In some diseases, the unique ability of the visual organ to perceive light radiation is affected. Gonioscopy, as the most important method of instrumental research, will help diagnose the condition of the eyes. Most often, a painless procedure for examining the anterior space of the eyeball is prescribed for glaucoma.
What is gonioscopy?
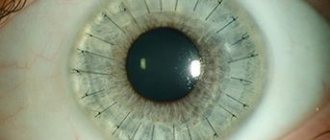
To treat various eye pathologies, the doctor needs information about the state of the eye chamber between the iris and cornea of the anterior part of the visual organ. For diagnostics in ophthalmology, a special device, a gonioscope, is used, equipped with a system of specifically installed mirrors. Thanks to the device, the doctor has the opportunity to view the structure of the visual apparatus, which is inaccessible by the usual method.
The essence of the technique
In addition to a device with mirrors, a slit lamp is used during the examination. The device is used as additional equipment. The device generates a beam of light that allows you to achieve the desired magnification to obtain the desired optical cut. Using a gonioscope, it is possible to achieve visualization of distant areas of the eye, an overview of the iris-corneal space of the eyeball, which is inaccessible for viewing during direct examination.
Gonioscopy is necessary to assess the functional abilities of the optical system of the organ of vision and its anterior chamber. Diagnostics is used to clarify the type of glaucoma, as well as to perform anti-glaucomatous manipulations in the space of the eye chamber.
About the structure of the eye
In ophthalmology, the chamber of the eye is a closed cavity filled with ocular fluid. The eyeball has an anterior and posterior chamber. The area between the cornea and the iris is called the anterior chamber, the area between the iris and the vitreous is called the posterior chamber. Both chambers participate in the circulation of ocular fluid and, in the absence of pathologies, have a constant volume. The formation of fluid involves the cilia of the ciliary body in the posterior chamber. The outflow of moisture occurs in the anterior region: where the cornea connects to the sclera and the iris passes into the ciliary body. This place is called the anterior chamber angle.
Types of gonioscopes used
The problem of physical examination of the state of the transition region from the cornea, bypassing the sclera and iris on the way to the vitreous body, lies in a special optical effect. The light falling during a routine examination reaches the iris at a certain angle, which interferes with the view of the front camera of the eye apparatus from a certain angle.
Thanks to the introduction of a gonioscope, light is blocked, allowing a detailed examination of the eye without optical interference. To diagnose pathological processes, several types of devices are used, differing in design and functionality.
The advantage of the Krasnov gonioscope
The GK-1 device is a single-mirror device consisting of a tetrahedral tube (prism) placed in a plexiglass housing.
- The front part of the device is made in such a way as to ensure a tight fit to the eyeball area. A prism is a contact lens that has a spherical shape.
- There is a gap in the center of the part in contact with the surface of the eye. A special incision hides the corneal portion of the prism, designed to contact the layer of the cornea.
Gonioscopy of the eye is performed during a smooth transition of the corneal part of the prism into the area of scleral curvature, allowing visualization of the angular region of the ocular chamber. The review is carried out through the plane of the base of the tetrahedron facing the diagnostician. As the procedure progresses, the doctor rotates the gonioscopic device to provide a view of the entire space of the corner zone.
The advantage of the Krasnov apparatus is that due to the small dimensions of the gonioscope, there is no need to use a solution for tight contact. The substance is filled into the space between the organ being examined and the tube of the device.
Features of the Goldmann gonioscope
The device, developed by a Swiss ophthalmologist, is made as a cylinder equipped with three mirror surfaces. Mirrors are installed at certain angles, which contributes to the refraction of light rays. The result is a clear view of the eye chamber along with the peripheral retina and ciliary body while rotating the mirror device.
A unique feature of the Goldmann gonioscope is the ability to perform not only a one-time camera diagnosis, but also conduct microgonioscopy using a slit lamp.
