Hello, friends!
For those who have carefully studied the technology of laser vision correction, carefully read the article about patient impressions, read the opinions of specialists and saved up money for the procedure, today I will talk in more detail about contraindications for the operation.
I believe that this information will be necessary for those people who have decided to take a bold step - surgical restoration of vision.
[direct]
What is laser vision correction
Human vision is the means by which we receive information from the environment.
Moreover, more than 80% of information perception occurs through the eyes, so any even slight visual impairment causes significant discomfort. The human eye is a complex mechanism. Light rays passing through the cornea, lens and vitreous body are naturally refracted and reach the retina. Afterwards, the signals are transmitted via the optic nerve to the brain, processed in its corresponding zone - and the person receives a clear image. With myopia and farsightedness, light rays are focused not on the retina, but behind or in front of it, and the picture turns out blurry.
The goal of any vision correction is to change the refractive power of the eye so as to “collect” the rays precisely on the retina. It is for this purpose that people wear glasses and contact lenses. However, these correction methods provide good vision only for the time they are used and do not relieve a person from the problem of poor vision.
Laser vision correction or refractive surgery is a medical procedure using modern laser technologies to correct the following diagnoses:
- myopia (nearsightedness);
- hypermetropia (farsightedness);
- astigmatism.
Unlike glasses or contact lenses, laser correction radically solves the problem of poor vision, and no additional devices will ever be needed to see perfectly.
Causes of age-related farsightedness
The apple shell, in turn, is divided into outer, middle and inner (mesh), of which it is the mesh that is capable of perceiving light flux. However, an object can be displayed not on the segment of the retina itself allocated by Nature, but on the plane behind it. This phenomenon occurs with farsightedness, which accompanies almost every person who has crossed the 45th milestone in life. Such natural farsightedness, also called presbyopia, is characterized by the display of a nearby object on the retina in the form of an indistinct (blurry) image. The reason for the loss of visual acuity in this case is the thickening of the lens substance and laxity of the ciliary muscle that comes with age, as well as a weakening of the accommodative functions of the eyes.
The more significant the manifestations of such age-related changes, the more farsightedness makes itself felt, allowing a person to clearly see objects only at an increasingly distant distance. Correcting farsightedness with the help of glasses and contact lenses is, of course, very successful, but does not solve the problem at its roots. If the loss of visual acuity is significant, and the accommodation of the eye leaves much to be desired, then the patient, of course, needs treatment. Modern ophthalmology comprehensively answers the question of how to correct vision with farsightedness, offering more than twenty solutions for this.
The doctor will help you choose the method that is suitable for the patient, taking into account the characteristics of the patient’s disease and the accompanying factors in his life. In case of any deviations, specialists combine various technologies to achieve the most successful solution to the problem. When choosing, you need to consider:
1. Features of the work, because for some specialties, for example flight, certain options for vision correction are prohibited.
2. The nature of physical activity. Sports and work activities that involve the possibility of head injury and blows to the face and eyes may also influence the choice of method.
3. The presence of certain diseases and conditions in the patient (diabetes mellitus, pregnancy, insufficient body immunity, etc.) can affect the outcome of the surgical intervention.
4. Existing eye diseases: glaucoma, inflammatory processes, herpes virus and previous surgical interventions on the organ may be a contraindication for some treatment options, even prohibited.
Vision correction methods
In general, the following types of visual acuity correction are used in medicine:
- Spectacle correction is all types of glasses that can increase the acuity or improve the quality of a patient’s vision. Nowadays, there are many materials and filters used to make spectacle glasses.
- Contact correction - contact correction is the correction of vision using contact lenses that are placed directly on the surface of the eyes.
- Surgical correction - surgical vision correction includes all surgical interventions that will ultimately help the patient see better. Most often, such manipulations are necessary for various diseases.
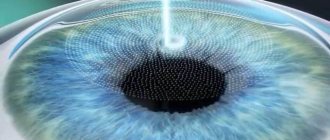
- Laser vision correction differs from conventional surgery in that there is no direct contact of any instruments with the eye. All manipulations are performed using a directed laser beam. The three most common types of laser vision correction are photorefractive keratectomy (PRK), LASIK and ReLEx SMILE. Their main difference is in the methodology and scope of application of the tools:
1. PRK (PRK) - the effect is performed directly on the outer surface of the cornea;
2. LASIK (Laser keratomileusis) - influence on the internal layers, which are previously exposed by a tangential cut of a surgical instrument and bending the resulting valve; 3. ReLExSMIL on the inner layers, but without forming a valve. The principles of PRK and LASIK, in fact, are not competing, they even complement each other. It is customary and more expedient to perform operations to correct myopia and complex astigmatism associated with myopia using superficial methods such as PRK; the correction of other refractive errors is more effective when using valve technologies, that is, LASIK.
