Snoring occurs due to attachment to past patterns
The psychosomatics of snoring in men and women is not much different. One of the basic psychological reasons is the reluctance to give up outdated attitudes, stereotypes and behavior patterns. A person is even ready to conflict with other people in order to preserve and defend old patterns of behavior.
It is important! The patient does not want to move forward, he wants to live as before. Moreover, he imposes his old model of life on everyone around him. This is why rhonchopathy is more common among older people.
Ronchopathy at a subtle level
Medicine explains rhonchopathy by narrowing of the upper respiratory tract. It disrupts air flow, resulting in wave vibrations. That's what we hear.
What affects the appearance of the disease:
- decreased muscle tone of the nasopharynx;
- respiratory diseases;
- specific structure of the jaw.
It is believed that only men snore. But in fact, rhonchopathy can occur in any person, regardless of gender and age. It's all about airway patency, not socio-demographic characteristics.
Female rhonchopathy
In women, snoring is associated with unexpressed thoughts, suppressed feelings, negative attitudes, and depression. They are tormented by grievances, irritation, and unpleasant memories. A special role is played by misunderstanding and a feeling of alienation in relationships with loved ones.
Ronchopathy in a woman is a protest, an expression of reluctance to change her habits and opinions. This is especially noticeable among mature women. Their children grow up, but mothers still try to impose their opinions. Confrontation between adult children and parents results in stress and snoring in women.
It is important! Snoring in women during pregnancy is associated with hormonal changes, weight gain, and swelling. Ronchopathy often occurs in women during pregnancy and menopause.
Night breathing problems in children
Children's snoring has the same reason - bitterness and despair. But what exactly causes such feelings, even the child himself does not always know. It can be assumed that the reason lies in the behavior of the parents. Most likely, the child lacks love, attention and support. Another reason is guilt. The child takes personal account of conflicts between parents and conflicts with peers.
Psychosomatic causes of snoring
In the works of ancient philosophers there are many statements about the influence of a person’s psychological status on the physical state of the body. Psychosomatics deals with the problem of studying the relationship between the development of pathological conditions and emotional state. As for snoring, psychotherapists identify several psychosomatic reasons for its occurrence during sleep. This:
- Blocking the emotional mood. The need to mask your true feelings is a prerequisite for the accumulation of negative energy, which is released during relaxation during sleep.
- Secretiveness of character. The inability or unwillingness to openly express one’s opinion, or concealing one’s point of view to please others, leads to the need to relax. This appears in heavy dreams and is accompanied by snoring.
- Problems with self-realization and self-esteem. Unfulfilled plans and dissatisfaction with oneself give rise to a depressed state that is disturbing in a dream.
Folk remedies for snoring
Deep despair from the awareness of one’s worthlessness, self-abasement, anger, and resentment spill out through night snoring, relieving a person of this heavy burden.
It should be noted that snoring in men is no more common than snoring in women, although there is an opinion that only men snore. Ronchopathy occurs even in children. Consequently, this pathological condition is inherent in all age categories and does not depend on gender.
Features of female rhonchopathy
Excessive emotionality, impulsiveness, sensitivity and the ability to empathize are the main causes of stress and depression in women. To these should be added a tendency to dramatize events, the accumulation of grievances due to lack of attention and misunderstanding on the part of family and friends.
The feeling of possessiveness towards children and husband, colliding with their desire for freedom and self-affirmation, often leads to disappointment and despair. As a protest, the body splashes out negative emotions with loud night snoring.
Psychosomatic factors of snoring are expressed by a reluctance to abandon existing stereotypical ideas about behavior patterns, giving rise to conflict situations and lack of mutual understanding. The desire to impose your ideas about everything on others results in stress and restless sleep, which provokes protesting snoring.
Psychosomatics of snoring
The snorer himself rarely suffers from his illness. But the people around the snorer suffer from sleep disturbances, insomnia, headaches, migraines, and constant fatigue. And even if a person lives alone, it is important to get rid of snoring. Because without correction, psychological problems can provoke the development of new diseases.
Damage to the nasal septum
A deviated nasal septum creates an obstruction to air movement. Wheezing is the result of sound vibrations.
Overweight and obesity
Fat is deposited everywhere, including on the outside of the neck and inside the throat. The more excess weight, the greater the load on the organs. Fat narrows the airway space.
In severe stages of obesity, not only snoring is observed, but also sleep apnea syndrome (stopping breathing). This is life-threatening and requires the use of a special device that maintains oxygen exchange and normal pressure levels in the nasal cavity and mouth.
Smoking
Smoking has a negative impact in several ways:
- dries out the mucous membrane, which causes nasal congestion;
- irritates the respiratory system, which leads to inflammation and narrowing of air space;
- stimulates the production of mucus (it fills the passages and disrupts air circulation).
In addition, smoking causes vasospasm, which impairs blood flow and weakens vascular and muscle tone.
Cervical osteochondrosis
Osteochondrosis disrupts blood circulation and oxygen exchange, salt deposits turn into growths, pinching muscles and blood vessels. Osteochondrosis is destructive changes in cartilage tissue. Without treatment, the disease will spread further and cause greater dysfunction of the musculoskeletal system.
Sleep positions
The worst position is lying on your back. The muscles of the nasopharynx relax too much, which causes snoring. In addition, it is important to pay attention to the position of the head. It should be higher than the body. To correct your sleeping position, you can purchase a special orthopedic mattress and pillow.
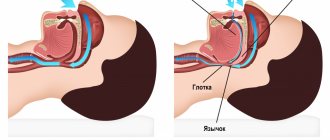
Mechanism of occurrence
Snoring occurs due to decreased tone of the muscles of the larynx and pharynx. What we take for snoring is vibrations of the walls of the pharynx, soft palate and root of the tongue. Snoring is the result of soft tissues closing during inspiration and blocking the airways. This disorder can occur for a number of anatomical, physiological and psychological reasons.
It is important! Changes that cause snoring can provoke the development of another problem - apnea. Apnea is interruption of breathing during sleep. It occurs due to the collapse of the walls of the nasopharynx.
Effect of the nasal septum
A reason that is relevant for all age groups. The nasal septum is a plate that divides the nasal cavity into two parts. A deviated septum impairs air circulation and causes rhinitis. It further worsens the patient's condition.
Nasal polyps and nasal congestion
Polyps are growths of the mucous tissue of the nasal cavity. The more growths, secretions, etc. in the nose, the less space is left for air movement. Remember how a person sniffles with a runny nose. At night, due to the special situation, the condition worsens even more.
It is important! Polyps make themselves felt only in the later stages. There is difficulty breathing, nasal congestion, and frequent upper respiratory tract infections.
Tonsils and adenoids
Inflammation in the throat also narrows the space for air movement. Enlargement of the tonsils is often observed, and it can be both anatomical and infectious. In both cases, this causes snoring. Changes in the tonsils are noticeable during wakefulness - the person breathes heavily and frequently, and opens his mouth slightly.
Adenoids occur against the background of infections and allergies. Lymphoid tissue grows and blocks the pharynx. You can suspect adenoids during wakefulness by noisy and difficult breathing, or hearing problems.
Congenital features
Congenital features include an elongated uvula or a large tongue. This anatomy blocks the lumen of the pharynx, which causes snoring. To combat congenital features, special mouthguards and palatal implants are used. The device is installed in an outpatient hospital setting.
Obstructive sleep apnea syndrome (OSAS) is
a condition characterized by the presence of snoring, periodic collapse of the upper airways at the level of the pharynx and cessation of pulmonary ventilation with continued respiratory efforts, decreased blood oxygen levels, severe sleep fragmentation and excessive daytime sleepiness.
A generally accepted criterion for the severity of OSA is the frequency of apnea and hypopnea per hour - the apnea/hypopnea index (AHI). It is considered inappropriate to separately calculate the number of apneas and hypopneas, since they carry similar risks in terms of developing cardiovascular and other complications. Currently, most international consensuses and clinical guidelines adhere to the classification shown in Table 1.
