Currently, circumcision has become one of the most popular male operations.
According to statistics, circumcision surgery is performed on every sixth man in the world. In Jewish and Muslim cultures, the ritual of circumcision is religious in nature.
In the United States, circumcision is considered a common medical procedure. American men use circumcision to solve both hygienic and aesthetic problems. Circumcision of a child's foreskin is performed right in the maternity hospital. Circumcision is most often performed on a child in the first 48 hours or 10 days after birth.
Proponents of circumcision believe that this procedure, despite some difficulty in performing it, brings enormous benefits to the male body. Thus, after circumcision, a child has a 10 times lower risk of getting a urinary tract infection. In addition, thanks to circumcision, a man gets the opportunity to prolong sexual intercourse.
Unlike male circumcision, female circumcision is considered an extremely harmful operation. This procedure is most common in Africa and the Middle East. The UN and Doctors Without Borders are against this manipulation that is detrimental to women’s health.
1
Circumcision of the foreskin
2 Circumcision of the foreskin
3 Circumcision of the foreskin
Circumcision in men. Indications
Male circumcision is performed in the following cases:
- medical indications;
- hygienic;
- religious.
In some conditions, circumcision is mandatory. Thus, with phimosis (sharp pathological narrowing of the foreskin), inflammatory purulent diseases can develop. One of the complications of phimosis is paraphimosis, in which the head or part of the head of the penis is pinched by a ring of the foreskin, and if circumcision is not done in time, this can lead to necrosis of the head and its amputation. Circumcision is also performed for foreskin cancer, post-burn or post-traumatic scar conditions.
Medical indications for circumcision
The most common indications for medical circumcision are the following diseases of the foreskin:
- phimosis (narrowing of the foreskin);
- paraphimosis;
- chronic recurrent, adhesive balanoposthitis (inflammation of the glans penis);
- lichen sclerosus;
- premature ejaculation, hypersensitivity (to increase the duration of sexual intercourse).
Hygienic indications for circumcision
In the pocket between the foreskin and the head of the penis, smegma accumulates, which serves as fertile ground for the development of infection. Stagnant smegma is also dangerous for women - contact with the cervix during sexual intercourse increases the risk of developing cervical cancer.
To prevent this, a man needs regular (at least twice a day) genital hygiene - it is necessary to retract the foreskin and wash off the smegma. Not everyone does this. Circumcision eliminates the need for such meticulous grooming in men.
Circumcision for religious reasons
Religious circumcision is performed at the request of the patient. Male circumcision as a religious ritual symbolizing unity with God was practiced in ancient Egypt. Currently, circumcision is most common among Jews and Muslims.
The Old Testament says: “This is My covenant, which you shall keep between Me, and you, and your descendants after you: that all your males shall be circumcised; circumcise your foreskin: and this will be a sign of the covenant between Me and you. Every male child among you throughout your generations shall be circumcised eight days from birth, and My covenant shall be an everlasting covenant upon your body. But the uncircumcised male who does not circumcise his foreskin [on the eighth day], that soul shall be cut off from among his people, for he has broken My covenant. (Joshua 5:2-8).”
The Holy Quran does not mention circumcision, but there are many hadiths (traditions) about its necessity. It is reported that someone came to the Prophet Mohammed and said: “I have accepted Islam.” Then the Prophet Mohammed commanded this man: “Throw off the hair of unbelief (that is, shave your head) and get circumcised” (collections of hadiths by Ahmad and Abu Daud).
Circumcision of the foreskin is performed to achieve the following purposes:
- reducing the risk of developing urinary tract infections, sexually transmitted diseases: genital herpes, syphilis, genital warts, HIV infection (AIDS);
- reducing the risk of developing (almost to zero) penile cancer;
- reducing the risk of cervical cancer in the wife of a circumcised man.
1 Consultation with a urologist
2 Consultation with a urologist
3 Consultation with a urologist
List of abbreviations
VPS - ventriculoperitoneal shunt
DTC - decompressive craniotomy
CT - computed tomography
MSCT - multislice computed tomography
SAH - subarachnoid hemorrhage
Dura mater - dura mater
Decompressive craniotomy (DTC) is used to relieve hypertensive-dislocation syndrome that occurs in severely ill patients during the acute period of subarachnoid hemorrhage [1, 2]. After stabilization of the neurological and somatic status, the patient undergoes cranioplasty surgery for protective, cosmetic and therapeutic purposes [3-7].
