Raise your head and look at something evenly colored, at some light background (snow, sky without sun). If something like this suddenly began to slowly float before your eyes:
... So meet me, these are “dead pixels” in your eye
, formed by the vitreous body (in the picture below it is in all its glory). For many, such “glitches” appear in childhood and multiply or gradually change over the years. For most people, their presence is not a cause for concern, but their sudden appearance or sharp increase is a reason for an urgent visit to an ophthalmologist. Especially if this is accompanied by lightning before the eyes, a dark veil or fine “tobacco dust”.
But to understand the full situation, let’s talk about what this phenomenon is in general and where it comes from.
Where is the vitreous body?
The eye is a ball, most of which is occupied by the vitreous body (as much as 2/3 of the volume).
It is clearly visible in the diagram above - this is the space between the lens and the retina in the eye cavity. In a normal eye, the vitreous humor is so transparent that when the eye is scanned, it appears empty. The vitreous body is a jelly-like, viscous and well-stretchable liquid, like jelly or jelly. Only transparent. This “jelly” consists of water, colloids and microelements - collagen fibers, reminiscent of intertwined ropes, soaked in hyaluronic acid. Unlike the cornea, which consists of the same matrix, the density of the filaments in the vitreous body is lower, so the cornea is dense and rigid (by the standards of what is in the eye), but here a viscous medium awaits us.
This environment is heterogeneous; there are voids and “cisterns”, various lacunae. You can inject a special solution into the eye, which will color the vitreous body, and all this beauty will be visible. For example:
The vitreous body is adjacent to the posterior surface of the lens; throughout the rest of its length it is in contact with the internal limiting membrane of the retina. A special hyaloid canal passes from the optic disc to the lens through the vitreous body, and the frame of the vitreous body is formed by a thin network of intertwined fibers of various forms of collagen protein. And the gaps are filled with liquid - this structure gives it the appearance of a gelatinous mass.
Thanks to the vitreous body, our eyes have the correct spherical shape, it provides incompressibility and ocular tone, absorbs shocks, and nutrients move through the channels. But its light refractive function is very small.
If we need to deliver a medicinal substance to the deep parts of the eye, then we inject it directly into the vitreous cavity with a microneedle, because the eye is such an organ quite isolated from the body as a whole, and not everything that enters the blood reaches the internal contents of the eye . The blood-ophthalmic barrier interferes.
It happens like this:
Why do “floaters” appear before my eyes?
Most people, when some unusual phenomenon occurs, if it does not cause discomfort, simply do not pay any attention to it. Meanwhile, the disease, the symptom of which is various visions, progresses and turns into more severe forms that are difficult to treat.
Black spots before the eyes - what are they? This is a visual effect associated in most cases with destruction of the organ of vision. The cavity of the eye between the inner membrane and the lens is filled with a transparent avascular gel-like substance, which is normally completely transparent. The substance consists of viscous non-sulfonated glycosaminoglycan, ascorbic acid, salts, enclosed in a framework of thin fibrillar proteins.
When the vitreous fluid liquefies, its fibers stick together and resemble “spiders”, “chromosomes”, “caterpillars”, “flies” in appearance. In addition to various images, “lightning” and “flashes” can be observed. They arise due to an abnormal reaction of the optic nerve to “optical voids” that arise when the vitreous body loses its homogeneity and divides it into thick and liquid fractions.
Where do glass worms come from?
For the most part, translucent “ghosts” that appear in the field of vision during, for example, a sharp fall or a parachute jump, lifting weights, or against the background of complete well-being and subsequently discernible when carefully examining light-colored objects are natural lacunae in the vitreous, caused by its design.
They sometimes close on their own, move, or form new ones on their own (slowly, over months). In general, any noticeable “worms” are something in the vitreous that prevents light from reaching the retina normally. In English-language literature, they are called “floaters” - like specks of dust on a camera matrix. This condition is called “vitreous destruction” (VD).
The presence of small single fragments in the vitreous cavity is normal from a medical point of view.