Van Beuningen gonioscope device
The optical part of the ophthalmological device is made in the shape of a tetrahedral pyramid, the sides of which are equipped with mirrors. The top of the pyramidal device is truncated, due to its spherical shape with a certain radius, it plays the role of the corneal part of the device. Placing the glass pyramid of the gonioscope in a glass case having a scleral shape makes it possible to view the ocular chamber without the need to rotate the pyramid.
Types
Ophthalmologists use the following gonioscopes:
- Single-mirror Krasnov (GK-1), which is a tube with 4 faces and a polymethyl methacrylate (organic glass) body. The main part is in contact with the cornea and is located in the center.
- Three-mirror Goldmann gonioscope in the shape of a cylinder. Mirrors are installed at different angles, which allows you to better inspect the UPC. It is actively used for selective laser trabeculoplasty SLT (a non-invasive procedure using a low-pulse laser for the treatment of glaucoma).
- Zeiss four-mirror goniolens for diagnostic purposes only. Prisms are used instead of mirrors.
- Direct Koerre (Keppe) lenses, when used, diagnostics are carried out in a horizontal position. No slit lamp required. Allows a panoramic view of the UPC.
- Direct gonioscopes from Swan-Jacob, which are suitable for surgical interventions. The lenses are held on the cornea using a special handle.
There are many modifications of the above lenses.
Indications for gonioscopy
The main reason for ordering an examination is the suspicion of glaucoma. Diagnostics are also prescribed during a routine examination of patients at risk for this disease. Glaucoma belongs to the category of progressive diseases that threaten irreversible blindness.
The disease is accompanied by an increase in intraocular pressure, which results in destruction of the retina against the background of optic nerve atrophy. The result is a cessation of visual signals entering the brain area, which impairs vision with limited visibility. Gonioscopy for glaucoma allows:
- identify or confirm suspicion of the presence of pathology and other types of diseases of the visual organ;
- check the health of the eyes before surgery, monitor the restoration of vision after it;
- Conduct preventive examinations to identify birth defects and anomalies.
During a gonioscopic examination throughout all stages of glaucoma treatment, the ophthalmologist is able to determine the form of the pathology (closed-angle or open-angle type). With the help of instrumental diagnostics, it is possible to identify the location of pathological changes and the extent of their spread throughout the anatomical structures of the eye. The results of gonioscopy for a specialist become a decisive argument in favor of choosing a method of treating glaucoma - medication or surgery.
Gonioscopy, as a technique for examining the eye, is also indicated for solving other problems related to the health of the visual organs:
- to identify foreign bodies in the eye when the organ is injured;
- for problems affecting the anterior chamber space (poor blood circulation);
- in case of suspected pigment dispersion associated with leaching of the pigment substance from the iris;
- with the development of inflammatory processes affecting the uveal tract;
- if there is a suspicion of a cystic or tumor process spreading to the cornea and iris.
Important! When diagnosing diabetes mellitus, gonioscopy is a mandatory procedure, since glaucoma often accompanies diabetes mellitus. Eye examination is necessary for timely treatment of eye pathology and prevention of malignant degeneration of the process.
Diagnostic process
The diagnosis itself consists of several stages.
Preparation
- Before starting work, the doctor prepares the device: adjusts the optics, checks the lighting, and treats the part in contact with the eye with a disinfectant mercury solution.
- The subject is positioned on a chair in front of the device, his chin should be on a stand, his head should be fixed to avoid involuntary movements.
- The patient is first instilled with drops with a local anesthetic effect: “Lidocaine” or its analogues. This is done to minimize discomfort for the patient, although in general gonioscopy is a painless procedure.
Inspection
In order to improve the quality of the examination, the ophthalmologist applies the gel to the part of the device that comes into contact with the eye. The doctor expands the eye space with his hands, instructing the patient to look alternately down and up, and at this time placing the scleral part of the gonioscope in the conjunctival area. Next, the parts of the anterior chamber of the eye are examined:
- corneas;
- root part of the iris;
- Schwalbe rings;
- areas of corneal trabeculae and Schlemm's canal;
- scleral spur;
- parts of the ciliary body;
- fibers of the pectineal ligaments.
