of pathology, when volvulus occurs inside the membrane covering the testicle. In this situation, access through the scrotum is optimal.
During the work, the surgeon removes hydatides (formations on the epididymis) and fixes the damaged testicle using the surrounding tissue, so there is no risk of re-torsion in the child after surgery.
Additionally, a novocaine blockade is performed, which is necessary to eliminate pain and relieve inflammation.
How long surgery for testicular torsion lasts depends on the timeliness of seeking help. With prolonged tissue pinching, it takes 15 to 30 minutes to restore blood flow. At this time, during the intervention, warm compresses are applied to the damaged area to speed up blood supply. If 30 minutes after the start of thermal applications the testicle does not change color and remains lifeless, the issue of removing the organ is decided.
Possible complications
If the operation is performed in a timely manner, negative consequences of testicular torsion in boys are rare: the functions are completely preserved, and the tissues undergo minor changes.
Untimely treatment causes serious and irreversible pathological processes:
- deficiency of oxygen and nutrients in tissues;
- cessation of blood supply to the testicle;
- rapid necrosis;
- general intoxication of the body;
- infertility.
The amount of male hormone production will decrease significantly in the future, and if a healthy testicle cannot cope, there is a high probability of developing infertility.
What happens when testicular torsion occurs and what it can lead to?
Regardless of the form of testicular torsion, the consequences are negative: the blood supply to the male reproductive gland suffers, which ultimately causes testicular necrosis.
The severity of the changes that occur will depend on a number of factors:
• ischemia time, • severity of torsion, • spermatic cord length.
The longer the ischemia lasts due to impaired blood supply, the greater the likelihood of developing irreversible changes in tissues. After repeated torsion, the testicle is subject to atrophy processes (reduction in size with decrease (loss) of functional ability).
To complications
torsion includes the following pathological conditions:
• Necrosis. • Gangrene. • Scrotal abscess, Fournier's gangrene, • Chronic epididymitis. • Sepsis.
Rehabilitation after treatment
Children, as a rule, spend no more than 2 days in a hospital setting. After discharge, the child must:
- dynamic observation by a urologist with ultrasound control;
- limit physical activity and strength training for 2 months;
- take medications prescribed by your doctor to prevent infection;
- exclude cycling, horses and other activities that can injure the scrotum for 2-3 months.
The sutures are removed a week after discharge, and a month later it will be necessary to undergo a follow-up examination using ultrasound and general clinical tests.
Testicular hydatid torsion: what is it?
Torsion of testicular hydatid with suspension (otherwise known as hydatid of Morgagni) has a similar clinical picture, complaints and management tactics. Hydatids of Morgagni are rudimentary processes of the testicle and its appendage, derivatives of the paramesonephric duct. Hydatid volvulus manifests itself as a more erased (mild) clinical picture and has fewer complications. Pathology is most often diagnosed at the time of surgery. Intraoperatively, the rudiments are bandaged and cut off.
Testicular infarction
The choice of treatment methods is influenced by the pathogenetic factor, the possibility of restoring blood flow, and the patient’s age. The degree of destructive changes correlates with the duration of obstruction of the vessels of the spermatic cord. With ischemia lasting less than 6 hours, the probability of a successful outcome remains 90-100%. After 12-24 hours, tissue death is recorded in 20-50%. After 24 hours, the probability of saving the testicle is 0-10%; orchiectomy is required. In case of a total infarction, the gonad is completely removed; in case of a segmental process, local excision of the altered tissue is possible.
Conservative therapy
In case of extensive testicular infarction, it is not applicable. Management tactics for segmented necrosis remain controversial, but confidence in local damage confirmed by duplex scanning and MRI data leaves the possibility of prescribing medications to improve blood circulation, antispasmodics, and blood thinners. A prerequisite is monitoring the state over time. If therapy is unsuccessful or the lesion enlarges, surgical intervention is resorted to.
Surgical treatment
Urologists consider the condition as urgent, operations are performed on an emergency basis. In the localized form, the goal of intervention is to preserve healthy testicular tissue. Partial orchiectomy is considered the optimal choice for young patients. However, most cases of segmental testicular infarction end in organ removal surgery due to the inability to exclude malignant lesions.
After exposing the testis, the doctor evaluates the color of the gland tissue; in large centers, intraoperative histological examination can be performed to differentiate between a tumor and a focal infarction. During volvulus, untwisting is performed, and after blood flow is restored, the testicle is fixed to the scrotum (orchiopexy). Idiopathic infarction implies total orchiectomy due to the likelihood of developing a purulent-necrotic process, atrophy with malignancy. In the long term, plastic surgery is possible to restore the normal anatomical dimensions of the scrotum.
Testicular infarction. Macroperparameter. (photo by D.S. Davydov)
In the postoperative period, antibiotics, means to improve blood supply, and vitamins are prescribed. To prevent hydrocele, it is recommended to wear a jockstrap and avoid lifting heavy objects. Sexual life can be resumed after 4-6 weeks. Suffered ischemia negatively affects spermatogenesis; even with a favorable course for 36-40 weeks, the full production of sperm and testosterone by the affected gonad remains impaired.