There is often a different story. But now we need to go a little deeper into the anatomy. The vitreous body itself is not attached to the retina along the main area, but is simply adjacent very closely. However, in the macula (the center of the eye, the macula), near the optic nerve and along the equator of the retina there are attachments, and quite strong ones. If, with age, in the event of an injury or the appearance of another disease of the eye and the body as a whole, not just destruction (generally not dangerous), but some blood cells and inflammation appear, this is a very dangerous problem. Everything that gets into such a closed cavity is absorbed for a long time, difficultly and not always completely with a transparent effect. As a rule, stained opacities, rough adhesions and cords remain, reducing visual acuity. Everything is explained by close, I would even say, intimate contact with such an important tissue as the retina (the retina and vitreous body suffer simultaneously in case of illness).
This is a terrible picture that can be seen with hemorrhage into the vitreous body (this is called hemophthalmos).
And if droplets of cholesterol accumulate in the vitreous body, it looks like “golden rain”.
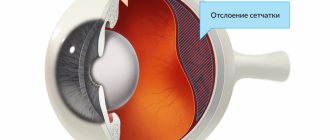
With a blunt blow to the eye, the vitreous body will take on the main deformation as a result of mechanical trauma and begin to change shape. Where it was simply adjacent to the retina, it will boldly move away and return back. But where there were adhesions, the vitreous body, when deformed, will pull the retina with it into the eye. This can result in a much more serious injury - a rupture or detachment of the retina. And this is all the chances of losing vision or deteriorating the optical quality of the eye to a few percent of normal.
Laser-demarcated retinal tear
Causes of flies flashing before the eyes: diabetes, poisoning, anemia
Diabetes. An increased level of glucose in the body indicates damage to the retinal vessels and the development of diabetic retinopathy. The strength of blood vessels decreases. Impaired cholesterol metabolism leads to the formation of tyrosine crystals. Eye movements contribute to pendulum-like oscillations of the crystals, as a result they shimmer, sparkle, and the patient sees gold and silver showers before his eyes.
Poisoning. Exposure to toxic substances on the nervous system leads to damage to the optic nerve. The result is flashing white flies, double vision, bright flashes and lightning. Poisons such as botulinum toxin and wood alcohol are especially dangerous for the optic nerve.
Anemia. A low level of hemoglobin leads to oxygen starvation (hypoxia), disruption of metabolic processes in the retina and, as a consequence, the appearance of the floater effect.
What happens with myopia?
In myopic people, as a rule, the axial length of the eye is more than 24 mm (the average statistical parameter, the measurement of which tells us about the progression of myopia). The eye goes from being shaped like a soccer ball to being a rugby ball. In this case, the posterior pole of the eye stretches, but if this is not dangerous for the outer sclera (it is quite elastic), then the middle (choroid) and inner sclera (retina) do not stretch. Therefore, in the posterior pole, the nutrition of the retina deteriorates, and dystrophic zones of stretching and ruptures appear along the periphery. The vitreous body plays a big role in this. At the attachment points, it pulls on the retina and holes are formed.
What happens as you age?
Somewhere after 30 years, new “midges” often begin to appear, and after 40 years, hyaluronic acid is gradually lost, the transparency of the vitreous body decreases, and visualization of fibers appears.
Even later, the vitreous body dries out altogether and begins to peel off from the retina (it simply comes off in places where there is no attachment).
Vitreous detachment is a normal sign of aging.
it is caused by liquefaction of the vitreous body, leading to tension in the retina in places of strong attachment, which can lead to retinal rupture. Acute vitreous detachment leads to retinal tears in 15% of cases.
Figuratively speaking, a kind of “snot” of gel (this is a very imprecise description of this type of tissue, but gives a very good understanding) hangs out inside the eye. Then this “clump of gel” comes off the optic nerve. As a rule, the separation zone looks like a ring (Weiss ring), that is, when projected onto the retina, the result is what patients call a “spider”, “big midge”, “figure eight”, “dark spot”, “analemma”, “circle” " and so on. The kaleidoscope can change: every day a new form. If the fastening ring does not come off, but simply stretches out, to hell with the kaleidoscope, you can live. But if it pulled the retina and tore off a piece, then there are retinal tears, detachments, and in general a lot of troubles.
This is how the ophthalmologist sees the Weiss ring:
Treatment of tears before retinal detachment occurs is laser photocoagulation of the tear zones in several rows along the edge, so that the formed fusion sites hold the retina in place.
All this is treated with a good prognosis if you contact an ophthalmologist within the first days, with an average prognosis if you contact an ophthalmologist within a month. If the detachment has begun and the fluid that has entered through the gap continues to flow under the retina, peeling it off, the problems begin to become irreversible, and the question is about preserving vision as such, at least with some optical quality.