The optometrist adjusts the position of the device with one hand and operates the slit lamp (light and microscope) with the other.
After removing the goniolens from the eye, the patient is given drops again to prevent the development of a bacterial infection.
From start to finish this procedure takes about fifteen minutes. If the doctor knows the research technique, then the patient can easily tolerate it, leaving no traces behind.
Description of the procedure
Regardless of the purpose for which the examination is prescribed according to the list of indications, the procedure requires simple preparatory measures.
| What the patient should know |
|
| What actions does the doctor perform? |
|
How to do it
- Since the examination uses a slit lamp, the patient must position himself opposite the lighting device, resting his chin on the surface of the special stand of the device.
- The subject's eye is treated with gel to improve contact with the gonioscope, and the head is fixed using a support device.
- The patient needs to slowly approach the device until the gonioscope eyepiece is in full contact with the vitreous body. You should look at the slit lamp.
- To ensure the correct position of the scleral segment, the person moves the eyes in different directions in accordance with the instructions of the ophthalmologist. The gonioscope is moved slowly to better visualize the anterior chamber.
- The final stage of gonioscopy is photographing important parts of the visual organ - the corneal surface, the iris of the eye, the tubules and the ciliary body itself.
The absence of pathologies is indicated by an open acute angle of the anterior chamber, which is completely accessible for inspection and freely allows moisture to pass through. Impaired fluid outflow suggests the development of cataracts. In order to prevent infection of the organ, after examining the eyes, antibacterial eye drops are instilled.
Algorithm for performing gonioscopy
The doctor or nurse is familiar with the description of gonioscopy to the patient before it is performed. When a person knows what awaits him, he behaves calmer and allows the doctor to carry out all the necessary manipulations without any difficulties. The procedure algorithm is as follows:
Congenital glaucoma in children
- No preparation is required before the event. If the patient uses contact lenses, then, of course, they should be removed. It is advisable not to use decorative eye cosmetics on this day.
- Immediately before the procedure, an anesthetic is applied to the surface of the eyeball being examined to reduce discomfort.
- Then gonioscopy gel is applied to ensure better contact of the device head with the surface of the cornea.
- Next, the patient sits in front of the device and a bright lamp. The device is brought to the eye so that the eye comes into contact with the head of the gonioscope. The patient's head is fixed using a special auxiliary element.
- Then the subject moves his head closer to the gonioscope until the lens of the attachment and the vitreous body come into full contact. The lens of the device presses on the eyeball; under pressure, its anterior chamber opens slightly, which gives access to the study of all structures of the eye that are of interest to the doctor.
- Now you can begin the actual inspection. As directed by the doctor, the patient will have to roll his eyes, raise them up, down, or look to the side.
- During the procedure, the ophthalmologist will take several photos to document the condition of the iris, cornea, ciliary tubules and ciliary body. After completing all the necessary steps, the device is removed.
The doctor will inject an antiseptic solution into the conjunctival sac of the examined eye to prevent infection or spread of an already developing infection. Minor discomfort after the procedure goes away on its own after a few minutes.
Gonioscopy for glaucoma
The interpretation of the data obtained during the examination depends on the qualifications of the diagnostician. The specialist classifies the condition of the organ of vision according to the location of the iris, which opens or closes the view of the examination area.
| Angle shape | Characteristics of the result |
| Closed | The iris completely covers the entire examination area. The situation indicates a severe form of glaucoma, the development of a tumor process |
| Medium Width | The ciliary body of the visual organ is almost completely hidden under the cover of the iris. The examination result can be considered a suspicion of congenital glaucoma |
| Narrow | The result is typical for patients with glaucoma with farsightedness. The diagnosis requires clarification |
| Open | The iris allows you to clearly visualize the study area, which may indicate congenital pathologies, severe injury to the lens, myopathy |
Types of procedure
Based on the purpose of the examination, different types of lenses are used for its implementation, fixed on the device and allowing to obtain a twenty-fold magnification.
