The retina is an important part of the eye that translates light into signals that travel along the optic nerve to the brain. Retinal detachment, unfortunately, is quite common. This is a serious ophthalmological disease, which in the absence of proper and timely treatment leads to loss of vision. Physiologically, retinal detachment is determined by its structure.
Several layers of cells take turns receiving light signals before converting them into a nerve impulse. During detachment, a layer of photoreceptors separates - those same rods and cones that are well known to everyone from school. In addition to the photoreceptor layer, all layers up to the outer layer, the epithelial one, peel off. Fluid accumulates between the layers of the damaged retina. The nutrition of the retina is disrupted, and vision rapidly declines.
Treatment for retinal detachment consists of soldering the layers and restoring normal cell nutrition. Ophthalmologists say that visual functions can be restored if treatment is started in the first month after detachment.
At CELT you can get advice from an ophthalmologist.
- Initial consultation – 3,500
- Repeated consultation – 1,800
Make an appointment
Causes of the disease
If we talk about the reasons, there are many of them. Most often, retinal detachment occurs due to its rupture due to eye injury or due to a congenital predisposition.
The following risk factors are identified:
- Myopia.
- Retinal dystrophy, congenital or age-related.
- Previous ophthalmological surgeries.
- Injuries to the eye, even those not related to the retina, increase the risk of detachment.
- Presence of diabetes mellitus.
- Cardiovascular diseases, malnutrition of eye structures.
Due to the large number of risk factors, there is no specific prevention. Treatment is carried out according to the same standard, taking into account the characteristics of a particular case.
Complications and consequences
Retinal detachment can provoke the development of a wide variety of negative consequences of the human visual system. Moreover, pathology itself often acts as a complication of certain diseases, and not only of the ophthalmological spectrum.
Most often, additional problems arise when retinal detachment is not diagnosed in a timely manner, in cases of unsuccessful operations or lack of treatment as such. With all this, even high-quality therapy provided to the patient on time does not guarantee the potential occurrence of pathological consequences.
Typical complications:
- Tears and perforations of the membranes adjacent to the retina. They provoke a whole range of ophthalmological problems, from diastasis to strabismus;
- The formation of hemorrhages caused by hemorrhages under the retina or into the vitreous body;
- Significant deterioration in the light transparency of the cornea and an increase in degenerative processes in it with the formation of erosions, leading to a decrease in the quality of vision and other pathologies;
- Slowing or stopping blood circulation in the central artery that supplies the retina. In turn, it causes local thrombosis and other pathologies of the cardiovascular system;
- Complete blindness in the terminal stages of retinal detachment.
Now you know everything about the symptoms, treatment and causes of retinal detachment.
Symptoms of retinal detachment
Symptoms characteristic of early stages of detachment and clinical manifestations of existing retinal detachment are identified.
The so-called harbingers include:
- Photopsia - light flashes before the eyes.
- Metamorphopsia - straight lines are bent, shapes and proportions are incorrectly perceived. It is important not to get confused, this is a characteristic sign of macular degeneration.
- Floaters before the eyes.
These are unreliable symptoms that may indicate other ophthalmic diseases. People with healthy eyes should pay attention to them and get diagnosed. For those who suffer from eye diseases, these symptoms may indicate an exacerbation or progression of other diseases.
Symptoms of retinal detachment:
- Early symptoms may include a hazy, foggy veil appearing before the eyes. There may be a feeling of darkening, a shadow before the eyes.
- Vision begins to decline rapidly. Moreover, a temporary improvement is possible in the morning.
- The field of vision narrows, improving in the morning. Most of the time there is a feeling of a black veil that prevents you from seeing.
The veil gradually spreads over the entire field of vision. Over time, retinal detachment leads to complete blindness. Therefore, it is important to start treatment at the moment the first signs appear. Time plays a huge role in the effectiveness of retinal detachment therapy.
Patient examination
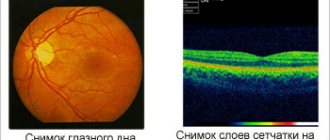
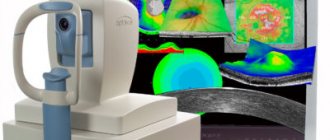
The main method for diagnosing retinal detachment or rupture is ophthalmoscopy. This is an examination of the fundus of the eye, which can be performed either in a standard way - using an ophthalmoscope, or by others. Retinal detachment is clearly visible during ophthalmoscopy. It is important to assess the shape of the detachment, the degree of damage, the location of retinal breaks, and notice dystrophy in time.
Other diagnostic methods are also used:
- Ultrasound examination (B-scan).
- Electrophysiological studies. They allow you to assess the extent of damage, learn about the capabilities of the retina and the level of loss of function.
- Measuring intraocular pressure. Carry out on both eyes. As a rule, with detachment there is a decrease in pressure compared to a healthy eye.
- It is important to evaluate the field of view. There is a special technique for this - perimetry. Interestingly, the field of view disappears on the side opposite to the detachment site.
After a comprehensive assessment of the eye condition, appropriate treatment is prescribed.
Secondary retinal detachment
Secondary retinal detachment occurs as a result of various eye diseases: inflammatory, penetrating wounds, neoplasms, vascular lesions of the retina (diabetes, hypertensive retinopathy, toxicosis of pregnancy, etc.). Wedge, the picture is characterized by a combination of O. s. with typical manifestations of the underlying disease. Unlike primary O. s. retinal breaks are often not detected.
After penetrating wounds O. s. caused by the formation of connecting cords or preretinal membranes in the vitreous body; in inflammatory diseases of the eye - chorioretinitis, scleritis - exudative detachment is sometimes observed, accompanied by opacities in the vitreous body, precipitates and other inflammatory manifestations in the vascular tract; in case of eye tumors, the retina is detached by a growing tumor and is characterized by rigidity, absence or a small number of retinal folds, and rare ruptures; diabetic retinopathy in the proliferative stage is often accompanied by retraction retinal detachment against the background of newly formed vessels and hemorrhages.
Treatment of secondary O. s. includes therapy for the underlying disease: for tumors according to indications - surgical treatment or photocoagulation; with post-traumatic and diabetic O. s. - conventional scleroplastic operations using vitrectomy to cut or remove the cords (see Vitreous body).
Bibliography:
Volkov V.V. Operations for diseases of the retina, Guide to eye surgery, ed. M. L. Krasnova, p. 264, M., 1976; Krasnov M. M. System of surgical treatment of retinal detachment, Vestn, ophthalm., No. 1, p. 3, 1966; Pivovarov N. N. and Prokofiev V. N. Mechanophosphene as an indicator of the functional state of the retina and its diagnostic value, ibid., No. 4, p. 34, 1974; Rosenblum M. E. Surgical treatment of retinal detachment, M., 1952, bibliogr.; Filatov S.V. Retinal detachment, M., 1978, bibliogr.; Shevalev V. E. and Babanina Yu. D. Surgical treatment of retinal detachment, M., 1965, bibliogr.; Arruga N. Sur la pathogenie et le traitement postoperatoire du decollement retinien, Ann. Oculist-. (Paris), t. 186, p. 507, 1953; Graefe A. Zur Lehre von der Netzhaut-ablosung, Arch. Ophthal., Bd 4, S. 235, 1858; Lincoff H. D., McLean J. M. a. Nano H. Cryosurgical treatment of retinal detachment, Trans. Amer. Acad. Ophthal. Otolaryng., v. 68, p. 412, 1964; Schepens C. A new ophthalmoscope demonstration, ibid., v. 51, p. 298, 1947.
HH Brewers.
Restoration of the retina after detachment
Retinal detachment is an acute disease that requires urgent treatment. If you start the disease by delaying treatment, the blood supply and nutrition of the cells are disrupted, resulting in changes that are difficult to treat and can lead to complete and irreversible loss of vision.
As a result of retinal detachment, the following diseases develop:
- Cataract.
- Chronic iridocyclitis.
- Subatrophy of the eyeball.
The essence of the treatment for detachment is to bring the layers of the retina together surgically. Conservative therapy does not help. It is also important to block the tear and repair the damage.
Vitrectomy
- Cost: 115,000 - 145,000 rubles.
- Duration: 30 minutes - 3 hours
- Hospitalization: 1 day in hospital
More details
Surgical methods are divided into two large groups:
- Extrascleral.
- Endovitreal.
The first method consists of performing an intervention on the surface of the sclera without penetrating the eyeball. Endovitreal surgery is operations that are performed from the inside of the eyeball.
Types of surgical intervention
The disease can be cured with laser, filling, or open surgery. The intervention is carried out immediately.
The main goal is to restore the structure of the membrane by bringing light-sensitive cells closer to the pigment epithelium. No retinal replacement is required.
Vitrectomy (removal of the vitreous)
It involves partial or complete removal of the vitreous body and replacing it with an artificial material (silicone, gas or solution). Microsurgery is indicated for retinal tears, retinopathy due to diabetes, and total retinal detachment.
The intervention proceeds as follows:
- make 3 small incisions;
- install an irrigation system (a device for circulating fluid);
- the vitreous body is removed;
- carry out tamponade;
- apply a suture.
Vitrectomy is contraindicated in cases of high intraocular pressure (glaucoma), malignant tumors, and coagulopathy.
Vitrectomy is one of the types of surgical intervention in the treatment of retinal detachment.
Extrascleral filling
It involves a mechanical effect on the retina with a filling (sponge). Filling can be radical, circular and sectoral. It is contraindicated in case of hemophthalmos (accumulation of blood in the eye), vitreous opacification. Preparation includes regional anesthesia or general anesthesia (in the secondary form of the disease).
The operation requires:
- silicone sponge;
- suture material;
- microsurgical scalpel;
- powerful lamp.
First, an incision is made, then the muscles are fixed and marking is carried out using the coagulation method. The filling is fixed with a mattress suture.
The most gentle method is laser coagulation
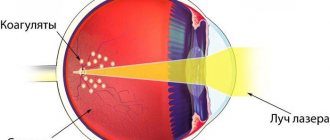
Patients ask whether it is possible to restore the retina with laser. Yes, laser coagulation is used.
This is a minimally invasive procedure. Indications: peripheral dystrophy and rhegmatogenous retinal detachment.
Contraindications include gliosis (layering of cells), clouding of eye structures, cataracts, and hemorrhages. The doctor installs the lens, focuses the rays and applies coagulates.
Pneumatic retinopexy using a gas bubble
During the procedure, the doctor introduces an air bubble into the eye, which causes the retina to be pressed and secretions to leak out. A laser or freezing device is then used to seal the gap.
Effective surgery: basic methods
At the moment, vitrectomy is considered to be the most modern method. This is an operation that involves introducing a special substance into the eye cavity. This may be a gas or oil that helps the retina adhere tightly.
There are other techniques, for example, scleral filling. The layers of the retina are brought together, squeezing the sclera from the outside. The compression area ensures the adhesion of the choroid and the retina. During the operation it is also possible to eliminate the gap.
After the main stage of the operation, other techniques can be used (most often laser coagulation is used) to secure the retina. Basic requirements for treatment: control at all stages, dynamic observation before and after surgery.
The type of surgery is chosen based on the condition of the eyes. It is important to assess the extent of damage and calculate possible risks. Thus, the presence of chronic retinal diseases greatly narrows the list of available treatment methods. Timely treatment can prevent vision loss and restore retinal function sufficient for normal life.
Treatment
All methods of treating retinal detachments are divided into three large groups: sparing, endovitreal and episcleral.
The first include cryopexy and laser coagulation of the retina. They are used to treat retinopathy, ruptures and subclinical retinal detachments.
The video below is an example of vitreoretinal surgery:
Endovitreal techniques include vitrectomy followed by the injection of liquid silicone or special gas. Of the extrascleral techniques, extrascleral filling (sectoral, radial, cerclage) and scleral ballooning are most often used.
Prognosis and prevention of retinal detachment
The prognosis depends primarily on the speed (that is, timeliness) of assistance. It is best to contact immediately at the first symptoms. The prognosis is also assessed by the condition of the vitreous body, the degree of damage, and the shape and location of retinal tears. The recovery prognosis is more favorable for those whose retina is not damaged in the central zone.
After the operation, the patient is recommended to undergo medical observation by an ophthalmologist; it is necessary, if possible, to avoid injuries and heavy physical exertion.
Prevention of retinal detachment involves maintaining visual hygiene. Even if a retinal detachment occurs, people with healthy eyes are more likely to recover. It is important to consult an ophthalmologist in time. If there are risk factors (for example, a history of chronic eye diseases), it is necessary to attend regular preventive examinations. Retinal detachment can be noticed early and prevented with painless and quick laser surgery. Similar operations are performed at CELT.
It is important to remember that pregnant women have an increased risk of retinal detachment during childbirth, especially if they have risk factors. In some cases, an ophthalmologist may recommend preventive laser treatment. Therefore, pregnant women need to contact an ophthalmologist for examination several times during pregnancy.
Those who have been identified as having a predisposition should give up contact sports that pose a risk of injury, avoid heavy lifting and intense stress, and monitor vascular health.
The CELT Clinic offers consultations and treatment with ophthalmologists with extensive clinical experience. Practicing qualified specialists will help you preserve your vision.
Primary retinal detachment
Primary retinal detachment occurs in approximately 1 case per 10,000 population and, without treatment, leads to blindness of the eye. Predisposing factors may be degenerative ischemic changes in the periphery of the retina, especially in combination with eye stretching in axial myopia, wrinkling of the vitreous body, and hereditary weakening of the connection between the pigment epithelium and the layer of rods and cones. O. s. can occur as a result of indirect trauma (falls, head injuries, sudden lifting of heavy objects, body concussion); at the same time the development of O. s. promotes rupture of the retina with subsequent penetration of fluid under it.
With O. s. Subjective sensations of photopsia arise in the form of sparks, lightning, curvature, vibrations of objects, a dark curtain appears in the field of vision, progressive limitation of the field of view and a sharp decrease in objective vision. There is a symptomatic difference in visual acuity and visual field in the morning and evening hours, the edges are explained by the displacement and partial resorption of subretinal fluid during sleep.
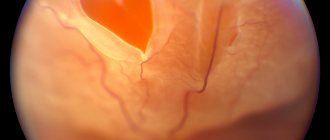
Ophthalmoscopically, the reflex from the fundus becomes gray, retinal folds are detected; due to swelling and loss of transparency of the retina, its vessels look dark; When the eye moves, the retina oscillates.
With difficult ophthalmoscopy in the diagnosis of O. s. Ultrasound echography helps (see Ultrasound diagnostics).
A simple diagnostic technique is to study the preservation of the mechanophosphene phenomenon. When pressing through the eyelids on the sclera with a glass rod, departing from the limbus by 12-14 mm, the patient normally notes the appearance of a dark spot with a light rim (the result of mechanical irritation of the retina). When pressing on the sclera at the site of the detached retina, this phenomenon is not observed or the spot becomes blurry. In addition, the patient feels a “shaking” or “vibration” in front of the eye during pressure. With O. s. There is also no such entoptic effect as autoophthalmoscopy, or the phenomenon of the retinal vascular Purkinje tree (the subject sees the vessels of his own retina during transscleral transillumination with a diaphanoscope or electric ophthalmoscope).
After the diagnosis of primary O. s. it is necessary to establish the localization of retinal breaks. Finding gaps is carried out mainly before surgery using reverse or direct ophthalmoscopy, biomicroscopy with a Goldmann lens when examining the extreme periphery of the retina with a maximally dilated pupil.
Retinal detachment in the fundus follows a certain pattern. Fluid from the vitreous body, penetrating through a retinal tear, first causes its detachment in the area of the break, then spreads to the dentate line and, falling (in the upper position of the break) downward due to gravity, flows around the optic nerve disk and ends up on the opposite half of the fundus. The level of retinal detachment almost always depends on the location of the break. The configuration of the detached retina, breaks and other changes in the fundus of the eye are plotted on a special diagram. There is an international color code for drawing the fundus.
Rice. 1. Schematic representation of determining the location of a retinal break during binocular ophthalmoscopy: 1 - probe for indentation of the sclera, 2 - site of a retinal break, 3 - lens.
The direct method of establishing the localization of a retinal tear during surgery is increasingly being used by pressing the membranes of the eye against the tear with curved tweezers or a thick injection needle with a blunt end and simultaneously observing the site of local compression using an electric direct ophthalmoscope or an indirect binocular Skepens ophthalmoscope (Fig. 1).
The perimetric method of calculating the projection of retinal breaks onto the sclera, described in many manuals, is labor-intensive and not accurate enough.
Elimination of O. s. is achieved by causing adhesive inflammation around the break and bringing the detached retina closer to the choroid.
Rice. 2. Schematic representation of diathermocoagulation for retinal detachment: 1—probe for diathermocoagulation, 2—sclera, 3—coagulants, 4—detached retina.
Of the many ways to induce adhesive inflammation, the most commonly used are diathermocoagulation, cryopexy (see Cryosurgery, in ophthalmology), photocoagulation (see Photocoagulation of the eye) and laser coagulation (see Laser, in ophthalmology). Athermocoagulation in the classical form (thermo-cauterization according to Gonen) is a kind of electric welding of the retina with the choroid through the sclera with a high-frequency current (Fig. 2). At the site of the rupture, through cauterization is performed with a needle electrode. Subretinal fluid flows out through the resulting microhole, the retina is adjacent to the choroid and is fixed as a result of the development of adhesive inflammation, and then the resulting scar.
In modern ophthalmic practice, a more gentle method is used - cryopexy with special tips cooled with carbon dioxide or liquid nitrogen. Subretinal fluid is usually not released. The degree of freezing is monitored ophthalmoscopically by the formation of a white spot.
Rice. 3. View of the fundus after laser coagulation performed for a retinal tear with a flat retinal detachment: the arrow indicates an atrophic rounded lesion at the site of the retinal break.
Photocoagulation and laser coagulation as independent methods of treatment are used for peripheral and central retinal tears with flat retinal detachment. The rupture is delimited by one or two rows of coagulants. The sufficiency of the dosage is determined by the appearance of a whitish cotton wool-like lesion without hemorrhages (Fig. 3).
When O. with., the edges do not fit completely after using the above methods, the membranes are brought together by pressing the sclera with fillings made of autotissue (ear cartilage, a piece of Achilles tendon, intussusception of the own sclera), homotissue (cadaveric preserved sclera and dura mater, catgut ), silicone rubber or silicone rubber sponge. Fillings that are 3-4 mm larger than the gap are pressed extrascleralally using U-shaped sutures or by inserting them into a pocket of dissected sclera and then suturing the edges of the pocket.
Rice. 4. Schematic representation of some stages of cerclage: a— application of the cerclage element and filling; b— eye after tightening and fixing the cerclage element with sutures; 1—cerclage tape applied under the rectus muscles of the eye; 2—seal on the sclera, 3—sutures.
In case of pronounced traction changes in the vitreous body, weak straightening of the retina after bed rest, or multiple ruptures, circular depression of the membranes is used at the level of the ruptures with a thread, polyethylene tube or silicone tape - the Arruga operation, or cerclage (Fig. 4). Cerclage is often combined with placing a filling under the thread or tape in the area of the ruptures. Subretinal fluid is usually released before the circular suture is tightened through a puncture of the sclera with a diathermocoagulator needle electrode.
There are methods of treating OS, in which the retina is brought closer to the choroid using various implants inserted into the vitreous body (endovitreal). For these purposes, sterile air, silicone liquid, luronite, nylon loops, and latex bubbles are used. Endovitreal injection of implants is often an addition to conventional scleroplastic operations, but sometimes it is used as an independent method, for example, the introduction of silicone fluid when the vitreous body shrinks and the retina tightens in the form of a funnel, with giant tears with inversion of their central edge.
Surgical treatment requires the patient to stay in the hospital for 1-3 weeks, including 2-6 days of bed rest in the postoperative period using a binocular bandage.
Patients with ruptures or defects of the retina, which pose a potential danger of O.'s occurrence, are subject to preventive treatment. These include valvular “silent” ruptures, as well as perforated ruptures, combined with photopsies. If O. s. occurred in one eye, then the fundus of the second eye is carefully examined dynamically and when “silent” tears appear, preventive treatment is carried out, which consists of photo-, laser coagulation (or cryopexy) of the retina around the breaks in order to cause adhesive inflammation.
Our services in ophthalmology
The administration of CELT JSC regularly updates the price list posted on the clinic’s website. However, in order to avoid possible misunderstandings, we ask you to clarify the cost of services by phone: +7
| Service name | Price in rubles |
| Appointment with an ophthalmologist (primary) | 3 500 |
| Autofluorescence, examination of the fundus using a fundus camera | 4 000 |
| B - ultrasonic scanning method | 700 |
| Vitrectomy for complicated conditions | 115 000 — 145 000 |
All services
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions