Uveitis that develops with Fuchs syndrome is also called heterochromic Fuchs cyclitis. This chronic non-granulomatous inflammatory disease is characterized by gradual development. At a young age, eye damage is usually detected on only one side.
Quite rarely, it is detected in children or affects both eyeballs. This disease occurs in approximately 4% of patients with uveitis, but it is often misdiagnosed. Heterochromia may be absent or invisible, especially in patients with brown eyes. Therefore, diagnosis should be carried out only in daylight and with a dilated pupil.
Symptoms of the disease
With this disease it is noted:
- Gradual decrease in visual acuity due to the development of secondary cataracts.
- The presence of constant floating opacities.
- Difference in the color shade of the iris in different eyes.
- This condition is usually diagnosed accidentally.
Fuchs syndrome is accompanied by the development and formation of:
1. Corneal precipitates, which are considered pathognomonic signs. They are usually quite small, gray or white, star-shaped or round in shape, and cover the surface of the entire endothelial layer. They may appear or disappear, but are not pigmented and do not merge with each other. Fibrin fibers are usually detected along with precipitates. 2. There is a weak opalescence of the aqueous humor, the number of cells in which is +2. 3. Infiltration of vitreous cells is often a leading sign of the disease.
During gonioscopy, changes are either not detected or are detected:
- Light radial vessels in the anterior chamber of the eye that look like branches. They lead to the formation of hemorrhages on the side opposite to the puncture of the anterior chamber of the eye (Amsler's sign).
- Membrane formations in the corner of the anterior chamber of the eye.
- Small anterior fusions (synechia) of irregular shape.
Signs (symptoms) of Fuchs' dystrophy
In the early stages of Fuchs' dystrophy, there is usually increased intolerance to bright light and glare. As the disease progresses, vision deteriorates in the morning and recovers somewhat in the evening. This is due to the fact that when the eyes are closed during sleep, moisture from the surface of the cornea does not evaporate, accumulating inside. During the day, open eyelids “turn on” the mechanism for removing intraocular moisture from the cornea, and a temporary normalization of the condition occurs. The progressive death of more and more endothelial cells leads to a gradual decrease in vision.
The main signs of endothelial dystrophy are considered to be the following:
- Deterioration of vision after sleep, blurry vision.
- Fluctuations in visual acuity.
- Glare (glare) when looking at a bright light source.
- Poor tolerance to intense light.
- Discomfort and feeling of sand in the eyes.
Fuchs endothelial dystrophy is characterized by bilateral damage. The disease is more common in women after 30-40 years of age. In case of serious deterioration of vision, when the ability to self-care is lost, the question of a corneal transplant arises.
Iris changes
The following changes are detected on the side of the iris:
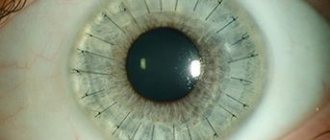
1. The presence of posterior synechiae, which form after cataract removal. 2. Widespread atrophy of the iris stroma, which includes the absence of iris crypts and a change in color to a faded direction. The dullness of color in the area around the pupil is especially noticeable. Due to the loss of supporting tissue, bulging of the radial vessels of the iris occurs. 3. With atrophy of the posterior pigment layer, a spotty appearance occurs, which is revealed by retroillumination. 4. Nodules form on the iris. 5. Rubeosis of the iris occurs, in which irregularly shaped, delicate neovascularization appears. 6. With atrophy of the pupillary sphincter, mydriasis occurs. 7. The formation of crystalline deposits in the iris is rarely detected. 8. Heterochromia is a very important diagnostic sign.
Treatment in Italy
Russian Medical Server / Treatment in Italy / Center for the treatment of rare diseases in Milan / Fuchs’ heterochromic iridocyclitis - treatment in Italy
Iridocyclitis is an inflammation of the choroid of the anterior part of the eyeball; in essence, iridocyclitis is anterior uveitis. Most often, the disease develops in active working age (20–40 years) and has a chronic relapsing course.
Let us recall that the anterior section of the choroid of the eye includes the iris and ciliary body, inflammation of the iris is called iritis, and the inflammatory process in the area of the ciliary (ciliary) body is called cyclitis. Due to the close location and the presence of a common blood supply network, isolated inflammation of any one of the structures of the choroid of the anterior part of the eye is practically not observed, and usually we are talking about combined inflammation, i.e. about iridocyclitis.
The inflammatory process in iridocyclitis is usually one-sided. The severity of the symptoms of the disease depends on the cause of the disease, as well as on the state of the patient’s immune system. The first signs of iridocyclitis are usually pain of varying intensity; patients also complain of blurred vision (the appearance of a “veil” before the eyes). In acute iridocyclitis, the pain increases quite quickly and can become unbearable. Swelling of the iris causes constriction of the pupil, and photophobia appears.
A characteristic sign of iridocyclitis is increased pain when pressing on the eyeball. The visible vessels of the mucous membrane of the eye are dilated, the color of the iris due to inflammation may become red, rusty or greenish, while the pattern of the iris is smoothed out, details are not distinguishable.
Very often (in about 70% of cases) iridocyclitis takes a chronic, relapsing course. In this case, the symptoms of the disease are less pronounced, complications often arise, the most common of which are adhesions (synechias). With iridocyclitis, adhesions usually affect the area of the pupil, it narrows and becomes deformed. The extreme manifestation of this process is complete occlusion of the pupil and a high risk of vision loss due to the development of obscuration amblyopia.
The causes of iridocyclitis are diverse and can be endogenous or exogenous. Often, iridocyclitis develops as a result of traumatic injury to the eye (wound, contusion, ophthalmic surgery), inflammation of the iris (keratitis). Iridocyclitis can be caused by previous viral, bacterial or protozoal diseases (influenza, measles, HSV, staphylococcal and streptococcal infections, tuberculosis, gonorrhea, chlamydia, toxoplasmosis, malaria, etc.), as well as existing foci of chronic infection in the nasopharynx and oral cavity (sinusitis, tonsillitis).
The cause of iridocyclitis can be rheumatoid conditions (rheumatism, Still's disease, autoimmune thyroiditis, ankylosing spondylitis, Reiter's and Sjögren's syndromes), metabolic disorders (gout, diabetes), systemic diseases of unknown etiology (sarcoidosis, Behçet's disease, Vogt-Koyanagi-Harada syndrome). The prevalence of iridocyclitis among patients with rheumatic and infectious diseases is about 40% of cases.
The occurrence of iridocyclitis is facilitated by the developed vascular network of the eye and the increased susceptibility of the iris and ciliary body to antigens and CECs coming from extraocular foci of infection or non-infectious sources of sensitization.
With the development of iridocyclitis, in addition to direct damage to the choroid by microbes or their toxins, immunological damage occurs with the participation of inflammatory mediators. Inflammation is accompanied by phenomena of immune cytolysis, vasculopathies, dysfermentosis, microcirculation disorders with subsequent scarring and dystrophy.
Of no small importance in the development of iridocyclitis are provoking factors - endocrine and immune disorders, stressful situations, hypothermia, excessive physical activity.
Fuchs' heterochromic iridocyclitis is usually (but not always) a unilateral, chronic, recurrent, practically asymptomatic anterior uveitis in young patients, often complicated by the development of cataracts and glaucoma (75 and 15%, respectively).
The pathogenetic basis of Fuchs' iridocyclitis is an immune reaction involving CD8+ T cells caused by chronic infection with the rubella virus.
The most common complaint is a progressive change in the color of the iris, which occurs in 70% of patients. The initially dark iris becomes lighter due to stromal atrophy. Blue eyes, on the contrary, darken due to the pigment epithelium beginning to shine through the atrophied stroma.
Heterochromia is absent in 6% of patients with bilateral lesions, and then atrophy of the iris stroma acquires special diagnostic value. Other complaints include a slight decrease in visual acuity, floaters, and discomfort in the eye. Pain and pericorneal injection are rare with this pathology. A characteristic, but not obligatory, finding is multiple small, stellate precipitates on the endothelium of the lower third of the cornea, forming the triangle of Arlt. During gonioscopy, newly formed vessels are visualized.
Laboratory diagnostics consists of determining antibodies to the rubella virus in chamber fluid (specificity 100%), oligocponal IgG (sensitivity 87%), as well as the modified Goldmann-Witmer index (antibody level index to the rubella virus antigen exceeding 40, in combination with characteristic symptoms is very informative).
Differential diagnosis should be carried out with other causes of acute anterior uveitis (HSV, herpes zoster virus, toxoplasmosis, Kraup-Posner-Schlossmann glaucomocyclic crisis) and heterochromia.
Local use of glucocorticoids with minimal inflammation, characteristic of Fuchs iridocyclitis, has no obvious indications, since with a slight effect on the underlying autoimmune process, hormonal therapy accelerates the appearance of cataracts and glaucoma. In this regard, careful dynamic monitoring of patients, aggressive therapy (and often surgery) for secondary glaucoma, and also, if indicated, phacoemulsification with perioperative local and systemic hormonal therapy and vitrectomy, seem more justified. The prognosis for vision is favorable even in cases of long-term inflammation.
! Despite the fact that many of the diseases described in this section are considered incurable, the Center for the Treatment of Rare Diseases in Milan is constantly looking for new methods. Thanks to gene therapy, it has been possible to achieve outstanding results and completely cure some rare syndromes.
Contact a consultant on the website or leave a request - this way you can find out what methods Italian doctors offer. Perhaps this disease has already been treated in Milan.
+7 (925) 50 254 50 – urgent treatment in Italy
REQUEST TO THE CLINIC
Photos of the iris in Fuchs syndrome
In this case, hypochromia occurs more often and only in 10% of cases does hyperchromia of the iris develop. Quite rarely, hyperchromia is a congenital feature. The heterochromic iris develops as a result of stromal atrophy and impaired pigmentation of the posterior endothelial layer, but it is also determined by the genetically determined color of the iris. With severe stromal atrophy, the posterior pigment located on the endothelium becomes translucent, which leads to the development of hyperchromic coloring. Usually the brown iris becomes lighter, and the blue one, on the contrary, becomes more saturated.
Diagnostics
Ophthalmologists make the diagnosis by examining the eye with a slit lamp. Ultrasound pachymetry is used to assess the thickness of the cornea and the severity of its edema. During endothelial microscopy, the clarity of the image of the endothelium, the density of cells per unit area and their average size are determined.
Optical coherence tomography is also used - OCT (OTC, eng.) - a method that allows you to obtain detailed information about all layers of the cornea.
Complications
Uveitis developing against the background of Fuchs syndrome is prone to a chronic course. In this case, complications often arise (cataracts, glaucoma), which are associated with the irrational use of local preparations of corticosteroid hormones.
1. Cataracts often complicate the course of the disease and have no distinctive signs from cataracts with anterior uveitis of a different nature. The effectiveness of surgery and implantation of posterior chamber lenses is quite high. However, the development of hyphema is possible. 2. Glaucoma can cause vision loss and usually accompanies a long-term condition.
Prevention measures and prognosis
It is necessary to carry out differential diagnosis with other pathologies of the organ of vision. These include cataracts, glaucoma, retinal and optic nerve dystrophy. For prevention, it is important to consume sufficient amounts of nutrients contained in plant and animal foods. To maintain the required concentration of biologically active molecules during spring vitamin deficiency, multivitamin complexes are recommended for use. A person should engage in regular moderate exercise and lead a healthy lifestyle.
Treatment of uveitis in Fuchs syndrome
Treatment of uveitis that develops with Fuchs syndrome includes:
1. Injections of long-acting drugs (triamcinolone acetate) into the posterior sub-Tenon's space help with vitreous opacities. 2. The use of topical steroids is ineffective. 3. Due to the fact that posterior synechiae are formed extremely rarely, mydriatics, as a rule, are not prescribed. 4. Vitrectomy is performed when there is significant opacification of the vitreous body, which is not amenable to treatment with steroid drugs.
What is subatrophy? Causes
The death of the eye, which occurs very slowly, and during which the eyeball shrinks, shrinks, and then dries out, is called subatrophy. Unfortunately, this disease, unlike a number of others, cannot be cured, and it leads to
complete loss of vision.
Ophthalmologists identify several reasons for its appearance, the most common of which are:
- post-traumatic period;
- protracted inflammatory process.
Unfortunately, subatrophic eyes must be removed, since they not only entail a regular inflammatory process, but also sympathetic ophthalmia. What it is? The last medical term is the damage to a healthy eye by the immune system: inflammation from the diseased eye passes to an eye untouched by the disease. That is why the elimination of subatrophy is a task of paramount importance, which should not be delayed under any circumstances.