Classification of OSA severity based on the apnea/hypopnea index (AHI).
| Severity of OSA | YAG |
| Lightweight | from >5 to <15 |
| Moderate | from >15 to <30 |
| Heavy | >30 |
Epidemiology
The prevalence of OSA is 5-7% of the total population over 30 years of age. About 1-2% of this group of people suffer from severe forms of the disease [36,42,64,70]. In people over 60 years of age, the incidence of OSA increases significantly and is about 30% in men and about 20% in women. In people over 65 years of age, the incidence of the disease can reach 60% [6]. The prevalence of clinically significant sleep-disordered breathing reaches 15% in therapeutic patients in a hospital [27,34,37]. These figures exceed the prevalence of bronchial asthma.
Epidemiology and pathogenesis
During sleep, the overall muscle tone naturally decreases, in particular, the movable structures at the level of the pharynx relax. If there are predisposing factors that cause a narrowing of the pharynx, snoring may occur due to the beating of the soft palate against the walls of the respiratory tract. With further narrowing of the airways, their complete collapse and the development of an episode of apnea are possible. The patency of the upper respiratory tract depends on the size of its internal diameter, the tone of the pharyngeal muscles and the degree of pressure reduction in the trachea and bronchi during inhalation. Figure 2 shows the reasons for the development of pathological narrowing and collapse of the airways during sleep.
Reduction in initial airway diameter
- · Obesity.
- · Anatomical defects at the level of the nose and pharynx (deviated nasal septum, polyps, enlarged tonsils, elongated uvula, neoplasms).
- · Retrognathia and micrognathia (small and posteriorly displaced lower jaw).
- · Hypothyroidism (decreased thyroid function).
- · Acromegaly (pathological enlargement of certain parts of the body due to impaired production of growth hormone in adults).
Metabolic, hormonal and endocrine disorders
Practicing doctors know quite well such pathological conditions as metabolic syndrome and Pickwickian syndrome. In both cases, the main component of these syndromes is obesity. However, few people realize that in patients with metabolic syndrome, the prevalence of OSA is about 50%, and in patients with Pickwickian syndrome - 90%. Moreover, OSA plays a significant role in the progression of both pathological conditions. Increasing severity of OSA increases visceral obesity and metabolic syndrome by disrupting the production of night-time hormones such as cortisol and insulin. In severe cases of OSA, a disturbance in the production of somatotropic hormone (growth hormone) and testosterone also develops, the secretion peaks of which are noted in the deep stages of sleep. With OSA, deep stages of sleep are practically absent, which leads to insufficient production of these hormones. One of the functions of somatotropic hormone in adults is the regulation of fat metabolism and, in particular, the mobilization of fat from the depot. If there is a lack of growth hormone, the accumulated fat cannot be converted into energy. Thus, all the resulting surplus becomes a “dead weight” that cannot be claimed. A person begins to gain weight, and any dietary or medicinal efforts aimed at losing weight turn out to be ineffective. Moreover, fat deposits at the neck level lead to further narrowing of the airways and progression of OSA, and this in turn aggravates the lack of growth hormone. Thus, a vicious circle is created, which is almost impossible to break without special treatment for OSA. Lack of testosterone in the body leads to decreased libido and impotence in men. The prevalence of OSA in patients with type 2 diabetes reaches 36%. Because of this, and given the proven negative impact of OSA on beta cell function and insulin resistance, the International Diabetes Federation has published clinical guidelines strongly recommending that healthcare professionals working with type 2 diabetes mellitus or obstructive sleep apnea provide clinical practice that , if the patient had one of the diseases, the possibility of having another disease would be discussed. In patients with hypothyroidism, the prevalence of OSA ranges from 25 to 100%.
Clinical picture
Important information to clarify the causes of OSA can be provided by an examination of the ENT organs, which allows identifying anatomical defects at the level of the nose and pharynx (polyps, deviated nasal septum, hypertrophy of the nasal mucosa, excessive soft palate and palatine arches, hypotonic and elongated uvula, hypertrophied tonsils) and evaluate their possible contribution to the development of upper airway obstruction.
Main symptoms:
- · Indications for snoring
- · Indications for sleep apnea
- Frequent awakenings and unrefreshing sleep
- Frequent urination at night (>2 times per night)
- Difficulty breathing, shortness of breath, or shortness of breath at night
- Belching and heartburn at night
- Night sweats
- · Feeling tired in the morning
- · Arterial hypertension (mainly night and morning)
- · Morning headaches
- · Severe daytime sleepiness
- · Decreased potency
- · Depression, apathy, irritability, low mood, decreased memory
The clinical picture in adults and children has certain differences. Adults typically develop severe daytime sleepiness. In children – hyperactivity and attention deficit disorder. Paradoxically, the situation with snoring and OSA in pediatrics has worsened in recent years. This is due to a very conservative approach to the treatment of adenoids and chronic tonsillitis, even with severe hypertrophy of the tonsils. If previously almost all of these children underwent adenoidectomy and tonsillectomy, now they are trying to preserve these lymphoid structures “to the last”, despite the presence of snoring and sleep apnea. OSA in children causes growth retardation and learning problems due to attention deficit disorder. If a child is not able to study normally at the age of 7-15 years, then it will be almost impossible to make up for this gap in the future, even if the tonsils undergo a certain reduction over time and this will lead to a reduction or elimination of breathing disorders during sleep.
Thus, if a child has hypertrophy of the adenoids and tonsils, snoring and indications of respiratory arrest, irritability, restlessness, tearfulness, then OSA must be excluded. Moderate-severe forms of the disease are an absolute indication for tonsillectomy and adenoidectomy in case of hypertrophy of these structures.
Diagnostics
OSA can be suspected based on the patient’s appearance, described in the “Clinical picture” section. Sometimes one glance at a patient entering the office is enough for this. If you ask the patient a few more questions about the presence of snoring, sleep apnea, frequent night urination, restless sleep and daytime sleepiness, then the preliminary diagnosis of OSA becomes obvious. In clinical practice, it is possible to use a fairly simple screening rule, with which you can suspect a disease and prescribe additional examination:
If three or more of the following signs are present (or just the first sign), in-depth evaluation for OSA is necessary:
- · Indications for sleep apnea.
- · Indications of loud or intermittent snoring.
- · Increased daytime sleepiness.
- · Frequent urination at night.
- · Long-term disturbance of night sleep (> 6 months).
- · Arterial hypertension (especially at night and in the morning).
- · Obesity 2-4 tbsp.
It should be noted, however, that this rule does not apply to all patients. Firstly, if a person sleeps alone, then he may not be aware that he snores or that he has sleep apnea. Secondly, patients may become so accustomed to the illness that they do not notice the obvious symptoms of daytime sleepiness. There is a paradoxical situation when a patient falls asleep right at a doctor’s appointment and begins to snore, and when they wake him up and ask him a question about daytime sleepiness, he answers that his sleepiness does not bother him. This situation is especially common among pensioners who have the opportunity to sleep during the day.
In this situation, it is possible to implement an approach to screening for OSA, based on the presence of a number of somatic diseases (see section on pathogenesis), in which the likelihood of having OSA is very high. We believe it is necessary to screen for sleep breathing disorders in patients with a certain list of somatic diagnoses.
A list of somatic diagnoses for which an in-depth study to identify sleep breathing disorders is indicated.
- · Obesity 2 degrees and higher (body mass index >35).
- · Arterial hypertension of 2 degrees and higher (especially at night, morning and refractory to treatment).
- · Cardiac bradyarrhythmias at night.
- · Heart failure of 2nd degree and higher.
- Severe COPD (FEV1<50%)
- · Respiratory failure of grade 2 or higher.
- · Pulmonary heart. · Metabolic syndrome.
- · Pickwickian syndrome.
- · Hypothyroidism (decreased thyroid function).
- · Diabetes mellitus type 2.
TREATMENT
Treatment methods for snoring and OSA are varied and depend not only on the causes, but also on the severity of the disease. They can be divided into the following categories:
- · General preventive measures: - weight loss, - stopping or limiting smoking, - avoiding alcohol and sleeping pills.
- · Positional treatment.
- · Use of electromechanical stimulating devices.
- · Use of pharmacological agents to relieve snoring.
- · Situational provision of free nasal breathing.
- · Use of intraoral devices.
- · Training the muscles of the tongue and lower jaw.
- · Surgical treatment (surgical, laser, radiofrequency)
- · Treatment by creating continuous positive airway pressure (CPAP therapy). Each of these methods is analyzed in detail below.
General preventive measures
Weight loss
In the presence of snoring and OSA, a decrease in body weight by 10% of the original can improve breathing parameters by 50%. This is usually accompanied by a transition to a milder severity of the disease. In some cases, with uncomplicated snoring, it is enough to reduce body weight by 5-7% in order to completely eliminate snoring without any other interventions. There is also the opposite situation. We observed patients who, over a period of one and a half to two years, increased their body weight by 15-20% of the initial one and moved from a mild form of OSA to a severe one.
Stopping or limiting smoking
Smoking causes chronic chemical trauma to the airways at the level of the pharynx, which leads to swelling and decreased muscle tone at the level of the pharynx, and this in turn contributes to the progression of snoring and OSA. Accordingly, patients with sleep-disordered breathing are advised to stop smoking. However, quitting smoking can lead to significant weight gain, which can even worsen the severity of snoring and OSA. Thus, when recommending smoking cessation, it is necessary to weigh the possible benefits against the risks. In obese patients, it is first necessary to achieve a significant reduction in body weight, and only then decide to stop smoking.
Avoiding alcohol and sleeping pills
Alcohol has a double negative effect on OSA. Firstly, it acts as a muscle relaxant and this leads to relaxation of the pharyngeal muscles and more frequent collapse of the airways. Secondly, ethanol increases the threshold of the brain's response to unfavorable stimuli. In this situation, respiratory arrests last longer and more severe hypoxemia develops. Taking a dose of alcohol equivalent to 100 ml of pure alcohol (250 g of vodka - authors' note) in a 70 kg person can worsen the severity of OSA by 50-70%. In severe OSA, drinking large doses of alcohol before bed increases the risk of death. Therefore, it is advisable to stop or significantly limit your alcohol consumption.
Positional treatment
Mild forms of snoring and OSA are often position dependent. In this case, the patient on his side may practically not snore, but on his back he may experience loud snoring and pauses in breathing during sleep. This is due to retraction of the tongue, especially in patients with retro- and micrognathia. There is a simple and effective way to wean a person from sleeping on their back. On night pajamas or a T-shirt, a pocket is sewn between the shoulder blades in which a tennis ball is placed.
In this case, every attempt to lie on your back will end in waking up and turning on your side. At the beginning of using this method, the quality of sleep may deteriorate, especially in people who are accustomed to sleeping on their backs, but within 3-4 weeks a strong conditioned reflex is developed not to sleep on their backs.
Application of electromechanical stimulation devices
Electromechanical stimulation devices are wristband-style devices that detect the sounds of snoring and send weak electrical or mechanical impulses that irritate the nerve endings in the arm and thus stimulate the patient's brain. Quite a lot of varieties of such devices are produced under various brands Snore Gone, Snore Stopper, etc.
These devices give a good effect when the patient only occasionally snores at night or snoring is observed only in the supine position. In this situation, the device can work several times during the night, sleep becomes shallow for a while and the patient stops snoring. Or, in response to the activation of such an “alarm clock,” the patient can change his position, for example, roll over from his back to his side. In fact, it turns out that these devices do not have any therapeutic effect, but only prompt the patient in response to the occurrence of snoring and, figuratively speaking, replace the wife’s elbow.
The use of pharmacological agents to relieve snoring
When snoring, the structures of the airways vibrate and bang against each other, which causes chronic injury, inflammation and swelling. This, in turn, makes snoring even worse. The patient is concerned about dry mouth, sore throat, sensation of a foreign body in the pharynx (with swelling of the uvula), accumulation of difficult-to-remove mucus on the walls of the pharynx in the morning. To relieve the above symptoms, pharmacological agents are used that have local emollient, anti-inflammatory and antiseptic effects. An example of such a drug is Slipex, which is sold in pharmacies without a prescription.
