A small appendage, the testicular hydatid, located at the top of the testis in men, is considered an absolutely useless rudiment, the same as the coccyx or wisdom teeth. However, in case of pathology - torsion or bending - it brings a lot of troubles.
If you do not consult a doctor in a timely manner, the process becomes acute, leading to necrosis of the hydatid. In this case, the patient will have to have the scrotum removed.
Appointment with a urologist - 1000 rubles. Comprehensive pelvic ultrasound - 1000 rubles. Appointment based on ultrasound or test results - 500 rubles (optional)
CLICK TO MAKE AN APPOINTMENT or ultrasound tests
Why does hydatid torsion occur?
Hydatid testis, being in a normal physiological state, does not cause any inconvenience to a man - many do not even know about the existence of this organ. Hydatid torsion can be caused by trauma to the scrotum. The development of the disease is also possible with strong contractions of the muscles associated with the testicle. This condition can be caused by physical overload during heavy lifting or sex, banal hypothermia, or a strong emotional outburst.
The pathology is more common in children during the maturation of the connective tissues of the scrotal organs. This is due to the imperfection of the nervous regulation of muscles in children, as well as the fact that the connective tissue of children contains more fluid than that of adults.
As a result of torsion or bending, the organ is not supplied with blood, the tissues fester (the testicles melt into pus) and gradually die. But even if the body somehow copes at one of the stages, infertility for the patient is practically guaranteed.
Diagnosis of testicular torsion
If torsion is suspected, a careful examination of the patient and palpation of the organ suspected of pathology is carried out. Based on the clinical picture, a preliminary diagnosis can be made.
To confirm it, an ultrasound of the scrotal organs with Doppler and diaphanoscopy are performed.
Diagnosis of testicular torsion includes orchitis, epididymitis, trauma and some other abnormalities. Torsion is distinguished from orchitis by its more acute onset, and from epididymitis by the nature of the pain syndrome (the pain intensifies when the scrotum is raised, and with epididymitis it weakens). The cremasteric reflex practically disappears during torsion, in contrast to inflammatory processes of the testicle. Less often it is necessary to carry out a differential diagnosis of testicular torsion with its hydrocele, strangulated by an inguinal hernia.
With torsion, laboratory tests are of little value. The same cannot be said about instrumental studies. The most indicative is an ultrasound examination with Doppler ultrasound - it detects all blood supply disturbances in the organ. Dynamic testicular scintigraphy can also be performed. Unfortunately, it is not widely available. Endoscopic diagnosis is rarely practiced.
In difficult cases, when there is doubt about the diagnosis or in emergency situations, as well as when receiving ambiguous results from instrumental studies, they resort to diagnostic dissection of the scrotum and revision of the testicle.
Symptoms of hydatid torsion
At the beginning of the disease, the patient feels severe pain in the left or right half of the scrotum, it becomes very swollen and red. Then the swelling subsides, and in its place a hydatida (another name is the testicular appendix) becomes noticeable. This is a small formation (about the size of a bean) of bright crimson, closer to black or blue. Touching this area causes severe pain.
In adults, these are sometimes the only symptoms; in children and adolescents, the body reacts more strongly - a high temperature may rise and vomiting may begin.
The disease is easy to diagnose even in the early stages using diaphanoscopy - the doctor examines the scrotum with a special flashlight. Further diagnostics can go in two directions:
- An ultrasound of the scrotum
is performed , thanks to which the urologist accurately determines the size of the formation and its position, and also establishes the location of the intended incision for the operation. - The urologist opens the scrotum
and immediately examines and removes the pathology.
How the diagnosis will be carried out depends on the condition in which the patient was admitted and other indications - the choice of method is solely within the competence of the doctor.
Pediatric urology PEDUROLOGY.RU
COM is an acute condition characterized by the main symptoms – pain, swelling, hyperemia of half of the scrotum. Occurs as a result of injury, torsion of the testicle or epididymis, necrosis of the hydatid of Morgagni, orchiepididymitis. Orchitis and epididymitis in most cases do not require urgent surgical treatment.
The causes of acute testicular diseases are considered to be excessive mobility of the testicle during contraction of the muscles that lift the testicle, during physical activity or erection, and trauma to the scrotum.
Testicular torsion.
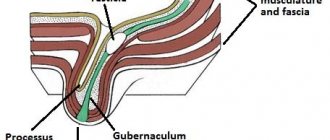
In the literature, extravaginal testicular torsion (true torsion of the spermatic cord from the external inguinal ring downwards), characteristic of newborns, and intravaginal testicular torsion are distinguished.
It is generally accepted that the cause of testicular torsion in newborns is free rotation of the testicle as a result of weakened or absent connection of gonadal tissue to the scrotum, although the etiology remains unclear.