Direct type of gonioscopy
To conduct an eye examination, a Koeppe lens is used, the sufficient curvature of which protects against complete reflection of light. The procedure is carried out with the connection of magnifying equipment - a microscope and an additional light source. To perform an extended examination of the eye chamber and a panoramic examination of the eyeball, the patient will have to lie on his back.
- Advantages. The technique allows you to examine different quadrants of the organ and compare the condition of different sectors of both eyes. Used to clarify the nature of congenital and acquired angle pathologies.
- Flaws. Lack of maximum accuracy due to the inability to fix the head of a lying patient. An ophthalmic lamp should not be used to closely examine tissue.
Features of indirect gonioscopy
The angle is visualized using a lens equipped with mirrors (one or more). The technique allows you to expand the area of examination of the organ of vision together with the assessment of the image in a mirror installed opposite through a slit lamp. The use of two lenses improves the visualization of all quadrants of the eyeball, and when connecting a system of four optical devices (lenses), there is no need to rotate the gonioscope during the examination.
The advantage of the technique is the use of Zeiss optics. Thanks to the small size of the prism-shaped lenses, they do not create problems when viewing. There is also no need to apply a lubricating gel, which is essential when preparing for a direct type procedure.
What is a gonioscope?
The ophthalmological device used for gonioscopy is called a goniolens or gonioscope. There are three types of this device, which determine the procedure:
| Gonioscope type | Features of the device and research methods |
| Kappe gonioscope (straight) | It is a transparent lens onto which medical gel is applied and applied directly to the cornea. Due to the fact that the outer surface of the lens has a certain curvature, it allows you to view the angle of the anterior chamber. The technique requires the patient to lie down and does not allow the use of a slit lamp. |
| Goldmann gonioscope (indirect) | The lens has the shape of a truncated cone and has two mirrors that allow light rays to be reflected from the anterior chamber towards the person performing the examination. The technique allows the use of a slit lamp and involves the use of a lubricating fluid that fills the space between the cornea and the surface of the lens. The patient is in a sitting position. |
| Zeiss goniolens (indirect/indirect) | The technique is based on the same principle as described above (Goldman), however, instead of mirrors in the lens, 4 prisms are used, which provide an overview of the angle of the anterior ocular chamber in 4 quadrants of the eye. Application with a slit lamp allows one to achieve excellent results, and the absence of the need to use a lubricating fluid and replacing it with a film of the patient’s tear fluid allows for a more in-depth diagnosis, allowing one to determine the nature of the adhesions of the iris and cornea, iris and lens. |
Contraindications to gonioscopy
- With inflammatory and purulent processes in the cavity of the visual organ.
- For severe eyeball injuries requiring emergency surgery.
- In case of mental disorders of the subject with demonstration of aggression.
- For drug or alcohol syndrome, allergies to drops (eye).
Comment. The presence of edema caused by exacerbation of glaucoma is not considered an obstacle to performing gonioscopic diagnosis. Swelling can be relieved with a few drops of a solution of glycerin in water or glucose, but the solution must be sterile.
In 1918, ophthalmologist A. Trantas proved the dependence of the progress of glaucoma on the processes occurring in the anterior chamber, and also used gonioscopy to diagnose eye diseases.
On the eve of 1925, thanks to M. Uribe-Troncoso, new models of electroophthalmoscopes appeared that visualized the anterior chamber. The device was first called a gonioscope.
Since 1938, ophthalmologists began to use a mirror gonioscope developed by G. Goldman. During the examination, a slit lamp was connected, and the examination was performed while sitting. Gonioscopy, prescribed to patients of any age, does not cause pain, lasts about 15 minutes, but is especially relevant for diagnosing glaucoma.
Sources used:
- Therapeutic exercises for the eyes / Biresford Stephen M. - M.: Potpourri, 2014.
