Angiospasm is something that can happen to anyone, as it is a symptom that accompanies many pathological conditions.
Angiospasm refers to a functional disorder caused by a sharp narrowing of the central artery of the retina. No organic changes in the vascular wall are observed.
What is retinal vasospasm?
Angiospasm is a case when medical intervention is necessary. Very often, vasospasm develops against the background of pathological processes of the cardiovascular system (91.2%). Of these, it is most common in atherosclerosis and arterial hypertension (60% of all cardiovascular pathologies).
In approximately 1/4 of all cases of vasospasm (25-30%), the causes remain unidentified. The patient can be of absolutely any age, but men over 40 years of age are most susceptible to this disease.
How does spasm occur?
With vasospasm, spontaneous uncontrolled contraction of the smooth muscle layer of the vascular wall occurs. The reason for this is disruption of ion transport. If the amount of Na+ and K+ is too small, erratic contractions occur, and if the level of Ca+ increases, then the muscle fibers are in increased tone.
In essence, vasospasm is a narrowing of the artery along its internal diameter. It may be short-term, but even this is enough for adverse effects on the eye to develop. Due to this narrowing, oxygen starvation of the eye occurs. With repeated vasospasms, the eye does not receive enough oxygen, which results in weakening of the vascular walls, impaired circulation, ischemia of the retinal tissue, and possibly a retinal stroke and complete loss of vision.
Causes and risk factors
As already mentioned, a large number of all cases of vasospasm remain without identifying the exact cause. This is due to the fact that the etiology of the disease is not yet fully understood. However, there are many reasons why this condition can develop. These include:
- Arterial hypertension. When a person's blood pressure often rises above normal levels, a reflex spasm of blood vessels occurs not only in the brain, but also in the eye area. At such moments, there is a strong release of catecholamines (hormones that are a kind of response to an emotional or physical stressful situation). They contribute to compression of the receptors of the vascular wall, and vasospasm may occur.
- Diabetes mellitus, especially its decompensated forms, are often accompanied by various vision pathologies, in particular diabetic retinopathy. And this pathology, in turn, is often combined with manifestations of vasospasm.
- Atherosclerosis. With atherosclerosis, damage to the flat cells lining the inside of the blood and lymphatic vessels of the cavities of the heart is observed. Because of this, there is an increase in blood pressure and disruption of blood flow through the vessels. The result is the same oxygen starvation, muscle contraction and vasospasm.
- Smoking and excessive alcohol consumption lead to narrowing (sometimes very strong) of the retinal arteries. Nicotine and ethyl alcohol have this exact effect on the organs of vision. Gradually, the lumens of the vessels narrow, first temporarily, and then permanently.
- Poisoning of the body with compounds of carbon disulfide and lead. This is especially common among people who work in hazardous industries and constantly receive doses of these substances.
- Diseases of the endocrine system (especially the thyroid gland and thyroid-stimulating hormone deficiency) can cause the development of vasospasm in both eyes at once.
- Mental disorders caused by disorders of the central nervous system.
- Errors in nutrition.
- Prolonged strain on the organs of vision, fatigue (both mental and physical).
- Genetic predisposition.
- Osteochondrosis of the cervical spine. If hernias occur, they can put pressure on the vessels and blood does not circulate well through them.
- Severe traumatic brain injuries.
- Hemorrhages and neoplasms in the brain. In case of injury, narrowing of the arteries of the head is a reflex reaction to prevent bleeding.
- Diseases of the heart and blood vessels.
- Frequent and severe stress, chronic fatigue. This also includes the period of serious hormonal changes in the body - pregnancy, puberty, menopause.
- Risk group - weather sensitivity, constant eye strain (for example, working at a computer), frequent hypothermia, toxicosis of pregnant women, drug addiction.
Pathogenesis
When the vascular walls sharply narrow, blood flow becomes minimal or stops altogether. This cannot but affect the retina of the eye, ischemic changes begin in it, and there is a violation of tissue trophism (cell nutrition processes) necessary to preserve the functions of the eye.
Retinal vasospasm: causes of the disease, main symptoms, treatment and prevention
It is a functional disorder that is provoked by a sharp narrowing of the central retinal artery or its branches, which is not accompanied by the development of organic changes in the vascular wall.
