Causes
There are the following reasons why eye redness may occur:
- exposure to negative environmental factors (wind, snowstorm, frequent exposure to dry air);
- eye strain during long-term work or study, especially if you have to sit in front of a computer for many hours;
- exposure to chemicals, toxins, foreign bodies;
- the use of an optical product that was not prescribed by the doctor, but was chosen by the patient himself, so it is not suitable for him and overstrains the eyes;
- infectious and viral diseases in the body, spreading to the organs of vision;
- cardiovascular pathologies, for example, with hypertension, the eyes become red almost all the time;
- liver disease.
Many of these pathologies and conditions must be treated in a timely manner to prevent many complications.
Causes of hyperemia
For your information! One of the common causes of hyperemia is failure to comply with personal hygiene rules (for example, using someone else's towel, rubbing the eyes with dirty hands, improper care of lenses, etc.).
Other reasons experts include:
- Uveitis (inflammation of the choroid of the eyeball).
- Scleritis (acute inflammation of the deep layers of the sclera - the white membrane of the eye).
- Barley (purulent inflammation of the hair follicle of the eyelash).
- Iridocyclitis (inflammation of the iris and ciliary body).
- Purulent inflammation of soft tissues as a result of infections in the mucous membrane of the eye .
- Acute glaucoma (sudden increase in intraocular pressure).
- Mechanical damage and trauma to the conjunctiva.
- Allergic reaction to cosmetics, household chemicals, pollen, etc.
- Blepharitis (inflammation of the edges of the eyelids).
- Chalazion (chronic inflammation of the eyelid margin).
- Stress and chronic fatigue.
- Radioactive radiation.
- Constant lack of sleep.
- Increased visual load (especially when working at a computer).
Know! In addition to infectious and inflammatory eye diseases, the cause of hyperemia can be cardiovascular pathologies, diabetes mellitus and other endocrine disorders, cerebral vascular diseases, etc.
Risk group
The risk groups for acute or chronic eye redness include the following categories of patients:
- suffering from systemic diseases, for example, hepatitis, diabetes, hypertension;
- people whose work involves the use of chemicals and harmful substances;
- people who, on duty, spend a long time on the street, even despite bad weather conditions (road workers, traffic police officers);
- patients who sit in front of a computer for long periods of time, use phones, TVs, tablets and other electronic devices, and read books in poor lighting.
If a patient is at risk, he needs to have his vision examined by an ophthalmologist annually to prevent many diseases.
Types of inflammatory process
Conjunctivitis can be acute or chronic. An acute process is characterized by an acute onset. First, the inflammation affects one eye, and over time the second is also involved in the process. The discharge is mucous or even purulent in nature. They stick the eyelids together so tightly that after waking up it is difficult for a person to open his eyes. The conjunctiva is red, swollen and cloudy.
The chronic form lasts quite a long time. Patients complain of eye fatigue, heaviness of the eyelids, and itching. Conjunctival hyperemia is mild. Discharge from the eyes is scanty and mucopurulent in nature.
It is very easy to get an infection in the eye. Don't rub your eyes with dirty hands
Acute conjunctivitis, in turn, is divided into the following forms:
- adenoviral. It is characterized by the formation of pinpoint vesicles, enlargement of the submandibular and parotid lymph nodes, as well as the appearance of infiltrates on the cornea, which spoil vision;
- gonorrheal This is a serious form of inflammation, in which the outer shell of the eye is sharply hyperemic, swollen and bleeding. The process can spread, even moving to the cornea. The appearance of ulcers on it is fraught with loss of the eye;
- chlamydial Characterized by the formation of granular follicles. Develops against the background of urogenital chlamydia;
- viral keratoconjunctivitis is more often diagnosed in childhood;
- allergic. Most often occurs during the flowering period. Household allergens are also often the cause of increased sensitivity. In addition to hyperemia of the mucous membrane, swelling of the eyelids and profuse lacrimation appear;
- dry. It mainly occurs in older people, as well as in those living in hot climates. When moving the eyeballs, a feeling of the presence of a foreign body appears.
If hyperemia of the mucous membrane of the eye is accompanied by swelling and pain, this may indicate the presence of the following diseases:
How to treat viral conjunctivitis
- allergic reaction. Allergens can include household chemicals, food, medications and much more;
- blepharitis - inflammation of the eyelids, in which they thicken;
- chalazion - growth and inflammation of the meibomian gland;
- barley;
- orbital phlegmon.
Symptoms of conjunctivitis depend on its form. Still, experts identify common symptoms:
- edema;
- discharge;
- itching and burning;
- lacrimation;
- pain;
- photophobia.
Depending on the underlying cause, conjunctival hyperemia may be accompanied by pain, a sensation of a foreign body in the eye
Depending on the degree of damage to the mucous membrane of the eye, experts distinguish three main forms of the disease:
- Conjunctival injection. The mucous membrane that covers the eyelids turns red. Hyperemia of the transitional fold and eyeball also occurs. The pathological condition is accompanied by photophobia, lacrimation, pain and burning in the eyes.
- Ciliary injection. Redness affects the iris of the eye. Deeper tissues are involved in the process. Most often, this form occurs with iridocyclitis and iritis. In this case, the mucous membrane has a purple tint, it is smooth, and there are no blood vessels protruding above it, as is observed with a conjunctival injection. This is because the inflammatory response is caused by the blood vessels inside the eye.
- The mixed form occurs during acute infectious processes, which are characterized by a hematogenous transmission route. The iris changes its color and a purulent infiltrate is observed.
Symptoms
If a person experiences redness of the eye, it may be accompanied by the following symptoms:
- acute or chronic pain syndrome;
- itching, burning, pain in the eyes, sensation of a foreign body;
- increased production of tear fluid or, conversely, excessive dryness of the eyes, which can cause damage to the cornea, on which small microcracks and injuries will form;
- if the cause of the condition is bacterial conjunctivitis, an additional purulent discharge will form, which sticks the eyelashes together in the morning and interferes with normal vision;
- a gradual decrease in visual acuity, which occurs in systemic pathologies accompanied by vascular disorders.
If red eyes are caused by a systemic disease, the patient may experience other symptoms that are associated with them. For example, with hypertension, the patient often has pain and dizziness, and his face turns red.
Conjunctival hyperemia: what is it?
Basically, this condition develops against the background of an inflammatory process on the mucous membrane of the organ of vision, or in the layer of blood vessels. The reason for this phenomenon is the impact of negative factors. Hyperemia was also observed against the background of eye injuries, diseases of the iris, and eyelids.
There are two forms of the pathological condition: acute, chronic. In the first option, redness occurs very quickly, first on one side, then on the other.
Sometimes hyperemia is accompanied by the separation of purulent contents, and a change in the shade of the eyeball and cartilage is recorded.
The chronic course of the pathology is often accompanied by severe itching, the feeling of a foreign object in the eyes, and constant tension in the organ of vision. The purulent discharge is not profuse, redness extends only to the upper part of the cartilage.
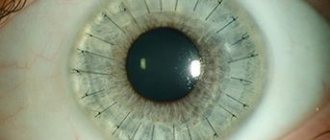
Photo
Diagnostics
To identify the causes of red eyes, your doctor will need to perform several diagnostic tests:
- Questioning the patient. The doctor identifies disturbing symptoms; people often complain of dryness and pain in the eyes.
- A general examination, during which the doctor may use a slit lamp to view details on the surface structures of the eye. When the organs of vision are red, purulent exudate may be released, increased or decreased production of tear fluid, damage to the mucous membrane, foreign objects and other formations.
- Fundus examination. This technique allows the doctor to evaluate all intraocular elements. The person is first instilled with Atropine or similar drugs that disrupt the process of pupil accommodation. Using a slit lamp, the doctor can evaluate the entire internal structure.
- Assessment of visual acuity using diagnostic tables. The more lines a person sees, the better the quality of his vision. The method is used to eliminate the possibility of decreased visual acuity in many diseases that cause redness of the mucous membrane.
- Measurement of intraocular pressure to eliminate the possibility of glaucoma formation.
- Bacterial culture to detect the infection and the antibiotic to which it is sensitive.
- PCR. This is a virological method with which the exact type of pathogen is determined.
- Ultrasound of the eyeball. Using directed ultrasonic waves, the position and condition of the intraocular elements and the eyeball itself are assessed.