- 100% vision / Mitchell H. Friedlander, Steph Donev. - M.: World of Books, 2005.
- Vision. Prevention and recovery. Methodological manual / T.M. Danilova. - M.: SPD Lyko B.B., 2005.
- “Eye Microsurgery” named after Academician S.N. Fedorov" of the Ministry of Health of the Russian Federation
Gonioscopy
- home
- Gonioscopy
Gonioscopy is a study of the angle of the anterior chamber of the eye using a gonioscope and a slit lamp. The angle region includes the marginal part of the anterior chamber, enclosed between the root of the iris and the limbus area. The essence of the method: a slit lamp provides focused illumination, the necessary magnification and optical section, the gonioscope mirror allows you to examine the angle of the anterior chamber of the eye being examined. The most widely used gonioscopes in our country are Krasnov and Boeningen. The Krasnov goioscope consists of an inclined glass tetrahedral prism enclosed in a plexiglass case. The front part of the gonioscope is in contact with the surface of the eyeball and matches it in shape; it is made in the form of a spherical contact lens. In the center of the scleral part of the gonioscope there is a hole in which the corneal part of the prism is placed. It is designed for contact with the cornea, and therefore has a spherical depression with a diameter of 10.5 mm and a radius of curvature of 8.5 mm. The image of the anterior chamber angle is seen through the base of the prism facing the observer. To examine the entire angle of the anterior chamber, the device must be rotated around its longitudinal axis. The gonioscope is small in size; during the study there is no need to use a contact solution to fill the space between the device and the eyeball. The Beuningen gonioscope is a four-sided glass pyramid with mirror surfaces and a truncated apex that contacts the cornea. The top of the gonioscope has the shape of a spherical surface with a radius of curvature of 8 mm. The glass pyramid of the gonioscope is enclosed in a translucent frame shaped like a scleral surface. When working with a pyramidal gonioscope, it is possible to examine all sides of the anterior chamber angle without rotating the pyramid around its axis. The Goldmann three-mirror gonioscope is a cylinder in which there are 3 mirrors located at different angles to the axis of the eye. This allows simultaneous examination of the anterior chamber angle, ciliary body and peripheral parts of the retina. Research methodology. Before the examination, the corneal and scleral parts of the gonioscope are disinfected by wiping with a damp swab soaked in a solution of mercuric oxycyanide (1: 6000). The gonioscope must not be wiped with alcohol, ether or boiled. After triple instillation of a 0.5% dicaine solution, the subject is seated in front of a slit lamp and the head is fixed on a stand. Having opened the palpebral fissure of the eye being examined and forcing the patient to look down and then up, the scleral part of the gonioscope is inserted into the conjunctival cavity. During the examination, the gonioscope body is held with the thumb and forefinger of the left hand, and the illuminator and slit lamp microscope are controlled with the right hand. To examine the upper and lower parts of the anterior chamber angle, the illuminator is placed to the right of the observer at an angle of 15-30°. When examining the lateral sections of the corner, the illuminator is installed on the side opposite to the mirror image of the corner, at an angle of 5-10°. The study of the anterior chamber angle usually begins with an examination of its lower parts, since in this area the angle is wider and more easily accessible to gonioscopic examination. As different parts of the angle are examined, the illuminator and microscope are moved depending on the position of the mirror surface of the gonioscope. The angle of the anterior chamber is clearly visible only if the capillary space between the cornea and the surface of the gonioscope is filled with tear fluid. An approximate inspection of the anterior chamber coal is usually carried out in diffuse light. To do this, use the gonioscopic attachment included in the slit lamp kit (ShchL-56). This attachment, placed on the head prism of the illuminator, produces a uniformly illuminated circle with a diameter of up to 20 mm. When conducting a study in diffuse light, the illumination slit should be wide open. For the purpose of more detailed gonioscopy and to obtain an idea of the shape of the angle, the study is carried out in direct focal light using a lighting slit. In this case, an optical cut