Therefore, if you suddenly see a lot of new “midges”, or they behave somehow strangely, or something else incomprehensible is happening in the eye, you should urgently go to an ophthalmologist.
Consequences of untimely therapy
If a patient does not see an ophthalmologist for a long time with a black cobweb before his eyes, complications gradually develop:
- complete loss of vision;
- disability;
- rhegmatogenous retinal detachment;
- macular hole;
- serious defects of the retina.
If a person has cobwebs floating before his eyes even after thoroughly washing and removing lenses, it is better to consult an ophthalmologist in a timely manner. The earlier the defect is detected, the higher the chance of complete preservation of vision.
Author's rating
Author of the article
Alexandrova O.M.
Articles written
2081
about the author
Was the article helpful?
Rate the material on a five-point scale!
( 1 ratings, average: 5.00 out of 5)
If you have any questions or want to share your opinion or experience, write a comment below.
“Mid flies” in the eye: so what to do with them?
If, after examination, the doctor finds no damage to the retina in the fundus and only notes the presence of microinclusions in the vitreous, then there is no need to worry
- there are no serious risks to vision in this case.
If the patient sees “garbage and midges” that bother him, but knows that there is no danger in this, the issue of dynamic monitoring and getting used to minor shortcomings in the quality of vision is most often discussed. In addition, after a couple of months, patients really stop noticing these inclusions and do not focus their attention on them.
But in some cases, complaints may be due to decreased vision due to “dirty” floating in front of the eye. Then, together with an ophthalmologist, a retina specialist (and not just a doctor in a clinic with a fairly rough knowledge of something from modern ophthalmology), the issue of treating this condition can be discussed.
There are two options: the first involves the destruction of fragments in the vitreous body using a modern YAG laser for laser vitreolysis, the second involves surgical removal of part of the vitreous body within the optical axis - a vitrectomy operation.
Treatment without surgery
The whole trick with the problem of “midges” and “spiders” is how to find a doctor who correctly interprets the changes in the eye.
The difference in incorrect diagnosis is colossal: to distinguish the degenerative calm state of simple destruction of the vitreous body from the pathological appearance of inflammatory cells, blood in the vitreous body, the onset of retinal detachment, vascular disorders and other things. That is, the patient is faced with the task of finding the expert who will reassure him or notice the problem in time.
The difference is in further tactics: the destruction does not need to be treated, you need to get used to it. In clinics, when there is a clear picture of DST (ordinary “garbage” in the eyes without the risk of further complications), they say: “Let’s prescribe resorption therapy.” And they prescribe certain “placebos”: emoxipin, taufon, katachrome. “Holy water” will help better in this case if you believe in it. A person feels good, and in a couple of weeks the brain builds a map of “dead pixels” and removes them on its own (at a high level, if you start looking closely, they will be visible again). If you start catching the “glitch” on purpose (as you may be doing right now), the distortions will be more noticeable. If you don’t think about them, you won’t see them. That's what is required. The brain is highly adaptable.
It’s another matter to overlook inflammation or the onset of retinal detachment. Here, “calming” methods cause the patient to lose a week or two, which will then lead to serious complications.
When surgery is indicated
Let’s agree that we are talking specifically about degenerative changes in the vitreous body, and not about the other above-mentioned conditions.
That is, when it is reliably known that from a medical point of view there are no risks, but something floating in front of the eyes still greatly interferes with vision. Option 1. Laser vitreolysis.
Any work in a closed vitreous cavity is potentially dangerous. It must be performed very accurately, since there are such sensitive structures nearby as the retina (especially its central zone) and the lens.
Ellex has recently proposed a new minimally invasive method for the treatment of vitreous pathology: Weiss rings, intravitreal opacities and adhesions, vitreous degeneration. This is a YAG laser device for treating the anterior and posterior parts of the eye using a targeted red diode laser. Since the structures adjacent to the vitreous body are very delicate, they came up with a reduction in the total energy due to the ultra-Gaussian profile of the laser beam. The small spot size and low optical breakdown energy (less than 1.8 mJ in air) perform photodestruction of inclusions in the vitreous body.