The most common operation in such patients is skull plastic surgery with autologous bone. Preservation of the patient’s bone before cranioplasty is carried out in two ways: cryopreservation and subcutaneous implantation in the anterior abdominal wall [8, 9]. Recently, there have been many reports on early and delayed complications of using autologous bone for cranioplasty [6, 10, 11]. The use of artificial implants can reduce the risk of postoperative complications compared to autologous bone. Previously, “freely” or “manually” modeled biopolymers were used. Currently, they are rarely used for plastic surgery of large defects due to poor cosmetic results. But the advent of stereolithographic and computer modeling technology for artificial implants has made it possible to improve the cosmetic results of such operations [12, 13].
The purpose of this study is to assess the risk of postoperative complications of cranioplasty, as well as to determine criteria for choosing a cranioplasty method.
Operation circumcision. How to prepare properly?
First of all, you should see a urologist for an initial consultation. Next, you will need to undergo a standard set of tests necessary for surgical treatment. The list of analyzes includes:
- general blood analysis;
- biochemical blood test (glucose, creatinine);
- coagulogram;
- infectious group (RW, HIV, Hepatitis B and C);
- ECG, consultation with a therapist (for men over 50 years old).
Circumcision of the foreskin
Posted at 14:36h in Services by doctor
Circumcision or circumcision is an operation that is performed for religious, medical, hygienic and even psychological reasons. It is usually performed on infants and young boys, but sometimes circumcision is performed on adult men.
Before you decide to have surgery, you should find out all the details about it, as well as take care of proper postoperative care.
From this article you will learn how circumcision is done correctly, under anesthesia or not; also photos of circumcision are presented here in sufficient quantities.
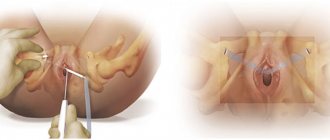
How is surgical treatment of foreskin diseases performed?
In our clinic, circumcision of the foreskin is performed on an outpatient basis, in the operating room, and the patient goes home within a few hours. The operation consists of excision of the foreskin and is performed under local anesthesia, however, at the request of the patient, the manipulation can be performed using sedation. Thus, during the operation the patient is in a state of medicated sleep and does not feel anything. The duration of the operation is 25-60 minutes. 1-2 days after circumcision surgery, the patient can return to daily activities with a number of restrictions. Absorbable sutures come off on their own; if the removal of the sutures is delayed, or they cause discomfort to the patient, the urologist removes the sutures on the 7-10th day. After 2 weeks, you are allowed to resume sexual activity.
Complications of circumcision (bleeding and infectious complications) are extremely rare.
When the tests are ready, you will come to the clinic to perform the operation. After the procedure, you will spend several hours under the supervision of a doctor in a comfortable single room in a day hospital. Then you can return home. If you are planning to have surgery with sedation, you should avoid eating in the morning. Also, keep in mind that driving is not advisable on this day, so plan to order a taxi or ask loved ones to pick you up after circumcision surgery.
How to optimally plan an operation? You only need to take 4 steps!
If you are planning to have circumcision surgery, then try to prepare for this event in advance.
Step 1 . Pass all the necessary tests (see above), you can take tests in our clinic any day from 08:00 to 11:00.
Step 2 . Call our call center and arrange a date and time for your initial consultation. If you wish, you will be connected directly to the doctor, and he will answer all your questions.
Step 3. Visit your doctor with your test results. During your appointment, the doctor will interview and examine you, answer in detail all your questions, analyze the test results and ask you to sign an informed consent for the operation. During the consultation, a date and time for the operation that is convenient for you will be determined. We recommend that you plan circumcision for the morning.
Step 4 . Come have an operation at MedicCity!
Material and methods
The retrospective study included 61 patients who, between 2010 and 2021, underwent preventive or delayed DST in the acute period of aneurysmal SAH after microsurgical exclusion of the aneurysm. All patients underwent cranioplasty after stabilization of their condition. Exclusion criteria from the study included childhood age, DST performed in another hospital, and bilateral DST. Gender, age, severity of the patient at the time of the first operation and at the time of cranioplasty, the presence of flap fragmentation during the primary operation, timing and material for cranioplasty, frequency of ventriculoperitoneal shunting, complications and interventions after cranioplasty, as well as follow-up period were assessed.
Sample characteristics
The sample included 61 patients (21 men and 26 women, mean age 45.2±9.4 years). All patients after DST underwent cranioplasty using autologous or artificial implants. Ventriculoperitoneal shunting complemented cranioplasty in 8 cases. Follow-up was possible in 36 (60%) patients over a period of 6 months to 7 years (average follow-up period 3.6±1.8 years). Patient data is presented in table. 1.
Table 1. Characteristics of the study group of patients
Method of preserving the patient's autologous bone
A fragment of skull bone removed during surgery is cleaned of blood, soft tissue and bone chips under sterile conditions, wrapped in dry sterile surgical material and sent for storage in a freezer, where it is stored at a temperature of –10 to –30 °C. Before cranioplasty, the autoimplant is removed from the freezer, defrosted and sterilized. Sterilization of models is carried out using a gas method (based on ethylene oxide) [13]. At the National Medical Research Center of Neurosurgery named after. N.N. Burdenko's method of preserving autologous bone subcutaneously in the area of the anterior abdominal wall is not used.
Cranioplasty technique
The incision is made along the old scar. The aponeurotic skin flap is separated from the temporal muscle and dura mater using a predominantly blunt method; if necessary, a monopolar coagulator or blunt-tipped scissors can be used. The atrophied temporalis muscle is carefully separated from the dura mater to avoid damage to it that could lead to liquorrhea. If the dura mater is damaged during the isolation stage, it is sutured or the defect is repaired with a fragment of the periosteum. If there is a bulge in the area of the trepanation defect that does not allow placing the implant and fixing it, a bolus injection of a hyperosmolar solution (20% mannitol, 200 ml), as well as short hyperventilation or temporary ventriculostomy of the anterior horn of the lateral ventricle can be used. If autologous bone is used as an implant, it is placed on the defect area and fixed with knot ligatures or craniofixes. In the case of using a pre-prepared sterile implant or molds for intraoperative modeling, holes are placed to suture the temporalis muscle. The temporalis muscle is fixed to the implant. Soft tissues are sutured in layers. An important point is the implementation of high-quality hemostasis before suturing soft tissues in order to prevent hemorrhagic complications. After suturing the soft tissues, a pressure aseptic bandage is applied. Skin sutures are removed no earlier than 8 days after surgery.
Circumcision. Postoperative period
Since circumcision of the foreskin is an operation, after it there will be pain at the site of the intervention for some time. Therefore, within three days after circumcision of the foreskin, the patient may be prescribed painkillers.
Circumcision in Moscow is carried out in many medical institutions. On the Internet you can find reviews about laser circumcision and other techniques. Whether circumcision with a laser (laser circumcision) or with the help of Surgitron is right for you, the doctor decides, paying attention to the complexity of the operation and concomitant diseases.
At the multidisciplinary clinic "MedicCity", consultations are conducted by highly qualified urologists who are ready to assist you in resolving any of the most delicate issues related to men's health.
The cost of circumcision surgery in our clinic is average in the capital. You can see the cost of circumcision surgery here. We are waiting for you at MedicCity!
results
Autologous bone grafting was performed on 47 patients (21 men and 26 women, average age 46.2±9.4 years). In 12 cases, the implant consisted of several fragments. In 6 cases, cranioplasty surgery was combined with simultaneous implantation of HPS ( n
=4) or delayed (
n
=2). Late and early complications were noted in 16 (34%) patients. In 2 patients, the occurrence of epileptic seizures was noted in the delayed period (after 2 and 6 months, respectively). Seizures can be controlled with anticonvulsants. When collecting a follow-up, it turned out that 2 (4.2%) patients died from causes unrelated to the interventions performed several years after discharge.
Artificial implants were installed in 14 patients. Complications were noted in 4 (28.5%) of them. This is mainly a delayed manifestation of the epileptic syndrome - in 3 (21.4%) patients (which can be controlled with anticonvulsants). It is worth noting that these patients did not have seizures before cranioplasty and did not receive anticonvulsant therapy. In 1 patient, after cranioplasty, a frontal sinus defect developed with the development of pneumocephalus, which required repeated surgical intervention to repair the defect. There were no fatal cases.
Data on complications of cranioplasty are presented in table. 2.
Table 2. Complication rates after cranioplasty
Repeated operations after cranioplasty
Repeated surgery was required in 11 patients, most of whom were patients ( n
=10) with autobone. Due to infectious complications (flap osteomyelitis), surgery was required in 6 (12.7%) patients. The average period of manifestation of infectious complications was 3.7 months (from 2 weeks to 6 months). In all cases, the wound was sanitation and the osteomyelitic implant was removed. Subsequently, 4 patients underwent plastic surgery with an artificial implant after 4-6 months. In 2 patients, repeat cranioplasty was not performed due to contraindications to surgery. Bone lysis was noted in 7 (14.8%) cases (Fig. 1).
Rice.
Fig. 1. Plastic surgery of a skull defect with a stereolithographic implant based on bone cement (Palacos): a, b – view before plastic surgery; c, d – view after plastic surgery. It is noteworthy that 5 (71%) patients underwent cranioplasty with a fragmented bone flap. In 2 cases, repeated operations were performed for cosmetic and protective purposes: resection of partially lysed bones and cranioplasty with an artificial implant. In 2 (2.1%) cases, after cranioplasty (in one of them after implantation of an artificial implant), pneumocephalus occurred associated with a defect in the frontal sinus on the side of the intervention (Fig. 2).
Rice. 2. Autolysis of the bone implant 11 months after cranioplasty. a — data from 3D reconstruction of MSCT examination; b – intraoperative view of bone implant resorption; c – demonstration of the lysed flap on a 3D model of the patient’s skull. The plastic surgery was performed under general anesthesia through a trans-eyebrow approach to the lateral parts of the frontal sinus, with the defect being plugged with a fragment of periosteum, Tachocomb material and fibrin-thrombin glue. After the interventions, no recurrence of pneumocephalus was observed.
Risk factors for complications
When analyzing the material, it was found that risk factors for infectious complications were the patient's age over 60 years and the presence of a fragmented flap (5 out of 7 patients had a fragmented flap). Unfortunately, given the small sample of patients, it is impossible to statistically confirm this conclusion.
It was not possible in this study to identify factors associated with the manifestation of epileptic syndrome or hydrocephalus in the postoperative period.
Skull plastic surgery is not so much cosmetic as therapeutic - cranioplasty improves the neurological status in the postoperative period, which has been demonstrated in many studies [3, 5, 6, 14, 15]. Despite the fact that the operation is technically quite simple, there is a risk of complications, which, according to the literature [16–18], can reach 18–36.5%. Aseptic bone graft resorption occurs in 24–50% of patients. Older age, flap fragmentation, hydrocephalus, and HPS dependence have been noted to be possible risk factors for bone resorption, although the exact causes have not yet been established [6, 11, 15, 19–21].
Perhaps one of the factors influencing the lysis of an autologous flap is the method of its storage and/or sterilization. Thus, in one of the studies it was demonstrated that flaps with subcutaneous preservation in the area of the anterior abdominal wall are less subject to autolysis after cranioplasty [22]. In our opinion, this technique is not justified due to increased trauma (double invasion of the anterior abdominal wall). It has also been shown that subcutaneous flaps can lyse over time under the influence of macrophages [9].
Currently, there are many artificial biopolymer or titanium computer-simulated implants (Fig. 3),
Rice. 3. Pneumocephalus after cranioplasty, the arrow indicates a defect in the left frontal sinus. which have been shown to achieve good cosmetic results with a low risk of complications [12, 22, 23]. At the same time, some implants or preoperative computer modeling can be quite expensive, and in rare cases there is a risk of a foreign body reaction to the allograft [13].
An underestimated complication, in our opinion, is the manifestation of epileptic syndrome in the delayed period after cranioplasty. According to the literature [18, 23], the risk of this complication reaches 14.8%; its connection with one or another type of implant has not been proven. In our work, such a complication was identified in 5 (8.1%) patients. In all cases, the epileptic syndrome was moderate in nature with a frequency of attacks from 1 to 6 per year. No seizures were observed while taking anticonvulsant therapy.
Surgical tactics for cerebrospinal fluid dynamics disorders (hygromas, ventriculomegaly, hydrocephalus) in patients who have undergone DST remain a controversial issue. There is no consensus regarding the timing and order of shunting operations and cranioplasty. According to the results of the work of Juneyoung et al., which included 51 patients, in 32 (62.7%) cases bypass surgery and cranioplasty were performed simultaneously. The risk of postoperative complications was 43%. Thus, the authors do not recommend performing bypass surgery simultaneously with cranioplasty. Recently, we also believe that it is better to separate these operations. Most patients after DST may experience liquorodynamic disturbances in the form of hygromas, ventriculomegaly, which do not cause neurological disorders. As proposed in 1970 by Davson et al. According to the theory of cerebrospinal fluid (CSF) absorption, the latter is absorbed into the superior sagittal sinus (SSS) in the presence of a pressure gradient between them. For normal absorption of CSF, a gradient of 3-5 mmHg is required. If the integrity of the skull is violated (after DST) in the long-term period, ICP becomes equal to atmospheric pressure, which can lead to a decrease in the gradient (ICP/VSS), thereby causing CSF hyporesorption, which manifests itself in the form of liquorodynamic disorders. Studies show that these disorders can regress against the background of restoring the integrity of the skull (cranioplasty). In our study, in only 3 cases cranioplasty was combined with simultaneous implantation of a VPS; in 2 patients, a VPS was installed before cranioplasty, in 2 patients - after. We were unable to determine the relationship between the timing of HPS implantation and postoperative complications. To avoid unjustified interventions, we recommend that the first step be plastic surgery of the skull defect, followed by determining the indications for shunt surgery. This issue requires detailed analysis on a larger sample of patients and is not the main purpose of our study.
Infectious and cosmetic complications served as a reason to review the indications for DST and limit their unjustified implementation. Also, in cases of fragmented flaps, we abandoned autoimplants during cranioplasty [10, 11, 19, 20].
We noted that when using an artificial implant there is a lower risk of postoperative complications. In no case did we note a reaction to foreign material or infectious complications. In this work, we were unable to confirm the effect of the timing of cranioplasty on the risk of postoperative complications, as the authors of other works do not show such an effect [23].
Based on our experience and the results presented in this work, we are of the opinion that in elderly patients or in patients whose bone fragments during DST, it is more appropriate to perform cranioplasty using simulated implants based on polymethyl methacrylate (Palacos) (Fig. 4) .
Rice. 4. Example of 3D computer modeling of a customized implant: a – front view; b – side view. In our opinion, cranioplasty is fraught with a significant risk of postoperative complications, reaching 18%. The tactics of widespread aggressive performance of DT without strict indications in the acute period of aneurysmal SAH can lead to complications of both DT and cranioplasty.
Surgical methods
Circumcision refers to plastic surgery. Modern surgery offers several intervention options; the choice depends on the joint decision of the patient and the doctor.
Partial. Often used for phimosis and paraphimosis. Only part of the foreskin is removed, allowing the glans to be exposed. At rest, it is half hidden by a fold of skin.- Free. Fully opens the head of the penis. A groove is formed in the coronal region of the genitals.
- Minimal. This circumcision process is used for cicatricial phimosis or excessive growth of the foreskin. Only excess hanging skin is removed; at rest, the head is completely closed.
- Tight. The entire foreskin is cut off, the head is completely open. This circumcision procedure is carried out only after detailed consultations with a urologist; contraindications are possible.
- High. It is used for significant growth of the foreskin. The circular postoperative suture can be located at different heights.
- Low. The incision to remove the skin fold is made in the coronary groove, which also hides the postoperative suture.
Circumcision surgery is irreversible, so before starting it, you need to weigh all the advantages and disadvantages. Complications are rare; in some cases, allergies to medications or scarring are possible.