of the corner is cut out. To obtain an optical section of the lateral sections of the corner, a horizontal slit is used. Most often, gonioscopy is performed using 18-20x magnification. After the examination is completed, the gonioscope is removed from the conjunctival sac, while the patient should look up, and the doctor pulls the lower eyelid down. The corneal-scleral part of the gonioscope is thoroughly wiped with a cotton swab soaked in a solution of mercuric oxycyanide and dried with a gauze cloth. After the examination, 2 drops of a 30% sodium sulfacyl solution are installed into the patient’s conjunctival sac. The anterior chamber angle is characterized by the following identification zones. 1. The cornea has the appearance of a transparent dome, hanging over the remaining zones of the angle. 2. The anterior limiting ring of Schwalbe is an elevation on the inner surface of the cornea with a rather steep slope descending towards the angle. This circular ring is the site of the end of Descemet's membrane and corresponds to the limbus region; it differs from the corneal tissue in its whiter color and less transparency. 3. Notch - a narrow groove that is the boundary between the anterior limiting ring of Schwalbe and the next zone of corneoscleral trabeculae. 4. The zone of corneo-scleral trabeculae and Schlemm's canal has the appearance of a pale gray, rather wide stripe. Almost in the middle of the trabecular zone, behind the translucent layer of trabeculae, the contours of Schlemm's canal are visible. Normally, Schlemm's canal does not contain blood. However, when the gonioscope presses too hard on the eye, as well as in some diseases, blood appears in Schlemm's canal. In these cases, Schlemm's canal looks like a bright red stripe that stands out against the pale background of the surrounding tissue. In old age and with certain diseases, increased pigmentation of Schlemm's canal is observed. 5. The scleral spur, or posterior limiting ring of Schwalbe, looks like a strip of bright white color. It is the site of attachment to the sclera of the ciliary body and limits Schlemm’s canal posteriorly. 6. The anterior surface of the ciliary body, protruding into the area of the angle of the anterior chamber, has a grayish-brown color and a slightly wavy surface. With age, this area becomes discolored and acquires a matte gray hue. 7. The root of the iris is a continuation of the anterior part of the ciliary body; it has different colors and relief. The root is delimited from the rest of the iris by one of the most peripheral contraction grooves. Sometimes the identifying zones of the anterior chamber angle can be partially covered by the pectineal ligament. The fibers of the ligament are thin bridges starting from the root of the iris and ending in the area of the corneoscleral trabeculae. The fibers of the pectineal ligament have the color of the iris. It is necessary to distinguish the pectineal ligament, which is a normal formation for the angle, from goniosynechiae. When conducting a gonioscopic examination, the shape of the anterior chamber angle and the presence of pathological changes in this area are determined. The shape of the angle is determined by the degree to which the iris covers the identification zones of the angle and by the distance of the root of the iris from the notch. The angle of the anterior chamber may vary in width and profile. At a wide angle, all of the listed structures are visible. A medium-width angle is characterized by the fact that all structures are visible except the anterior part of the ciliary body and the scleral spur. With a narrow angle, most of the trabecular zone is covered by the root of the iris, part of the angle is accessible to observation. In the case of a closed angle, the root of the iris reaches the level of the scleral spur. The angle profile corresponds to the degree of divergence between the posterior surface of the cornea and the plane of the iris. There are “coracoid” and “obtuse” angles. The angle of divergence can be calculated mathematically or measured (goniometry). A closed angle is always a pathology: it is observed during an acute attack of glaucoma, in cases of blockage of the angle zones by an iris tumor, etc. Changes in the anterior chamber angle associated with inflammation include goniosynechia. There is fusion of the iris root with the ciliary body stripe, scleral spur, trabecular zone, anterior limiting ring of Schwalbe, and cornea. Depending on this, goniosynechia is distinguished as ciliary, trabecular, and corneal. Goniosynechiae are observed in primary and secondary