Causes
The reason for the development of such a spasm has not yet been established. When it is not possible to find out the causes of the pathology, one considers idiopathic forms of the disease. When retinal vasospasm occurs in children, it is associated with spastic damage to the middle layer of arteries and autonomic disorders, as well as some features of the formation of the peripheral nervous system.
The main factors for the appearance of retinal vasospasm in adults are
Hypertonic disease. In this case, the disease is associated with vasospasm, including the eye area. This condition may occur due to the intense release of catecholamines, which have a pressor effect on the receptors of the vascular wall.
Diabetes. In the decompensated form of diabetes mellitus, there is a high risk of diabetic retinopathy, which is accompanied by frequent episodes of vasospasm.
Atherosclerosis. Atherosclerotic damage to the vascular endothelium is accompanied by increased blood pressure and impaired perfusion. In response to hypoxia, a spastic contraction of the muscular layer of the central retinal artery or its branches occurs.
Bad habits. Retinal artery spasm can occur due to increased nicotine content in smokers or ethyl alcohol in people who abuse alcoholic beverages. Such substances can cause a temporary narrowing of the lumen of blood vessels, which is replaced by dilatation.
Intoxication. Sometimes the cause of increased tone of the vascular wall is poisoning with compounds of carbon disulfide and lead. Persons working in hazardous industries and suffering from chronic intoxication are susceptible to the occurrence of such a pathological reaction.
Symptoms
Most often, this pathological condition is characterized by a bilateral, less often unilateral course.
During the narrowing of the lumen of the central retinal artery or its branches, the patient may experience the appearance of flickering floaters or a veil before the eyes.
Blurred vision with a short spasm is transient. Sometimes such patients may experience distortion of visual perception such as meta- and photomorphopsia.
Sometimes the patient may experience a feeling of discomfort in the orbital area on the affected side. There may also be a sensation of pulsation in the temporal region, dizziness and headache. After the end of the attack, the patient’s general condition is completely normalized, and visual dysfunction disappears. With prolonged ischemia, an irreversible decrease in visual acuity may occur.
Diagnostics
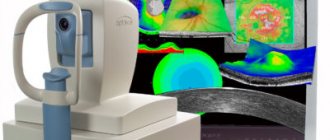
When diagnosing the disease, the patient undergoes a medical history and examination of the eye, as well as ophthalmoscopy, non-contact tonometry, retinal angiography and optical coherence tomography of the retina. When scanning the central region of the retina, a sharp thickening of the macula, complete smoothing of the foveal recess and a decrease in the reactivity of the retina can be determined.
Treatment
At the moment, no etiotropic treatment regimen for retinal vasospasm has been developed. Pathogenetic therapy is aimed at dilating spasmodic vessels in order to restore retinal blood flow in the ischemic area.
During an attack, the efforts of specialists should be aimed at eliminating the spasm, since prolonged disruption of microcirculation can cause complete or partial loss of vision.
To do this, such patients are prescribed infusions of antispasmodics and plasma substitutes, after which electrophoresis is performed with peripheral vasodilators and vasodilators.
To reduce intraocular pressure, the patient can be prescribed saluretics and carbonic anhydrase inhibitors. If there is no effect, an irrigation system is installed in the retrobulbar space. Instillation of beta-adrenergic blocker solutions may also be prescribed.
Prevention
Nonspecific prevention is based on ensuring control of blood pressure and blood glucose levels, taking statins for atherosclerosis and using personal protective equipment when working with pesticides in an industrial environment.
Source: //www.obozrevatel.com/health/bolezni/angiospazm-setchatki.htm
Symptoms
The following symptoms indicate that retinal vasospasm is developing:
- Deterioration or distortion of vision (fogging for 1-5 minutes at first, then up to an hour).
- Flickering of flies before the eyes, the appearance of sparks, rainbow spots, darkening.
- Headache – sometimes severe and sudden, paroxysmal, dizziness.
- Discomfort in one or both eyes.
- Pulsation in temples.
- Redness of the mucous membrane of the eye, swelling.
All these symptoms are most often transitory in nature. After the attack, the condition returns to normal, vision is restored. The exception is cases of prolonged ischemia - visual acuity decreases irreversibly. Angiospasm is most often unilateral, but sometimes there can be a bilateral course of attacks.
