Causes of stress incontinence in women
The cause of the pathology lies in the structure of the female urinary organs. In the weaker sex, a short urethra emerges from the bladder, which opens on the vulva.
Laughing, sneezing, physical activity and coughing increase intra-abdominal pressure, causing the bladder to move downward. In this case, the middle part of the urethra is normally held in place and even rises slightly upward with the help of ligaments. As a result, the urethra becomes bent, blocking the passage of urine.
A pathology called stress incontinence occurs due to weakening of the ligamentous apparatus that supports the urethra in the correct position. In this case, with an increase in intra-abdominal pressure, the urethra becomes hypermobile, i.e., it cannot stay in place and falls down after the bladder. As a result, the urinary tract cannot create a barrier to urine, and it begins to be released spontaneously.
In the ICD - International Classification of Diseases - stress incontinence caused by urethral hypermobility is coded N39.4, since it refers to specified types of urinary incontinence.
This type of urinary incontinence can be combined with other disorders of the urinary system. In this case, the woman requires complex treatment.
Constant leakage of urine causes physical and psychological discomfort. Patients feel complex because of the unpleasant odor, and inflammatory foci, ulcers and cracks form on the genital mucosa, caused by tissue irritation from leaking urine. You can correct the situation by contacting the Center for Aesthetic Medicine of St. Petersburg. Specialists will identify the cause of incontinence and treat it using modern methods.
Stress incontinence
Causes of stress incontinence:
- Age-related changes . With age, tissues become less elastic and lose tone. The same applies to the ligaments that support the urethra. As a result, a woman develops urethral hypermobility, leading to urinary incontinence.
- Hormonal imbalance . In this case, the ligaments weaken due to a lack of female hormones that maintain their tone. Treatment with drugs that compensate for hormonal deficiency will not change the situation, since the tissues have already changed properties. The problem can only be fixed through surgery.
- Difficult and numerous births , especially those accompanied by ruptures and the use of obstetric instruments.
- Intense exercise in strength sports , high degree of obesity, constipation, severe diseases of the lungs and bronchi, accompanied by cough. In such women, due to frequent increases in intra-abdominal pressure, sprains occur in the ligaments that support the urethra, which leads to incontinence.
- Dramatic weight loss . Rapid changes in weight lead to prolapse of organs (ptosis), weakening of ligaments and leakage of urine.
- Features of the structure of the pelvic organs and connective tissue. Sometimes urine is not retained due to the physiologically incorrect location of the bladder and urethra, as well as due to the structural features of the tissue that supports the pelvic organs.
The specialists of the Center for Aesthetic Medicine will relieve stress incontinence, regardless of its causes. Doctors will select the optimal method for eliminating mobility of the urethra, relieving the woman of complexes and health problems.
In what cases is it carried out?
The main indication for surgery—urethral transposition—is such a pathology in women as postcoital cystitis. Let us remember that this is an inflammation of the bladder caused by a fungal or bacterial infection. Cystitis, the symptoms of which appear 1-2 days after intimacy, is called postcoital. An exacerbation of the condition usually occurs after each sexual intercourse.
Transposition of the urethra is prescribed in cases where non-surgical treatment methods have been ineffective.
Moving the external opening of the urethra gives a positive result due to anatomical features:
- Near the outer part of the urethra is the wall of the vagina.
- Increased activity in this area of the urethra.
- Remnants of the hymen (urethro-hymenal folds) lead to displacement of the external opening of the urethra into the vagina during intimacy.
Due to the conditions described above, during sexual intercourse, the urethra moves into the vagina, the outer part opens. As a result, the vaginal microflora with existing bacteria penetrates the urethra and bladder.
Transposition of the urethra in women is not performed during pregnancy and in the period after childbirth, with vaginal candidiasis, with acute inflammation in the vagina/urethral area.
Indications for surgery to eliminate urethral hypermobility
Urine leakage during laughing, sneezing, coughing, or physical activity.
Combined types of incontinence, in which the mobility of the urethra is combined with other disorders. In addition to surgery, the woman is prescribed additional treatment.
High degree of obesity, severe illness, accompanied by constant coughing attacks. The operation is prescribed as a preventive measure at the first signs of incontinence.
Degrees of urinary incontinence
Contraindications
- Infectious processes in the pelvis and genital tract, including STDs. Surgical treatment is carried out only after the infection has been eliminated.
- Rashes in the intimate area caused by herpes, papillomavirus, skin diseases.
- Pregnancy, including those planned in the near future. Since it is unknown what the birth will be like, it is better for a woman to postpone surgical treatment until the birth of the child and the end of the postpartum period.
- Menstruation.
- Reduced blood clotting.
- Cancerous and precancerous pathologies.
- Exacerbation of chronic diseases.
- Poor health, fever, colds.
The operation is not performed for incontinence caused by significant prolapse of internal organs and dysfunction of the nervous system. In this case, the woman requires other treatment.
Preparation for the treatment of stress incontinence caused by urethral hypermobility
At the appointment, the doctor will find out the type of urinary incontinence. To associate incontinence with urethral hypermobility, the woman is asked to lie down on a couch and cough. This test is called a cough test - with stress incontinence, urine is released during coughing.
A woman is asked about situations in which urine leakage occurs. If incontinence occurs not only during wakefulness, but also during sleep, or is accompanied by other disorders of the urinary system, the patient may require other treatment or a combination of surgery with additional therapeutic methods.
Before the operation, the woman undergoes tests:
- General blood and urine tests.
- Blood for clotting time and bleeding duration.
- Blood for syphilis, AIDS and hepatitis.
- Smears from the genital tract for microflora and infections.
- Pap smear of the cervix for cancer and precancer.
If necessary, the following are prescribed:
- Cystoscopy is an examination of the bladder from the inside using a special device - a cystoscope.
- Ultrasound of the pelvis.
Other tests may be needed. Most often they are performed on women suffering from chronic pathologies.
A new approach to the treatment of postcoital cystitis
Target.
Evaluation of the effectiveness and safety of a combined minimally invasive technique for removal of urethrohymenal adhesions and para-urteral filler implantation.
Patients and methods.
38 patients with postcoital cystitis were treated.
Age ranged from 17 to 38 years. Of these, in 34 (89%) women the disease debuted with the onset of sexual activity, and in 4 (11%) with the onset of regular sexual activity. Upon examination, all patients showed varying degrees of severity of urethro-hymenal adhesions and a positive O᾽Donnell-Hirschhorn test. All women underwent cystoscopy before and after surgery. In one case, urethral transposition was previously performed with a temporary effect. All women underwent surgical treatment - removal of urethro-hymenal adhesions and suburethral injection of hyaluronic acid-based filler. The gel was injected paraurethrally, fan-shaped, in a volume of 1-2 ml, from a point at 6 o’clock on the dial, creating a gel cushion and thus lifting the meatus and distal urethra, limiting their mobility and contact damage during coitus. No complications were observed. Results.
Quality of life improved in 29 (76%) patients.
In 2 patients (5%) after 8 months, as the gel biodegraded, cystitis recurred, however, in 1 woman the symptoms were not so pronounced, which did not require repeated administration of the gel; in one observation, the filler was reinjected. In a patient who had previously undergone urethral transposition, injection of filler did not bring the desired effect. In another 6 patients (16%), postcoital urinary dysfunction ceased, however, relapses of cystitis persisted, which required fulguration of bladder leukoplakia. Patients under observation. After surgery, examinations were performed at 1, 6, and 12 months. During vaginal examination, when performing the Hirschhorn test, the external opening of the urethra did not shift inward, the urethra was projected above the entrance to the vagina. Of all women operated on using the described method, 76% of cases showed an improvement in sexual life. No patient required urethral transposition. Conclusions.
A minimally invasive technique can improve the results of treatment of patients with postcoital cystitis.
This technique is free of the risks of developing secondary dyspareunia and disruption of vaginal and clitoral orgasms, and can serve as an alternative to traditional urethral transposition. The main disadvantage is the natural biodegradation of the gel, which may require its repeated administration. Key words:
postcoital cystitis, urethral transposition, paraurethral filler implantation, filler.
For citation:
Glybochko P.V., Rapoport L.M., Inoyatov Zh.Sh., Enikeev M.E., Enikeev D.V., Snurnitsyna O.V., Malinina O.Yu., Lobanov M.V. , Demidko Yu.L. A new approach to the treatment of postcoital cystitis. Issues of urology and andrology. 2019; 7(1): 59–63. DOI: 10.20953/2307-6631-2019-1-59-63
How is surgery performed to eliminate urethral hypermobility and incontinence?
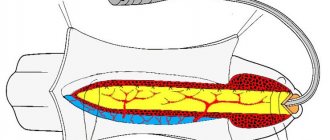
During the operation, the doctor places a special mesh tape under the urethra - a sling, which is then secured in the tissues of the groin or pubis. The mesh structure gradually fuses with the tissues, serving as a kind of frame. The sling supports the ligaments, relieving the urethra from hypermobility and maintaining the correct position of the urethra when intra-abdominal pressure increases.
Urosling
The intervention is performed under general anesthesia. It is possible to use epidural and spinal anesthesia, during which an anesthetic drug is injected into the spine, turning off the sensitivity of the lower half of the body.
After anesthesia, the doctor makes an incision on the upper wall of the vagina, through which the tissues of the urethra and female genital tract are separated.
Two more miniature incisions are made, which can be located:
- On the abdomen in the pubic area - this operation is called retropubic.
- In the groin - this method is called suburethral.
Then a mesh consisting of thin polymer threads is passed through the incisions. The sling can be inserted:
- From top to bottom - in this case, the doctor inserts a mesh tape into one of the upper incisions, passes it under the urethra and brings it out into the second upper incision.