Surgical treatment of farsightedness
The term “surgical treatment of farsightedness” means surgical intervention or laser correction of farsightedness. Surgical treatment of hyperopia, regardless of the technique used, is the fastest and most effective way to correct farsightedness. Surgical correction of farsightedness lasts for several minutes under local anesthesia, and the patient can be discharged home on the same day. Surgical treatment of farsightedness, regardless of the method, consists of enhancing the refractive ability of the farsighted eye. Each of them has its own indications and contraindications. Taking into account all the examination data, the doctor will suggest the most optimal operation for your eyes.
Laser correction for various visual impairments
Hyperopia, also known as farsightedness, is a condition of the organs of vision in which the image is focused in the plane behind the retina, and not on it. As a result, all objects become blurry. Hypermetropia can occur at any age.
What unites age-related and normal farsightedness is the fact that it is difficult for a person to focus vision on an object nearby: the image “floats”.
Laser correction is an effective way to restore vision in mild to moderate farsightedness, which will allow you to forget about glasses or contact lenses for many years.
Advantages of laser surgery:
- rapid recovery - 1 - 2 days after surgery;
- minimal restrictions after surgery;
- preservation of the corneal structure;
- no wounds;
- minimum pain - 2 - 3 hours after surgery;
- laser correction of farsightedness provides stable results and a lasting refractive effect;
- It is recommended to treat farsightedness in both eyes at once;
- absence of corneal opacification in the postoperative period;
- the ability to correct high degrees of farsightedness, including astigmatism.
Myopia or simply myopia
- This is a violation of refraction - the refraction of light in the eye. As a result of the disease, an image is formed in front of the retina; in order to focus on an object, a person needs to hold it directly in front of his eyes. Myopia can be congenital or acquired, and usually worsens with age.
Surgeries for myopia are classified as cosmetic. This means that there are no absolute indications for their implementation; it all depends on the patient’s desire, his desire for comfort and refusal to use glasses and contact lenses.
Advantages of laser surgery:
1. Safety—observations of patients have shown that this type of intervention is safe and very effective. 2. Possibility of use for various eye diseases - if patients have no contraindications, laser treatment will help restore good vision in many eye diseases. 3. Speed of the operation—the duration of the procedure is no more than 15 minutes. 4. Painlessness—the patient only feels touch during the operation. 5. Stable results - provided the patient does not have progressive myopia, the correct shape of the cornea after laser correction will remain for many years.
Astigmatism
- a common visual impairment caused by congenital changes in the shape of the cornea. Astigmatism occurs due to deformation of the two main meridians of the eye - vertical and horizontal. The refractive power along the main corneal axes determines the type of astigmatism:
- Direct astigmatism - the maximum refractive power is observed at the vertical meridian.
- Reverse - occurs when the greatest refraction occurs in the region of the horizontal axis.
- Astigmatism with oblique axes - due to deformation of the cornea, the main meridians do not coincide with the horizontal and vertical axes of the eyeball.
Surgeries for astigmatism using laser energy have now become popular. Such methods allow treatment to be carried out as quickly as possible and with the least likelihood of side effects. The benefits of laser intervention are the same as for myopia and farsightedness.
Relative restrictions
Relative limitations mean such temporary conditions that turn laser correction into an unsafe operation, and therefore extremely undesirable. They should definitely be discussed with a refractive surgeon. The procedure is postponed until the patient recovers or there is a need for emergency surgery.
This is first of all:
- Infectious processes: tuberculosis, hepatitis B, etc.;
- An inflammatory disease of the body can negatively affect postoperative vision restoration;
- Malignant neoplasms of various localizations;
- Inflammatory eye diseases, especially in the acute stage: conjunctivitis, blepharitis, keratitis. Surgical intervention can cause an exacerbation of the existing inflammatory process and contribute to the further spread of infection, which can cause serious complications;
- Decreased immunity. The state of the immune system is reflected in the speed of all regenerative processes occurring in the body. Weakened immunity can cause a prolongation of recovery time for damaged cornea;
- Allergic diseases;
- Presence of a pacemaker;
- Pregnant and lactating women. During pregnancy and breastfeeding, the body maintains an unstable hormonal balance, and any surgical manipulation can change it unpredictably. In addition, drops and gels prescribed as antibiotic therapy during the recovery period can pass through the placenta or breast milk into the baby’s body and cause harm to his health;
- Dry keratoconjunctivitis of moderate and low severity;
- Deformation of the eyelids;
- Epithelial keratitis and its consequences, herpetic keratitis (a laser beam can contribute to the activation of the herpes virus and provoke an exacerbation of the disease);
- Increased intraocular pressure is subcompensated;
- Congenital lens opacity (not corrected with glasses and corrected with glasses);
- Dystrophy of the retina of the eye. In this case, preliminary laser coagulation is required;
- Operated retinal detachment (depending on the degree of stabilization of the process and the location of the lesion);
- Newly developed visual impairment.
There are several individual restrictions for prescribing surgical correction using the LASIK method:
- The cornea should have an optical power ranging from 39 to 49 diopters;
- Sunken position of the eyeball in the orbit (enophthalmos);
- Cornea with a radius of less than 5 mm;
- The thickness of the cornea in the central part is less than 480 microns;
- Astigmatic difference more than 7 diopters; eyeball of small diameter.
Special limitations characteristic of the PRK method:
- Inflammatory and infectious lesions of the eyes and eyelids, especially in the acute stage;
- Severe lagophthalmos is a disease manifested by impaired eyelid closure;
- Epithelial keratitis and its consequences;
- Tendency to keloid formations;
- Neurotrophic diseases;
- Congenital cataract;
- Carrying and breastfeeding a child; endocrine disorders.
The FEMTO-LASIK laser correction technique allows refractive treatment for patients with insufficient thickness of the cornea, dry keratoconjunctivitis and a number of other visual impairments. It eliminates the occurrence of negative consequences, individualizes the corneal flap, changes it depending on the characteristics of the eye and provides excellent correction results.
Indications and contraindications for laser vision correction
Surgery for deviations from normal vision is prescribed in the following cases:
- degree of pathology from 3 diopters;
- mixed astigmatism with farsightedness;
- inability to wear contact lenses and glasses.
Surgical intervention is not prescribed:
- children under 18 years of age and adults over 45 years of age;
- patients with only one visual organ;
- for infectious and psychological diseases;
- in case of oncological pathologies;
- during breastfeeding and childbearing;
- for diseases of the cardiac and endocrine systems;
- with diabetes mellitus.
Important! For patients who are not eligible for laser surgery, alternatives are offered, such as lens implantation, tangential and arcuate keratomy, refractive lens replacement, and other surgical options.
Phakic lens implantation
Phakic lens implantation (IOL) involves placing an additional diverging (“positive”) lens directly onto the lens, which focuses light rays entering the eye onto the retina. Usually, phakic lens implantation is carried out at a young age and with large degrees of hypermetropia, which cannot be corrected by excimer laser vision correction. The IOL is implanted into the eye cavity through a puncture, without suturing. The biocompatibility of the lens material minimizes the risk of complications. The operation and postoperative period are painless, vision improves within a few hours after the intervention. The advantages of this operation include, among other things, the possibility of removing the lens, that is, returning the eye to the preoperative state.
If there is opacification in the lens due to hypermetropia, the lens is replaced for refractive purposes. This operation is similar to that performed for cataracts. Currently, when carrying out such an intervention, the method of phacoemulsification, or crushing the lens using ultrasound, is used. The natural lens is removed through a 2-3 mm puncture, and a soft artificial lens is implanted in its place, designed in such a way that the patient no longer needs distance correction. And recently, a number of large manufacturers have developed and are introducing multifocal artificial lenses, which allow one to see well not only near or far, but to combine sufficiently high vision for both near and far. This happens due to the fact that each such IOL has several focal lengths. True, quite often the patient needs to get used to such a correction.
The choice of tactics for surgical treatment of farsightedness is strictly individual and is determined based on the results of a complete ophthalmological examination. Since refractive surgery is the method of choice, the decision to undergo correction is made by you. We will help you find your way - recommendations depend on your age, general health, existing or pre-existing eye problems, your glasses or contact lenses, lifestyle, profession, work goals and the results you expect from the operation.
Laser surgery and patient age
The permissible minimum age at which laser vision correction can be performed is 18 years. If the procedure is carried out earlier, the result will not be final, since in children the eye tissues go through a developmental stage and the refractive properties of the corresponding elements of the eye gradually change, reaching a stable position by about 18 years.
After 45 years, people experience age-related hardening of the lens, which becomes increasingly difficult to adapt to optical conditions, and the muscles that hold it weaken, and the eye loses the ability to focus. This means that, starting from the age of 45, all interventions are performed after a thorough diagnosis and for serious indications. Doctors generally do not recommend any surgery to improve vision for people over 55 years of age.
Prevention and treatment of complications of farsightedness
If you have developed complications of farsightedness such as amblyopia, impaired binocular vision or strabismus, you need comprehensive treatment to improve visual acuity. Treatment includes various types of stimulation: laser, magnetic, classes on computers equipped with unique programs, as well as a number of other latest devices. If indicated, no earlier than 1 month after excimer laser surgery, you may be recommended to undergo surgical correction of strabismus.
You can find out more about lens replacement in the treatment of astigmatism here
Photorefractive keratectomy (PRK, Trans-PRK)
This is the oldest method of laser vision correction, which, however, has not lost its relevance today. Of course, modern PRK is significantly different from that used since 1985, at the dawn of excimer laser ophthalmic technology. And yet its essence remains the same.
The PRK operation consists of two stages. At the first stage, the top layer of the cornea - the epithelium - is removed to access the stroma, on which the correction is carried out. In outdated PRKs, this stage was performed by scarification - mechanical scraping. Today, the mechanical process has been replaced by laser action. The second stage of the operation is ablation (laser evaporation) of the corneal tissue until the required geometry of the natural lens is achieved. Both in the early method and now, it is performed with an excimer laser, however, modern laser systems have made it possible to transform a two-stage operation into a one-step operation, which has returned the relevance of an already outdated technology.
Today's methods of photorefractive keratectomy have received the prefix “trans” and have gotten rid of half of their former “disadvantages”. But the modified Trans-PRK is suitable only for people with a slight or moderate degree of myopia (up to -6 diopters), is accompanied by severe pain and discomfort in the first days after surgery and has a long period until complete restoration of vision (one month). In addition, scars on the cornea obtained during surgery can cause haze phenomena.
Among its undeniable advantages are:
- speed of operation;
- the possibility of vision correction for people with thin corneas and orbital features;
- no restrictions on active lifestyle in patients in the long-term period.
How to make the right choice?
The first thing a person who decides to perform excimer laser correction of myopia needs is to make an appointment with a specialist in a clinic that can offer, if not all, then most of the modern methods of laser vision correction.
Based on the results of a complete ophthalmological examination, the laser surgeon will give recommendations on the most suitable laser correction methods, taking into account the person’s profession, lifestyle, wishes and financial capabilities, as well as the presence or absence of contraindications.
It is worth knowing that if myopia is more than 15 diopters, it is generally not advisable to perform laser vision correction, because the thickness of the cornea after laser ablation will become critically small, which can lead to many complications. An alternative option for such patients may be implantation of an artificial lens inside the eye, which will help restore 100% vision.
Contraindications
There are many contraindications that make the procedure impossible:
- Infectious and viral diseases in the acute stage. Vision correction is possible after complete recovery, elimination of all symptoms, and repeated laboratory tests.
- Diseases affecting the immune system. These include rheumatism, rheumatoid arthritis, HIV, AIDS. If a patient with this diagnosis undergoes laser correction, the tissue will take a very long time to heal.
- Progressive decrease in visual acuity. Carrying out the procedure is irrational, since after it the vision will reappear.
- Minor age. Doctors recommend performing the procedure after 25 years, since by this time the eyeball will have fully grown. If vision correction is performed earlier, visual acuity will decrease again due to age-related changes. The correction will be irrational and a repeat operation will be required.
- Pregnancy and lactation. It is recommended to perform the operation 6 months before pregnancy. This is due to the fact that after exposure to the laser, the retina may detach during childbirth, as the woman actively pushes. If a caesarean section is planned, there are no contraindications to the procedure. Laser correction during breastfeeding is not recommended, as it is very stressful for the woman; local anesthetics that pass into breast milk are used.
- Thinning of the cornea. High risk of rupture. This will lead to a sharp deterioration in the quality of vision, up to complete blindness. The procedure is completely contraindicated for keratoconus, when the cornea protrudes forward, which leads to its thinning.
Since there are many contraindications to the procedure, it is recommended to undergo timely consultation with all specialists in order to identify deviations in health status.
Indications
Laser correction for farsightedness is permitted if visual acuity is impaired by no more than 6.0 diopters. In the case of this pathology, the light beam is focused behind the retina and patients have difficulty seeing nearby objects. But there is presbyopia - a special type of hypermetropia. It is characterized by the same manifestations, but the etiology of its occurrence is different. In the case of presbyopia, the lens of the eye is damaged due to age-related changes. This is typical for people over 50 years old.
It is important to be able to distinguish age-related farsightedness from true hyperopia, since treatment tactics are different.
Features of the operation
Each method of laser vision correction has its own distinctive features. There are also common features associated with the technological sequence of the process. Operations take place in several stages^
- Separation of the corneal flap (using a cutting instrument or beam).
- The flap is pulled back. The laser acts on the cornea until the necessary parameters are acquired.
- The flap is returned in place to heal.
The features of this type of operation are:
- bloodlessness;
- contactless;
- Vision correction occurs thanks to a laser beam through short flashes of light.
During the operation, local anesthesia is used, but unpleasant sensations may occur: burning or stinging in the eyes.
A neoplasm that is not life-threatening, but interferes with life, is xanthelasma of the eyelids.
The presence of a pacemaker is a direct contraindication
A disease that prevents vision at dusk and in low light is night blindness.