When a person notices several of the described symptoms at once, this indicates that he needs to go to the hospital.
Symptoms of retinal vasospasm
The most common symptom of retinal vascular damage is visual distortion (photomorphopsia). The patient may also be bothered by “fog” in the eyes, which can last from a few minutes to an entire hour. Floating spots before the eyes are also a sign of vasospasm. If all of the above symptoms occur, you should immediately consult an ophthalmologist. He will have to examine the fundus of the eye using special instruments, this will help identify narrowing of the retinal vessels.
Diagnostics
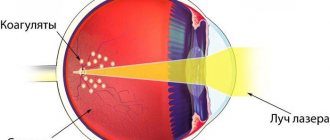
- Ophthalmoscopy is the main method for diagnosing vasospasm. During the procedure, a mirror or electric ophthalmoscope can be used. This manipulation allows us to identify narrowing of the arteries and all their branches, pallor of the fundus, swelling of the optic nerve and its waxy tint. Such an examination does not require special preparation, and it does not take much time.
- Blood and urine tests are necessary, because vasospasm is often a consequence of diseases of the internal organs.
- Non-contact tonometry is a test for measuring intraocular pressure.
- Retinal angiography is an examination of the fundus of the eye to study the condition of the retinal vessels.
- OCT of the retina is optical coherence tomography, the latest technology for the most accurate study of eye tissue.
Symptoms and diagnosis
With retinal vascular spasm, patients complain of the following:
- periodic blurred vision (can last from 1-5 minutes to an hour);
- the appearance of spots before the eyes;
- headache;
- discomfort in the eye area;
- sensation of pulsation in the temples;
- distortion of vision.
Important information: How to treat moderate myocardial hypoxia (oxygen starvation of the heart) and what are its symptoms
Signs of eye changes and well-being depend on the location of the pathological process and the presence of concomitant diseases. Thus, patients with stage II cervical spine osteochondrosis complain of changes in visual perception, darkening, the appearance of flickering, sparks and colored spots before the eyes. During an attack, hyperemia (redness of the mucous membrane of the eyes) and swelling of the conjunctiva are possible. After the end of the attack, visual dysfunction can be leveled, and the general condition of the patient can be completely normalized.
The main method for diagnosing the disease is ophthalmoscopy using a mirror or electric hand-held ophthalmoscope. If you conduct an examination during spasms, you can detect characteristic signs of malnutrition in the fundus:
- a sharp narrowing of the CAS and its branches;
- pallor of the fundus;
- swelling and waxy appearance of the optic disc.
The examination does not require special preparation of the patient, it is painless and does not take much time. Diagnostics includes testing, because in most cases, vascular spasms are associated with diseases of internal organs and systems, and if necessary, additional examinations are prescribed:
- non-contact tonometry;
- retinal antiography;
- Retinal OCT.
Treatment
Once the diagnosis is accurately established, treatment begins. It will be carried out jointly by an ophthalmologist and a therapist. In some cases, a cardiologist, neurologist or endocrinologist is involved - this depends on the pathology of the internal organs.
The most important thing in treatment is to expand the spasmodic vessel to ensure normal blood flow. Symptoms need to be relieved as soon as possible, since too long a disruption of blood circulation leads to oxygen starvation and partial or complete loss of vision.
It is also very important to begin treatment of the underlying disease, which causes such a complication as vasospasm. If this is not done, then the attacks will repeat again and again.
Drug treatment
It includes taking vasodilating drugs (Cavinton, No-shpa, Papaverine and others). In addition, sedatives (for prolonged stress) and dehydrating drugs are prescribed (to remove excess fluid from the body and lower blood pressure, as a result of which the reflex resistance of the vascular walls is removed) - Hydrochlorothiazide.
If there is pronounced discomfort in the eye area, a retrobulbar injection of Atropine (0.1%) or injection of Papaverine into the muscle is prescribed. Also, depending on the symptoms and the main diagnosis, medications are prescribed that provide cells with oxygen, for example, Nootropil.
Medications that prevent blood clots and improve blood flow - Trental - may be prescribed. Therapy is usually carried out on an outpatient basis. Sometimes, in the absence of positive dynamics from treatment, inpatient treatment may be recommended.
If there is severe intoxication of the body or euclampsia, the patient is hospitalized on an emergency basis. For pregnant women, all drugs are prescribed with great precautions so that side effects do not have a negative impact on the fetus.