- From bottom to top - the mesh is passed under the urethra, and then pulled up and removed through two incisions in the skin.
There are mini-slings - small meshes used to treat mild forms of incontinence. During this operation, the doctor makes one incision in the upper part of the vagina. The mini-sling passed through it is secured in the tissues using special fasteners resembling a plastic harpoon.
The method of mesh insertion is selected individually for each woman, depending on the characteristics of the disease and individual body structure.
The inserted tape (sling) is given the necessary tension, allowing it to support the urethra without pinching it. When this can be achieved, the doctor secures the ends of the tape in the tissue and cuts them. Soon the incisions will heal, and traces of the operation will become almost invisible.
After the sling is inserted, the woman remains in the clinic for some time and then can go home - she does not require hospitalization.
Sling surgery
How is the operation performed?
At the patient's choice or according to indications, general anesthesia or spinal anesthesia is performed first. The decision about surgery should be made by a woman together with a doctor, after a series of studies, which include:
- visual examination on a gynecological chair;
- general blood analysis;
- general urine analysis;
- a smear to check the purity of the vaginal microflora;
- urogenital smear for infections.
If the degree of cleanliness of the vagina is insufficient, and also if the presence of any infectious diseases has been detected, then the operation is postponed until the pathologies are completely cured.
Otherwise, the disease may spread to other organs, as a result of which the upper urinary tract and even the kidneys will become infected, which is much worse than postcoital cystitis. Contraindications include the period of menstruation, as well as 2 days before and after it.
When all the tests are collected and their indicators are normal, the anesthesiologist asks the woman if she is allergic to any drugs. Next, anesthesia is administered in the operating room, and the surgeon begins performing urethral transposition with vaginal access.
The manipulation itself is relatively short and falls into the category of simple ones. The likelihood of postoperative complications is extremely low, but it is still worth taking the choice of the attending physician with full responsibility.
What to do after surgery to correct urethral hypermobility and treat incontinence
- In the first days after installing the sling, a woman may experience pain, swelling, discomfort in the vaginal area, and discomfort when urinating. The symptoms will gradually go away if the woman follows the doctor’s recommendations.
- To avoid bleeding, inflammation and other complications, certain restrictions must be observed during the recovery period. A woman must not:
- Lift weights, play sports, go to the gym.
- Live sexually.
- Swim in a bathtub, pool or pond.
- Overheating - bathhouse, solarium, sauna, beach are prohibited.
- Use medications not recommended by your doctor. Self-medication can cause inflammation, allergies, infection, and bleeding.
You can return to your normal lifestyle only after a medical appointment, during which the urologist will make sure that tissue healing is completely complete.
Women suffering from urethral hypermobility, leading to stress incontinence, should contact the Center for Aesthetic Medicine in St. Petersburg. Doctors will perform research, select the best method of surgery and carry out treatment using advanced technologies.
Urethral transposition
The rarest form of bladder inflammation is postcoital cystitis. With postcoital cystitis, inflammation in the bladder occurs after sexual intercourse. This is facilitated by the anatomical features of the urethra, such as its low location or hypermobility (excessive mobility of the distal urethra). The consequence of this is that during sexual intercourse the urethra moves into the vagina, and due to friction, flora pathogenic for the urinary system penetrates through the urethra into the bladder and causes inflammation.
The clinical picture of such inflammation is no different from the usual manifestations of cystitis. Unlike typical cystitis, which is most often caused by hypothermia, and which usually occurs infrequently, postcoital cystitis occurs after each sexual intercourse. This forces a woman to limit or avoid sexual intercourse. A misconception about the true causes of the disease may lead to thoughts that the husband has other sexual partners. There may be discord in the relationship between the spouses and a break in the relationship. At the same time, the examination, as a rule, does not detect sexually transmitted infections in spouses.
Treatment can be conservative or surgical. Conservative treatment involves taking antibacterial drugs to “get ahead” of the inflammatory process, i.e. taking a single dose of antibiotic before sexual intercourse. But this approach does not suit all women. Patients who have regular sexual intercourse, sometimes daily, are usually not satisfied with the constant use of antibacterial drugs. In this case, the only and very effective treatment method is surgical. It should be noted that this is the only form of bacterial cystitis that can be treated surgically.
Transposition of the urethra is not a very complicated operation in which the external opening of the urethra is moved upward by 1.5-2 cm from its original position. The operation is performed in a hospital setting, where the stay takes no more than 1-2 days. For a certain time after the operation, the patient is not recommended to have sexual activity, usually 4 weeks, during which complete healing of the postoperative wound occurs. The positive effect of this operation, performed with absolute indications and technically correct, is about 90%. Transposition of the distal urethra is an effective surgical treatment for hypermobility and vaginal ectopia of the urethra in women. This operation allows you to relieve the patient from constant infection and exacerbation of urinary tract infection