glaucoma, iridocyclitis. Degenerative-trophic changes in the angle of the anterior chamber are expressed in sclerosis and compaction of trabecular tissue, as well as in exogenous pigmentation of corneoscleral trabeculae and Schlemm's canal. These changes occur especially often with glaucoma. The main indications for gonioscopic examination are glaucoma, tumors in the root of the iris, foreign bodies in the angle of the anterior chamber. Gonioscopy is performed for the purpose of diagnosing glaucoma, differential diagnosis between primary and secondary glaucoma, and choosing a method of drug and surgical treatment. After antiglaucomatous operations, gonioscopy gives an idea of the state of the artificially created pathways for the outflow of aqueous humor, which is especially important if surgical treatment is ineffective. For iris tumors spreading in the area of the anterior chamber angle, gonioscopy makes it possible to determine the boundaries of the tumor and decide on surgical tactics. If there is a foreign body in the area of the anterior chamber angle, determining its size, shape and position, as well as its relationship with surrounding tissues are important in choosing the surgical method. Microcycloscopy is a method of intravital examination of the ciliary body using a gonioscope and a slit lamp. It is carried out by changing the position of the reflecting mirrors of the gonioscope or using gonioscopes with different angles of inclination of the mirrors. There are anterior and posterior microcycloscopy. During anterior microcycloscopy, the process part of the ciliary body is examined, and during posterior microcycloscopy, its flat part, the dentate line and the peripheral parts of the retina and choroid are examined using a Goldmann gonioscope. The method is of great practical importance in the diagnosis of foreign bodies and neoplasms of the ciliary body, peripheral retinal breaks, inflammatory and dystrophic changes in the peripheral parts of the retina and choroid. Swelling of the corneal epithelium, which is usually present during an acute attack of glaucoma, is not a contraindication to gonioscopy. After installation of a 40% solution of glucose or glycerin, diluted half with water, into the conjunctival sac, the swelling of the corneal epithelium is significantly reduced, which allows gonioscopy. Gonioscopic examination is not performed for acute conjunctivitis, dacryocystitis, keratitis and corneal ulcers.
When conducting this study, the patient's head is on the slit lamp stand, the chin and forehead are fixed, and the doctor, having previously applied a special gel to the contact surface of the gonioscope and opening the palpebral fissure of the patient's eye with one hand, places the contact surface of the gonioscope on the cornea of this eye with his free hand. The doctor holds the gonioscope with one hand, and with the other, using the slit lamp handle, moves the light slit along the edge of the gonioscope. The mirror surface of the gonioscope allows you to direct a beam of light into the corner of the anterior chamber of the eye and obtain a reflected image. In clinical practice, the gonioscopes most often used are Goldmann (three-mirror cone-shaped), Van Bouningen (four-mirror pyramidal) and M. M. Krasnov (single-mirror) (Fig. 6.15). The gonioscope allows you to examine the structural features of the anterior chamber angle: the root of the iris, the anterior strip of the ciliary body, the scleral spur to which the ciliary body is attached, the corneoscleral trabecula, the scleral venous sinus (Schlemm’s canal), the internal border ring of the cornea. It is especially important to determine the degree of openness of the anterior chamber angle. According to the super front chamber, it can be wide, medium width, narrow or closed. At a wide angle, all its constituent elements are clearly visible, including the ciliary body strip and corneoscleral trabeculae. With an anterior chamber angle of average width, the ciliary body is not visible or is defined as a narrow strip. If the angle of the anterior chamber is narrow, neither the ciliary body nor the posterior part of the corneoscleral trabeculae can be seen. When the anterior chamber angle is closed, the corneoscleral trabeculae are not visible at all, and the iris root is adjacent to the anterior limiting ring of Schwalbe. Gonioscopy allows you to detect various pathological changes in the angle of the anterior chamber: goniosynechia, newly formed vessels, tumors, foreign bodies. Our company offers consumers: - Van Beuningen 4-mirror gonioscope - 3-mirror Goldmann lens.