Traditional treatment
Used:
- St. John's wort, yarrow and chamomile - these herbs, 1 tbsp each. brew in 1 liter of water, infuse for 15-20 minutes and take morning and evening.
- Valerian and lemon balm 2 tbsp each. pour water and leave for 3 hours, then the mixture is steamed in a water bath for 15-20 minutes and taken in small portions throughout the day.
- Horsetail, bird knotweed and hawthorn (flowers) 1 tbsp each. 1 liter of water is poured in, the solution is infused and consumed orally 20-30 minutes before meals.
Treatment methods
How the retina changes during the development of the disease
Treatment of vasospasm is an important process. An individual course of treatment is selected for each patient. It is necessary to take into account the age of the patient, the type of pathology, the reasons that caused it, etc.
Interesting! Therapy is aimed primarily at relieving symptoms and eliminating factors that provoked the development of the disease.
Conservative methods
This includes the use of drugs from several groups, with their help you can eliminate the pathological process:
- Vitamin complexes: B15,12, 1;
- Preparations to reduce vascular permeability: Gingko, Parmidine;
- Strengthening preparations: Vazonit, Kaviton;
- Improving microcirculation: Emoxipin;
- Prevents the formation of blood clots: Trombonet.
Conservative therapy is rarely used to treat pregnant women, since side effects can negatively affect the condition of the fetus.
Physiotherapy
Hemorrhage
How to relieve vascular spasm in the organ of vision using physiotherapy:
- Laser irradiation purifies the blood. It becomes less toxic, the immune system is strengthened.
- Magnetotherapy improves blood circulation, cells become more permeable, inflammation and pain are relieved.
- Acupuncture – recommended for the treatment of angiopathy that occurs after injury.
The price of such treatment varies.
Traditional methods
Arterial spasm can be relieved not only by traditional methods, but also by traditional medicine.
The methods do not completely eliminate the pathology, but improve the patient’s condition. The safest recipes:
- Take half a tablespoon of St. John's wort, chamomile and hot water. Mix, leave for half an hour, strain. Every morning on an empty stomach, drink 1/5 of the resulting product.
- Take fifteen grams of lemon balm, yarrow, and valerian. Separate two spoons, pour a glass of boiling water, let it brew for three hours. Boil in a water bath for fifteen minutes, strain. Add water, the total volume should be 0.25 liters. Drink the prepared product throughout the day.
You can use folk remedies only after visiting a doctor. It is unacceptable to use such methods as the main treatment.
Proper nutrition
During diabetic and hypertensive angiopathy, a special diet is required. You need to avoid foods that contain a lot of cholesterol.
Important! A doctor should prescribe proper nutrition.
If you are diabetic, avoid the following foods:
- Mustard;
- Alcohol;
- Spicy dishes;
- Sweet fruits;
- Sugar.
For hypertensive angiopathy, the following restrictions are provided:
- No strong tea or coffee;
- Fatty dishes and broths are not allowed;
- Spicy dishes;
- Smoked sausages or fish;
- It is too salty.
You need to stick to this diet exactly as much as your doctor recommends.
Forecast
The prognosis depends, first of all, on the cause of the attack, that is, on the underlying disease. The duration and frequency of attacks is also important.
If the attacks return very often and last more than 15 minutes, then the prognosis cannot be called favorable. In such cases, irreversible consequences often develop. Timely treatment is the key to a favorable prognosis.
Possible complications
Complications that can develop after attacks of vasospasm of the retinal vessels include retinal dystrophy or stroke, hyperopia, thrombosis or embolism of the retinal arteries, optic nerve ischemia, and glaucoma. The most dangerous consequence is complete loss of vision.
Preventive measures
There are no preventative measures as such. We can only advise you to lead a healthy lifestyle, undergo regular examinations by an ophthalmologist, eat right, protect yourself from stress, ensure that you get good sleep and reasonable physical activity.
It is also important that your eyes do not become too tired, especially when working at a computer. Breaks are important here, at least short-term, for 3-5 minutes. Hypertensive patients must control and stabilize their blood pressure, diabetics - their blood sugar levels. People working in hazardous enterprises must take all precautions and use protective equipment.
Watch a video about retinal vascular angiopathy: