Central retinal artery occlusion (CRA) is a disease that affects the retina of the visual organs, located on the back wall of the eye.
The retina of the eyes contains rods and cones that perceive light and send nerve impulses to the brain, as a result of which a person sees the world around him. The retina needs a constant supply of blood. Blockage of arterial and venous vessels can cause blood and fluid to accumulate in the retina, which interferes with light perception and leads to loss of visual ability. The degree of visual impairment depends on the area where the thrombus occurred.
The disease is most often diagnosed in middle-aged and elderly people, with the majority of patients being men over 60 years of age. In women, the pathology occurs 2 times less often.
Occlusion of the central retinal artery is a pathology in which blood circulation stops in the branches or in the basin of the central retinal artery. In about half of the cases, the blockage causes vision loss on one side. In approximately 40% of cases, arterial occlusion affects the branches of the artery and causes blindness in the corresponding visual field. In some cases, blockage of the central nervous system develops with other pathologies of the visual system.
Acute blockage can lead to impaired blood flow and retinal ischemia. A sudden circulatory disorder in the central artery in most cases leads to permanent loss of vision in one eye.
Reasons for development
Occlusion can develop in both the central vein and the central artery of the retina. How severe the loss of visual ability will be depends on the location of the blood clot and the severity of the blockage. So, in some cases, patients’ optic nerves and the retina itself, which receives oxygen and other necessary substances, are under attack. Obstruction of the central retinal artery can lead to narrowing of the fundus vessels.
The mechanism of development of the pathology is often associated with retinal spasms, the formation of blood clots in blood vessels, embolism, and vascular insufficiency.
Most often, occlusion of the central nervous system is a consequence of some pathological phenomena in the body.
The likelihood of developing vascular blockade increases as a person ages. The causes of the pathology can be:
- high blood pressure;
- vascular atherosclerosis;
- temporal arteritis;
- increased cholesterol levels;
- papilledema, macular degeneration.
In young people, blockage of a central vein or artery may develop for the following reasons:
- inflammation of the inner lining of the heart of an infectious nature;
- dysfunction of the left heart valve;
- tachycardia;
- type 2 diabetes;
- disorder of the cardiovascular system, dystonia;
- antiphospholipid antibody syndrome;
- excess body weight;
- intravenous administration of narcotic drugs, which increases the likelihood of thromboembolism;
- smoking;
- rare blood diseases, increased blood clotting.
Predisposing factors may also be:
- rheumatism of the fundus vessels;
- increased intraocular pressure;
- retrobulbar hematoma;
- oncological neoplasms;
- emboli in blood vessels;
- long bone fractures;
- bleeding in internal organs;
- previous surgical interventions on the eyes.
All these factors can cause a slowdown or cessation of blood circulation in the vessels and lead to ischemia.
If the patient receives assistance in the first 40 minutes after loss of vision, the likelihood of partial restoration of visual abilities increases several times.
Prolonged lack of oxygen can provoke necrosis, death of the optic nerve and, as a result, complete and irreversible loss of the ability to see.
Causes
The mechanism of the pathology may be due to spasm, thrombosis, embolism or collapse of retinal arterioles. Often, incomplete and complete occlusion is caused by blockage of retinal vessels with calcified, cholesterol or fibrinous emboli. But in any case, occlusion of the central artery is a consequence of systemic chronic or acute pathological processes.
The main risk factors for occlusion in old age are: arterial hypertension, giant cell arteritis (Horton's disease), atherosclerosis. In younger people, these may be circulatory disorders in the retinal vessels associated with infective endocarditis, damage to the valvular apparatus of the heart muscle, heart valve prolapse, arrhythmia, neurocirculatory dystonia, antiphospholipid syndrome, diabetes mellitus.
Local provoking factors for thrombosis of the central retinal artery are often retinovasculitis, edema, optic disc drusen, ophthalmotonus, compression of the orbital vessels by retrobulbar hematoma or tumor, and ophthalmological operations.