In practice, the effectiveness is 50%, because if the opacification is located close to the retina or close to the posterior capsule of the lens, or is too dense, etc., then application is impossible. Often one large fragment turns into several smaller ones; they can shift from the optical axis, or they can increase. In general, only after examination by a specialist with experience in laser surgery using this installation will you be able to find out whether this is your method.
Option 2. Vitrectomy.
This is a full-fledged abdominal operation with all the ensuing consequences. That is, it doesn’t matter whether a small “midge” swims or a “big spider” - the technology involves the work of a vitreoretinal surgeon. A vitrectomy—an operation to remove the vitreous—is performed as follows:
3 small punctures are made into the cavity of the eyeball in the projection of the plane of the ciliary body, that is, 3.5–4 mm from the limbus - the border of the transparent and opaque parts. The size of the piercing is measured in G units (Imperial radius unit). The standard 3-port sutureless technique is 23 G. Nowadays, most operations are performed using the 25 G technique - this is 0.445 millimeters. The dependence is this: the larger the G, the smaller the puncture size. The most gentle technique is 27G (0.361 mm). By the way, the smaller the puncture, the more expensive the cost of a set of consumables. For removing floaters, 27 G is ideal.
A solution balanced in salt and pH composition is supplied through one port to maintain the tone of the eye and maintain its volume during surgery, so that when the vitreous is removed, the eye does not begin to “collapse.” The second incision is needed to shine light into this “cave,” that is, the cavity inside the eye where the vitreous humor is located. In the third, the instrument itself is inserted - a vitreotome, a small guillotine with a tube. It looks like a micro-meat grinder, with the help of which the surgeon grinds the fibers of the vitreous body and sucks them into the cavity of the tube.
At the end of the operation, a balanced solution remains in the eye, which is then replaced with intraocular fluid. The ports are removed from the self-sealing sutures and a bandage is applied for a couple of hours.
In experienced hands, this operation takes 20 minutes under local anesthesia and the result is no gross floaters in front of the eyes, but any operation that opens the eyeball has a wide range of potential risks, posterior segment surgery doubles these risks.
In any case, I always make it clear to the patient that this is a very serious intervention with a minimal problem from a medical point of view.
From time to time, in case of severe clouding that reduces vision, it is necessary to perform such an operation for drivers, pilots, etc. - in cases where even slight short-term “fogging” can affect safety.
Are there treatments for this pathology?
There are no medications that have proven effective in eliminating the syndrome. At the same time, some medications improve metabolic processes, resolve spots before the eyes, and prevent the development of the disease. An improvement in the condition is observed in patients who have undergone treatment with Emoxipin and Wobenzym.
An effective addition to this therapy are special vitamin and mineral complexes containing lutein, which is necessary for the formation of the macula in the retina.
If damage to the retina has occurred, then the only way to prevent retinal detachment is laser surgery. The procedure is performed on an outpatient basis, under local anesthesia.
Two technologies are used for surgical treatment:
Vitreolysis. The operation is performed using a VAG neodymium laser. The beam acts specifically on the affected areas of the vitreous body, crushing them into small particles. Rarely used due to serious side effects.
Vitrectomy. The procedure involves cutting out the vitreous, or part of it, and replacing it with a balanced salt solution. The operation is unsafe, as there are many complications: hemorrhage, cataracts, retinal detachment. This risky operation has been proven to be highly effective and has positive responses from patients.
Modern ophthalmology, therefore, does not currently have effective and at the same time safe methods for treating floaters.
At the initial stage, you can completely defeat the disease by switching to a healthy lifestyle: a balanced diet without harmful foods; moderate physical activity; rejection of bad habits; Regularly performing special eye exercises for eye floaters syndrome.
"The Horror Story"
In my favorite Fedorovsky center, such patients who are worried about trifles because of the “midge” are told a story about a patient who came to the clinic with a complaint about the “midge”. He was told that it was not dangerous and there was no need to treat it. He insisted, the doctor from Fedorov’s clinic tried his best to dissuade him from the operation. He even suggested visiting a psychiatrist to find the answer to the question “How to live with such a “midge”?” The patient did not persuade the doctor from Fedorov’s clinic to perform the operation and flew to the States to look for someone who would agree to operate on him. Found. After the operation, inflammation of the membranes of the eye occurred. The eye went blind, became small, red and began to bother the patient. Already in Russia the eye had to be removed. Final: no eye - no midge.