- MRI, CT. Such testing is often performed when it is impossible to accurately identify the cause of the condition using other methods. On the screen, the doctor will see a layer-by-layer image of the visual organs, nerve fibers, and brain. Using the test, you can accurately determine the cause of redness.
Based on genetic tests, the doctor determines the exact cause of the disease, and only then can treatment begin.
Hyperemia of the conjunctiva of the eyes: diagnosis
The patient’s quick and complete recovery directly depends on high-quality diagnosis and prescribed treatment. The visual examination takes only a few minutes. The doctor uses special instruments to examine the condition of the mucous membrane of the eyes, and then, based on the results obtained and the patient’s complaints, makes a diagnosis. Depending on what caused the disease, additional laboratory tests and consultations with other specialists may be required: a therapist, an allergist, a surgeon.
Treatment
The method of treating the condition depends on the cause that caused the redness. Most often, complex therapy is used, aimed at eliminating all possible causes:
- reduction of time spent on the computer, telephone, TV and other gadgets;
- increasing the time spent on sleep, which should be at least 8 hours a day;
- lack of reading during therapy;
- replacing contact lenses with glasses so as not to further irritate the mucous membrane of the eyes;
- local antibiotics using drops and ointment, if the cause of the condition is a bacterial infection;
- systemic antiviral agents that eliminate the pathogen from the blood;
- removal of a foreign body from the eyes by an ophthalmologist if it is the cause of the condition;
- washing the eyes with saline solution or antiseptics;
- treatment of systemic disease.
After completing therapy, it is recommended to consult an ophthalmologist again so that he can examine your vision organs. This will prevent the risk of recurrence of redness.
Treatment of hyperemia
Treatment is selected depending on the cause (or pathogen) of the disease. Drops, ointments, topical antibiotics, etc. are used as therapy.
Thus, patients are prescribed the following types of medications :
- Drops and ointments with an antibacterial effect (Tobrex drops, Sulfacyl sodium drops, Tsipromed drops, Levomycetin ointment, Oftocipro ointment, etc.). They are used for the development of bacterial infections in the eye area.
- Antiviral drops and ointments (Ophthalmoferon drops, Actipol drops, Dexamethasone drops, Zovirax ointment, Acyclovir ointment, etc.). The drugs are indicated for viral etiology of the disease.
- Antihistamines (Allergodil drops, Claritin tablets, Cortisone tablets, etc.). They are recommended in case of an acute reaction to a particular allergen.
It is worth noting! It is recommended to instill drops into the conjunctival sac, slightly pulling the lower eyelid down. Ointments are placed there (in small quantities).
The products must be used 4-5 times a day. The course of treatment is determined individually.
In case of hyperemia, it is not recommended to make compresses or apply bandages to the eyes , as this can only aggravate the disease.
Complications
If the causes of redness are not eliminated in time and treatment is not started, the following adverse reactions may occur:
- the spread of a bacterial or viral infection into the lacrimal sac, conjunctiva, cornea and inside the eyeballs;
- spread of a bacterial or viral infection into the nasopharynx, which can cause sinusitis, rhinitis, tonsillitis;
- gradual decrease in visual acuity;
- inflammatory condition of the eyelids, cornea, eyelids, conjunctiva.
The formation of complications can be easily prevented with timely therapy.
Types of hyperemia
Depending on how deep the infection has penetrated, redness is divided into two types: ciliary and mixed. Ciliary hyperemia is diagnosed when the infection spreads deep into the eye. In this case, the vessels are not the standard red, but more blue in color. This condition indicates that deep-lying arteries are affected.
Mixed hyperemia is called hyperemia, in which infection occurs not only of the conjunctiva, but also of the ciliary body. In this case, the infection penetrates the organ of vision through the blood.
Prevention
To prevent the sudden formation of red eyes, it is recommended to adhere to the following rules:
- spend less time on electronic gadgets, read in moderation;
- spend more time in open space, where the eyes do not need to get used to nearby objects;
- take vitamins, harden yourself to support the immune system;
- Visit an ophthalmologist annually to prevent the development of many serious diseases.
Preventative measures will not completely eliminate the risk of redness, but they will significantly slow it down.