The potential danger of occlusion exists with hypercoagulability syndrome, fractures of long bones, intravenous injections associated with the risk of thromboembolism, air or fat embolism. Collapse of retinal arterioles is also possible with massive blood loss due to uterine, gastrointestinal or internal bleeding.
Spasm, thromboembolism or collapse of arterioles leads to a slowdown or complete cessation of blood flow in the affected vessels, leading to acute ischemia of the retina. At the same time, if blood flow is restored during the first 40 minutes, it is possible to restore some of the impaired visual functions. If hypoxia continues for a longer period, necrosis of ganglion cells and nerve fibers develops in the retina, followed by their autolysis, which makes the return of vision impossible. The outcome of central retinal artery occlusion in most cases is optic nerve atrophy with irreversible blindness.
Classification
Retinal vascular occlusion is divided into the following types:
- Occlusion of the central artery. With this type of pathology, a blockage occurs in the main artery, which is enriched with oxygen and delivers blood to the retina of the eye.
- Occlusion of the CAS branch. Occurs when there is a thrombus of small branches of the artery.
- Occlusion of the central retinal vein. This is a blockage of one of the venous vessels.
Central vein occlusion is divided into two types:
- Blockage of the central retinal vein. In this disorder, obstruction of blood flow occurs in the main vein.
- Branch retinal vein block. It is observed with embolism on the branches of the vein.
The most dangerous is considered to be blockage of the central retinal vein. This type of disease is characterized by a sharp painless loss of a person’s visual ability.
Symptoms of occlusion
Most often, occlusion of the central retinal artery or vein is unilateral. Usually, blockage of blood vessels occurs unexpectedly for a person and does not cause pain. The patient experiences sudden loss of vision in one eye in just a few seconds.
About 10% of patients experience short-term visual disturbances, and thrombosis may be preceded by flashes of light and blurred vision in the field of vision. In rare situations, loss of visual fields is observed.
The severity of visual impairment can range from the ability to distinguish objects to complete loss of visual function in one or both eyes.
Impairment or loss of visual ability can occur either temporarily or permanently.
If there are any signs of vision deterioration, the patient needs urgent consultation with a specialist. To do this, you should go to the emergency room.
Temporal arteritis
Temporal arteritis, also known as Horton's syndrome (HS) or granulomatous giant cell arteritis (GCA), is a pathological process in the body characterized by severe headaches in the temporal region. According to some reports, women suffer from this disease much more often than men.
The disease mainly affects older people, usually those 55 years of age and older. However, cases have been recorded where the disease affected people under 40 years of age.
The disease is expressed by changes in medium and large blood arteries; they are located very close to the carotid artery, but small capillaries are not affected by this disease.
Basically, only individual arteries are affected, the main function of which is to supply the brain with blood.
Localization is in one area of the head, maybe in the optic nerve, vessels supplying the eyes, or in a certain area of the cerebral cortex.
Causes
Horton's syndrome is a rheumatic disease that has a very negative effect on the human immune system. Why this happens has not been studied. Most likely, the occurrence of the disease is associated with infectious processes in the body that were caused by viruses or bacteria, for example, rubella, chickenpox, pneumonia, hepatitis or influenza.
In approximately 1/3 of those with this disease, a hepatitis marker and antibodies to it are detected in a blood test; in addition, this antigen is located precisely in the walls of the affected arteries. Also, another cause of temporal arteritis may be a genetic predisposition to this disease.
People with HLA-DR4 proteins, which are localized in white blood cells, are most susceptible to this pathology.
Polymyalgia has been noted to be a comorbidity of temporal arteritis. It is also a pathology of a rheumatic nature.
The symptoms of temporal arteritis depend on the stage of human vascular damage; they differ slightly from each other, but there are also those that are characteristic of all stages. Often, a recent respiratory illness can be seen in the medical history.
The symptoms are as follows:
- Headache. Its localization is mainly in the temporal region, but can also be felt in the parieto-occipital region. The pain is very similar to a migraine. Often, pain is present only on one side. Intensifies with pressure, chewing, turning the head or coughing.
- You feel tension and fatigue in your masticatory muscles. It may be that the patient cannot eat food during painful attacks.
- If the optic nerve and ocular vessels are damaged, vision deterioration may occur. Characterized by sudden loss of vision in only one eye.
- Pain in the eyes when looking up, down, right or left.
- Increased fatigue.
- Increase in body temperature to subfebrile level.
- Loss of appetite and severe weight loss.
- Sudden jumps in blood pressure.
- The scalp in the hair area becomes thinner, which can cause pain when touched.
- Externally, you can notice a strong swelling of the temporal artery.
If you suspect temporal arteritis, you should consult a rheumatologist or neurologist.
To diagnose and make an accurate diagnosis, the doctor must:
- Palpation of the temporal region. A bulging and strongly pulsating artery is palpated, the patient feels pain, and nodules are palpated along the entire vessel.
- General and biochemical blood test. The blood will immediately show whether there is an inflammatory process. The main indicators are ESR (erythrocyte sedimentation rate), CRP (C reactive protein).
- Biopsy of the temporal artery to identify changes in the walls.
- Consultation with an ophthalmologist, fundus examination.
- Ultrasound (ultrasound examination) of blood vessels, viewing the walls of the arteries and their changes that lead to a narrowing of the lumen.
When temporal arteritis is confirmed, there are two treatment methods: surgery or drug treatment, which only helps to relieve the disease.
In drug treatment, drugs of the glucocorticosteroid group are prescribed. These are hormonal drugs, and the dosages are quite significant.
The most common prescribed drug is Prednisolone, and there are many analogues. The dosage of Prednisolone must be prescribed by a doctor individually for each patient.
The dosage depends on the picture of the disease, both normal and high are possible.
In the acute stage of the pathology, Prednisolone is often administered intramuscularly or intravenously. As soon as the acute attack is over, you can return to taking the medicine in tablet form.
The duration of drug therapy is also prescribed by the doctor, usually the treatment period is 14 days. When taking glucocorticosteroids, constant monitoring of blood pressure and blood sugar levels is required.
If Prednisolone is prescribed for a very long period, then in parallel the doctor prescribes drugs that maintain the level of potassium in the patient’s blood.
A special diet must be prepared. This is done in order to prevent the occurrence of hypokalemia.
Another mandatory drug, methandrostenolone, is introduced, its main goal is to avoid the occurrence of catabolism and osteoporosis.
Contraindications for the use of Prednisolone are:
- Individual intolerance to the components;
- Frequent increases in blood pressure;
- Diabetes;
- Acute endocarditis;
- Nephritis;
- Stomach ulcer;
- Psychoses;
- Postoperative period;
- Active form of tuberculosis.
To prevent the formation of blood clots in the patient, heparin drugs are prescribed. The dosage and method of administration are prescribed by the doctor individually for each patient. Anticoagulants are strictly prohibited if the patient has hemorrhagic diathesis and other diseases that initiate weak blood clotting.
Contraindications for heparin:
- Increased vascular permeability;
- Severe disorders of the kidneys and liver;
- Anemia;
- Venous gangrene;
- Leukemia;
- Endocarditis;
- Bleeding;
- Aneurysm.
If the course of temporal arteritis is very severe, then the doctor may decide in favor of surgical intervention. This operation is called angioprosthetics. Represents the elimination of affected areas in the venous bed. The decision to perform surgery is made if there are complications of temporal arteritis.
The period of drug therapy with a confirmed diagnosis can be quite long. Usually it is from ten to twelve months, and sometimes much longer.
There are also traditional methods of treatment for temporal arteritis, but do not forget that this is a very serious disease. Folk remedies are not ways to completely get rid of the disease, but will only help alleviate the condition.
Herbal decoctions that help reduce headaches:
- Maryin root.
- Siberian elderberry flowers.
- St. John's wort.
- Peppermint.
- Coltsfoot.
- Common wormwood.
- Common oregano.
- Red clover.
- Valerian root.
- Dill seeds.