The following components are important in the development of torsion:
Excessive testicular mobility associated with weak attachment of the testicular membranes in a newborn; abnormal attachment of the gubernaculum and lack of fixation of the undescended testicle; deformation of the testicle located in the scrotum in the form of a “bell tongue”. The term “bell tongue deformity” is used to describe an abnormally high transition of one layer of the tunica vaginalis to another, as a result of which the testicle appears to hang like a bell tongue inside the tunica vaginalis and can freely rotate around the longitudinal axis of the spermatic cord. Contraction of the cremaster fibers, provoked by injury, exercise, exposure to cold or irritation of the genital organs, stimulates rotational movements of the testicle, similar in nature to the movements of the tongue of the bell, which ultimately leads to ischemia.
Neonates account for 10% of all cases of testicular necrosis associated with torsion.
If torsion occurs in utero, after birth, a dense, painless formation is determined in the scrotum; the skin of the scrotum may be discolored, ecchymoses, and edema. In such cases, the testicle is rarely viable. Fixation of the contralateral testicle is necessary to prevent possible future twisting and necrosis.
The main symptom of testicular torsion is pain, usually acute. The pain may radiate to the groin area and lower abdomen. (When examining a child with abdominal pain with suspicion of acute appendicitis, it is necessary to examine the scrotum. This may include radiating pain due to testicular torsion, as well as torsion of an undescended testicle). Testicular torsion may be accompanied by nausea and vomiting. Testicular torsion lasting more than 12-24 hours carries a poor prognosis.
The gradual appearance of unpleasant sensations in the scrotum area, turning into increasing pain within 12-24 hours, is more typical for epididymal torsion or orchiepidymitis. It is possible to develop specific orchitis as a complication of mumps.
Urinary tract symptoms such as frequent urination, painful urination, pyuria; Fever may occur with epididymitis.
Hyperemia and swelling of the scrotum occur with any disease manifested by edematous scrotum syndrome.
Upon examination, local pain in the epididymis or testicle may be detected, which helps in the differential diagnosis of the condition.
There are no pathognomonic symptoms for testicular torsion, but some authors attach some importance to changes in anatomical relationships: abnormal position of the testicle lying transversely, anterior location of the epididymis, elevated (tucked up) position of the testicle due to shortening of the cord and absence of the cremasteric reflex on the affected side.
The “blue dot” symptom is characteristic of necrosis (torsion) of the hydatid of the epididymis and the testicle itself. Appendages of the epididymis can be located on the head of the epididymis, its body or tail. There is also paradidymis - an appendage appendage of the testicle or Giraldes organ, which is located most proximally, but can also be located along the spermatic cord, and sometimes extends from the cord to the distal part of the inguinal canal, located significantly above the testicle.
If testicular torsion is suspected, emergency surgery is indicated. An inspection of the corresponding half of the scrotum is performed. By opening the membranes, the diagnosis is clarified. The effusion can be hemorrhagic, transparent, with a pronounced inflammatory process, cloudy, purulent, with fibrin flakes. The testicle and epididymis are examined.
With necrosis of the hydatid, the last changed, black or cherry color is removed. With testicular torsion, the color is cherry or bluish-black. The torsion is eliminated, the testicle is warmed with napkins with a warm isotonic solution, and the spermatic cord is blocked with a novocaine solution. If viability remains, the testicle is fixed. If, after performing all conservative measures, there is no change in the condition of the testicle, the necrotic testicle is removed. The contralateral testicle is fixed.
With orchiepidymitis, the testicle and epididymis are enlarged, injected with vessels, purulent effusion, and fibrin deposits are present. Fibrin and effusion are evacuated; in case of pronounced purulent process, a rubber graduate is left.
In case of bruise and hematoma of the testicle, the hematoma is emptied, non-viable tissue is removed, and in case of testicular ruptures, it is sutured behind the tunica albuginea.
If the testicle is torsion in the inguinal canal, the incision is made according to the inguinal canal; if necessary, it is opened and the torsion is eliminated. If immersion is possible, it is fixed in the scrotum. When tensioning the elements of the spermatic cord, the testicle is left in place.
In the postoperative period, antibiotics are prescribed, wearing a suspension, in case of severe inflammation and after straightening the torsion - blockade of the spermatic cord a\b + novocaine. After organ-conserving surgery, complex therapy is prescribed to relieve the autoimmune reaction.
If an organ-removing operation is performed, in the future the testicle will be replaced with a silicone prosthesis of the appropriate size.
Diagnostics.
In clinical cases of testicular torsion, emergency surgical treatment is indicated.
In situations where the clinical picture is not obvious, it is possible to use diagnostic methods.