Situational relief of nasal breathing
Difficulty in nasal breathing can significantly increase snoring and OSA. Situationally, nasal breathing can be improved by using special nasal strips to expand the nasal passages “BreezeRight”
These strips, which have springy properties, are glued to the wings of the nose, move them apart and significantly facilitate nasal breathing.
Predicting the effectiveness of strips is quite simple. The patient should be asked to grab the wings of the nose with his fingertips, spread them apart and take several breaths in and out through the nose. If the patient experiences significant relief in breathing, the strips can help improve nasal breathing at night and relieve snoring.
Use of intraoral appliances
Currently, in world practice, a large number of different types of intraoral applicators are used, which are installed on the dentition and provide forward displacement of the lower jaw. This leads to an increase in the anterior-posterior size of the pharynx and relief from snoring.
Surgery
Chronic difficulty in nasal breathing is one of the causes of snoring and OSA. Moderate and severe forms of OSA should be considered as an absolute indication for the elimination of significant chronic nasal obstruction. For mild forms and uncomplicated snoring, especially in older age groups, it is necessary to carefully weigh the possible benefits and risks. In this case, it is necessary to take into account the social significance of snoring for the patient and his desire to eliminate this sound phenomenon.
Surgical interventions at the pharyngeal level include uvulotomy (partial or complete removal of the uvula), tonsillectomy, and uvulopalatopharyngoplasty. The last intervention is the maximum possible removal of tissue at the level of the pharynx, including tonsillectomy, uvulotomy, excision of part of the soft palate and palatine arches. These interventions are quite traumatic and must be used according to strict indications, as they have certain risks (postoperative asphyxia or bleeding; in the long term - a nasal voice and food getting into the respiratory tract). It should also be noted that in severe forms of OSA in obese patients, the positive effect of surgical intervention is achieved only in 20-30% of those operated on. This is due to the persistence of obstruction of the underlying parts of the pharynx at the level of the root of the tongue and the epiglottis.
In any case, the decision on surgical treatment of snoring and OSA should be made by a qualified ENT surgeon, taking into account clinical examination data, polysomnography results and other additional examination methods.
Treatment methods
A common cause of snoring is negative attitudes and feelings of despair. To cure, psychologists recommend doing the following:
- let go of the past, learn to enjoy life in the present;
- accept yourself, find your place in this world;
- learn to value yourself and express your opinions, your feelings;
- learn to listen to other people, seek compromises in difficult situations;
- develop positive thinking, look for sources of positive emotions.
It is important! The true cause of despair may be hidden deep in the subconscious. For faster and more effective treatment, we recommend contacting a psychoanalyst.
In addition to psychotherapy, follow these tips:
- sleep on your side;
- treat inflammation of the nose and throat in a timely manner;
- use traditional medicine to prevent and treat diseases (drops, sprays, inhalations, decoctions).
If swelling of the mucous membrane is caused by allergies, then antihistamines are needed. And if the inflammation is caused by an infection, then antibiotics and antiseptics are needed. It is better to consult a therapist for medication.
Snoring Louise Hay
According to Louise Hay's theory, snoring indicates a person's reluctance to part with outdated stereotypes. Affirmation for healing: “I forget everything in my head that upsets me. I move from the past to the new, fresh, vital.”
Snoring Vladimir Zhikarentsev
According to V. Zhikarentsev, snoring occurs due to fixation on old patterns and attitudes. Healing Affirmation: “I release everything in my mind that is not love and joy. I am moving away from the past into a new, fresh and full of life present.”
Snoring Liz Burbo
With the help of snoring, a person is relieved of the stress accumulated during the day. This affects timid people and those who are forced to restrain themselves during the day. And behind this there may be a fear of being rejected.
For healing, it is important to understand that until you accept yourself, snoring will push other people away from you. People around us treat us the way we treat ourselves. Learn to express your opinion. You are worthy of attention. Learn to listen to others and respect yourself, then other people will begin to listen to you and recognize your opinion.
It is important! Traditional and folk medicine, surgical therapy and psychotherapy are used to treat snoring. If the cause is physiological, then medical treatment is necessary. For example, a deviated septum requires reconstructive surgery. And inflammation requires a course of treatment with a spray. Without treatment, snoring will further irritate your organs and further weaken your muscles.