There are also various folk methods:
- Cut a small leaf of indoor aloe lengthwise to create two halves. Lie down in a dark room and apply the cut to the temporal area, remain in this position for about 30 minutes.
- Lubricate the temporal and frontal area with garlic juice.
- Add a few cloves of garlic to the milk and bring to a boil. Wait a little time to brew and cool until warm. Place 5-10 drops of the decoction into each ear canal, then tilt your head so that all the liquid drains out.
- Wrap slices of raw potatoes in gauze and apply to the temporal and frontal areas.
- Cool the boiled potatoes in their jackets a little and apply warm to the temporal and frontal areas.
- Relaxation, a state of complete peace and meditation.
- Raw potato juice should be drunk immediately after cooking.
- Eating potatoes throughout the day. It is necessary to boil one kilogram of potatoes, peeling them and without adding salt. Then, eat one potato at a time all day, dipping it in sugar.
- Lie down with your eyes closed or fall asleep.
You shouldn’t expect the impossible from folk methods. They will not be able to completely get rid of the disease, but will only relieve pain. Therefore, you should immediately consult a doctor so that he can prescribe the necessary treatment.
If treatment of the disease is ignored, other arteries may be affected. Often, the kidneys are the first to suffer.
The most important complication of temporal arteritis is complete loss of vision or other problems in the field of ophthalmology.
Complete blindness occurs due to the fact that there is a violation of blood flow through the inflamed arteries to the eyeball and optic nerve.
As a result, the nervous tissue of the retina dies, and the patient may become completely blind. The consequences of the disease can be ischemic disorders leading to a stroke.
Also, as a complication of temporal arteritis, a malfunction of the gastrointestinal tract is possible; against this background, other diseases may develop.
Prevention
Unfortunately, it is impossible to give precise recommendations in order to prevent the occurrence of this disease, since the nature and sources that provoke temporal arteritis are not fully understood.
Secondary prevention of this disease consists of lifelong use of immunosuppressants and steroid hormones.
In order to stop headache attacks, you should choose the most effective drug for yourself and use it.
Source: https://oftalmologiya.info/zabolevaniya-glaz/281-visochnyy-arteriit.html
Diagnosis of pathology
A thorough history will help make the correct diagnosis. The specialist must find out what systemic pathologies the patient suffers from, whether there has been damage to the organs of vision, whether there are heart problems, whether there are inflammatory diseases, metabolic disorders, as well as severe vascular diseases of the retina.
The necessary research methods are:
- Fundus examination. Using biomicroscopy, the degree of occlusion can be determined, and the eye’s reaction to light will be reduced or absent altogether. The center of the macula will usually be brightly colored and the arterioles will be narrowed. Examination of the fundus of the eye using an ophthalmoscope will reveal swelling of the optic disc, loss of transparency and pallor of the retina.
- Perimetry. It will help identify scotomas and narrowing of visual fields.
- Visometry. If there is an occlusion, the specialist will detect a deterioration in visual clarity, the severity of which depends on the degree of blockage.
- To determine the location of the blood clot, fluorescein angiography is performed, which will determine the degree of blockage of the vessels and slowing of blood flow.
- Electroretinography will reveal a decrease in the amplitude of wave oscillations. This may indicate the death of ganglion cells.
Also additionally carried out:
- dopplerography of eye vessels;
- optical coherence and laser tomography;
- tonometry;
- laboratory diagnostic methods: hematological blood test, coagulogram, lipid spectrum analysis, biochemical study, blood culture;
- Ultrasound of the heart and carotid arteries.
Some patients require consultation with highly specialized doctors - hematologist, surgeon, cardiologist, endocrinologist, rheumatologist, infectious disease specialist.
The short posterior ciliary arteries supply the outer layers of the retina
The main vessel supplying the eyeball is the ophthalmic artery (a. ophthalmika).
This artery is the main branch of the internal carotid artery. It enters the cavity of the orbit, forms an arc and is divided into many branches. The ophthalmic artery gives rise to:
— Central retinal artery. As is clear, this branch of the ophthalmic artery nourishes the retina, entering it with a single trunk and giving back a small branch. This vessel of the eye supplies the medulla of the retina and the intraocular part of the optic nerve head;
- Posterior short ciliary arteries. These branches of the ophthalmic artery supply blood to the sclera of the posterior pole of the eyeball. Merging together, they form the so-called arterial circle of Zinn-Haller. They also form their own choroid, the choroid. It, in turn, supplies blood to the neuroepithelial layer of the retina.
There is also evidence that these eye vessels penetrate the ciliary body, but they do not play a special role in its nutrition.
The clinical feature of the posterior short branches is that they do not anastomose with other vessels of the eye, therefore inflammatory processes developing in the choroid proper do not lead to hyperemia of the eyeball.
— Two posterior long ciliary arteries. Located slightly distal to the posterior short ciliary arteries. Their main function is to supply blood to the ciliary body.
- Muscular arteries. These branches of the ophthalmic artery are divided into:
-) superior, blood-supplying muscles, levator palpebrae superioris, superior rectus and superior oblique;
-) lower, supplying blood to the remaining oculomotor muscles.
- Medial arteries of the eyelids. Merging with each other, they form the arterial arch of the eyelids (upper and lower). It also sends branches to the conjunctiva.
- Anterior and posterior conjunctival arteries. These eye vessels supply the conjunctiva.
- Lacrimal artery. It departs from the arch of the ophthalmic artery and is located between the superior and external ocular muscles, giving them its branches. Also takes part in the formation of arterial arches of the eyelids.
- Supraorbital artery. A rather large vessel of the eye, originating from the ophthalmic artery and passing through the notch of the same name in the frontal bone. Nourishes the muscles and soft tissues of the upper eyelid.
- Supratrochlear artery. It goes together with the trochlear nerve.
- Ethmoidal arteries. These are independent branches of the ophthalmic artery, slightly supplying the orbit.
The maxillary artery is divided into:
- Infraorbital artery. It goes on the channel of the same name. It nourishes the lower eyelid and also supplies blood to the inferior rectus and inferior oblique muscles, the lacrimal gland and the lacrimal sac.
- Facial artery. The angular artery comes from this vessel of the eye.
What is arterial anastomosis
When there is difficulty in blood flow through a large artery supplying organs or limbs, the roundabout movement of blood is activated. It is called collateral and the reason for its activation can be physiological compression of the main vessel (for example, tilting or turning the head), physical, emotional activity or pathological changes.
Bypass circulation becomes especially important when the lumen of a vessel is blocked by a thrombus, atherosclerotic plaque, embolus, or narrowing due to persistent spasm.
The vessels through which collateral blood flow passes are called anastomoses. Normally, spasm predominates in them, which redirects blood to the main lines. If there is an obstacle to the movement of blood through the main arteries, the anastomoses experience increased pressure on the walls. Due to this, the structure of their muscle and elastic fibers changes, they acquire a wider lumen.
If anastomosis is an anatomical concept, it always exists and connects two vascular branches, then collateral means a bypass movement of blood during disease or stress.
In addition to existing anastomoses, newly formed ones can also be used for collateral blood flow. That is, the blood moves along a more complex trajectory.
We recommend reading the article about cerebral artery hypoplasia. From it you will learn about the causes of hypoplasia of the cerebral arteries, symptoms, methods of diagnosis and treatment of cerebral arteries. And here is more information about carotid artery stenosis.
Anatomy of the forehead: what layers does the zone consist of?
From an anatomical point of view, the forehead can be considered as a structure consisting of 5 layers :
- leather;
- subcutaneous tissue;
- aponeurotic layer;
- loose connective tissue;
- periosteum.
Recent studies have shown the presence of distinct septa between the periosteum and the frontalis muscle :
- superior frontal septum;
- inferior frontal septum.
They act as attachment points for the frontalis muscle .
Thanks to this, the frontalis muscle at the lower point of attachment between the eyebrow and the inferior frontal septum can serve as a levator , and between the inferior frontal septum and the superior fibers - a hairline depressor .
Recommendations for forehead correction with botulinum toxin
It is advisable to resort to botulinum therapy for the forehead if the target muscle is the main cause of disruption of facial harmony.
The literature describes various techniques for administering and dosing the toxin to smooth out horizontal forehead wrinkles by injection into the frontalis muscle.
When examining a patient's upper face, the doctor should assess:
- lateral and medial muscle activity;
- asymmetry;
- compensation for eyebrow ptosis;
- muscle mass;
- eyebrow width;
- forehead height.
The shape and height of the eyebrow is influenced by the interaction of the frontalis muscle and the medial glabellar complex.
The number of injection points can be determined by the degree and location of muscle contraction (from 5–7 to multiple injection points).
Types of anastomoses
In the circulatory network, connections between vessels can be of several types.
Intrasystem and intersystem
If the anastomosis is intended to move blood between branches of the same vessel (for example, knee, brachial artery), then it is called intrasystemic. They are limited to the basin of only one large vessel and are used on a local anatomical area. They are the most common type of arterial anastomosis.
Source: https://vision-health.ru/zabolevaniya/nadblokovaya-arteriya.html
Treatment for central artery occlusion
The goals of therapy for blockade of the central artery or vein of the retina are:
- restoration of venous circulation;
- resorption of hemorrhage;
- removal of swelling;
- improvement of the trophism of the retina.
If there is a sudden deterioration in visual ability in one eye or the appearance of blind spots, one should not wait for the independent restoration of visual ability. The rapid development of the disease requires assistance to the patient as soon as possible.
Urgent Care
In case of occlusion, you should immediately contact a medical facility: further treatment may not bring results.
On the first day, the following measures should be taken:
- special massage of the eyeballs to move the embolus;
- paracentesis (incision) of the anterior cavity of the eye;
- Special local remedies that improve blood circulation, stimulate cell nutrition and increase oxygen will help reduce intraocular pressure;
- To normalize eye metabolism and microcirculation, vasodilating drops are used.
Despite the provision of urgent medical assistance, blind spots may remain in the field of vision. The clarity of the patient’s vision directly depends on the severity of the damage to the macula, the severity of edema and blood flow disorders.
After suffering from the disease, the patient must undergo regular examinations by an ophthalmologist after 1, 3 and six months.
Medications
A patient with occlusion of the central nervous system must be urgently hospitalized. Failure to seek medical help in a timely manner can result in disaster.
Therapy should begin immediately after the first symptoms of blockage occur: in this case, the favorable outcome of the disease increases.
In the first hours, drug treatment is used:
- for arteriolar spasms, vasodilators are used - Nitroglycerin, Euphyllin, Papaverine, oxygen inhalation, as well as oxygenation. Atropine eye drops are also used to relieve smooth muscle tone;
- for thrombosis of the central artery, thrombolytics, anticoagulants, and dextrans are taken. To dissolve blood clots, antithrombotic medications (Fibrinolysin) are prescribed;
- for any type of occlusion, retrobulbar and parabulbar injections are recommended with agents that dilate blood vessels, improve blood flow, and reduce blood clotting;
- they also use antioxidants and instillation of adrenergic blockers;
- when vascular tone is weakened, analeptics (Caffeine) are indicated;
- in the treatment of pathology, diuretics and anti-inflammatory drugs, as well as medications that stimulate blood circulation, are also used;
- It is mandatory to treat the corresponding disease that caused the blockage of the central artery or vein.
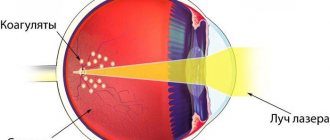
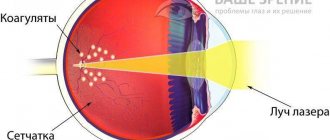
To eliminate occlusion and prevent complications, laser treatment is sometimes prescribed. To prevent the formation of a blood clot in the second eye, preventive therapy is used.