Ultrasound allows you to clarify the anatomical changes of the scrotum and its contents, changes in echogenicity. Dopplerography allows one to judge the blood flow in the testicle, whether it is depleted or increased. The published literature describes the use of testicular isotope scintigraphy. When torsion occurs, there are 3 phases, depending on the duration of the disease. The early phase (first 6 hours) shows normal current, the same on the contralateral side, or more often reduced. The middle phase (next 18 hours) reveals a halo of increased activity around an unchanged center. In the late phase, there is a sharp increase in radioactive radiation around the low-activity center.
Epididymitis manifests as a marked increase in blood flow on the affected side in the absence of an area of hypoperfusion.
The duration of torsion has a detrimental effect on both viability and its subsequent development. Experiments on animals revealed that severe changes were observed in Sertoli cells after 4 hours of ischemia, Leydig cells were more stable, but were almost completely destroyed after 10-12 hours of ischemia.
A number of studies have revealed varying degrees of infertility and suppressed spermatogenesis in men who suffered unilateral testicular torsion with corresponding abnormalities in sperm tests, and the degree of abnormalities depended on the duration of ischemic testicular damage. However, it is not clear enough whether these changes were the result of testicular abnormalities that preceded torsion, which were the cause of torsion, or the result of an autoimmune lesion of the contralateral testicle that already existed at the time of surgery. You need to realize that leaving the testicle after eliminating the torsion with ischemia lasting more than 24 hours may not be harmless.
For allergic edema of the scrotum, as well as with Quincke's edema, the entire scrotum is enlarged, the liquid permeates all its layers. Palpation in this case is not painful.
If you would like more information, please
contact us or see your doctor for
specific recommendations for diagnosis and treatment.
For many questions, an online consultation with a urologist is possible -
https://pedurology.ru/index.php/on-line1
Is it necessary to treat the testicular appendix and what will happen if it is not treated?
If the twisting and bending of the hydatid is not treated, severe inflammation develops in the scrotum, instantly spreading to the surrounding tissues. As a result, the patient can expect complications:
- Hydrocele of the testicle
– the lymphatic structures of the scrotum are affected, which can lead to complete atrophy of the testicle; - Epididymitis
- this inflammatory process, flowing into a chronic form, leads to infertility; - Testicular atrophy
is a violation of all testicular functions, tissue necrosis, purulent melting of the scrotal structures.
Due to the high probability of developing these complications, hydatid torsion requires immediate contact with a urologist and surgery.
Treatment of hydatid torsion: surgery only
The only correct solution for testicular appendix torsion is surgery. In adults, the intervention is performed using local anesthesia. Children are operated on under general anesthesia.
The surgical operation is performed through an incision above the upper pole of the testicle, which has a pathological neoplasm. During examination of the organ, an almost black, bean-shaped formation is discovered. The hydatid is removed, followed by a set of measures for processing and suturing the incisions. To prevent and prevent infection after surgery, patients are prescribed antibiotics.
To avoid infection, postoperative sutures must be cleaned regularly. Approximately, sutures are removed 6-8 days after surgery.
Rehabilitation after surgery
In case of hydatid torsion, rehabilitation measures are aimed at preventing infectious inflammation in the scrotum. For this, the patient is prescribed antibacterial drugs.
You also need to pay attention to seam hygiene. It should be washed daily and treated with antiseptic solutions. Postoperative sutures are removed 7-10 days after surgery.
It is important to know! Since this type of operation is not considered complex or traumatic, wearing elastic support trunks is not required. Throughout the entire period of recovery of the body, the patient should avoid hypothermia of the genitourinary system and observe bed rest. UHF therapy, the essence of which is to heat the affected organ with light, will help speed up the healing process.
Three myths about the treatment of hydatid torsion
Myth No. 1. The hydatid leg will straighten itself
Twisting and bending of the hydatid stalk will not go away on its own.
If the pathology is not eliminated, severe inflammation is guaranteed, easily spreading to surrounding tissues. Due to the risk of complications with hydatid torsion, surgery is urgently performed.
Myth No. 2. Testicular hydatid torsion can be treated with medications.
Stories about drug treatment and manual reduction of the hydatid are fairy tales. But you will still have to take pills - anti-inflammatory and painkillers. This will help avoid postoperative pain and complications.
It is impossible to correct the position of the hydatid manually. Moreover, carrying out such manipulations is dangerous. When pressed, the abscess will burst and the infection will spread throughout the scrotum.
Myth No. 3. Removing hydatid is difficult and dangerous
Testicular surgery is performed urgently in the clinic without special preparation. The urologist carefully dissects the testicular tissue and removes the twisted hydatid. Local anesthesia is sufficient for the procedure. If everything is done under sterile conditions, there is nothing dangerous in the operation.