The retina is a rather thin membrane of the eyeball, the thickness of which is 0.4 mm. It lines the inside of the eye and is located between the choroid and the vitreous substance. There are only two areas of attachment of the retina to the eye: along its serrated edge at the origin of the ciliary body and around the border of the optic nerve. As a result, the mechanisms of retinal detachment and rupture, as well as the formation of subretinal hemorrhages, become clear.
Structure
The retina is a multilayered membrane consisting of:
- photosensitive cells;
- pigment layer;
- choroid;
- nerve layer.
Useful video
Anatomy and physiology of the retina:
Photoreceptor apparatus
Presented by 2 types of light-sensitive cells:
- Sticks. A large number of cells capture weak light rays and provide a person with vision at dusk or at night.
- Cones. They are few in number because they are highly sensitive to daylight. Provides vision in good lighting conditions.
Macular area
The sweet spot, or macula, is the area with the highest concentration of light-sensitive cells. In this place, maximum human visual acuity is achieved. The area is located above the exit zone of the optic nerve.
Optic disc
Alternative name: optic nerve head. This is the outlet for the long processes of the nerve cells of the retina. There are no photosensitive cells in this area, so there is no vision in this area and is called a blind spot.
Blind spot
The diameter is up to 5 mm. It is the area where the optic nerve exits the retina. The cranial-brain pair is formed from 1.2 million nerve cell axons located throughout the surface of the retina. It is also the exit point for blood vessels that supply the retina with oxygen and nutrients.
Blood supply to the retina
Under the pigment layer is the choroid, consisting of choriocapillaris. These are small vessels that provide trophism and respiration of the nerve cells of the fundus. With capillary thrombosis, dystrophic-degenerative changes in the retina develop and its detachment begins.
Causes
The causes of retinal detachment, as mentioned above, may be the following factors:
The photo shows a schematic representation of the process of retinal detachment
- Head injury.
- Eye injury.
- Myopia.
- Strong physical activity.
- Changes in the choroid.
- Modifications in the vitreous body.
- Untreated inflammatory processes of the eye;
Everything you need to know about receptors
Association neurons in the brain and spinal cord collect and translate information from sensory neurons. A sensitive neuron receives any stimulation and converts it into nerve impulses, which ensure the transmission of information to the central nervous system and executive organs. From all parts of the body, impulses arrive at the spinal cord and, passing through it, end their path in the cerebral cortex. Information passes through neurons in the form of a weak electrical signal. This is what is meant by the term “nerve impulse”.
When it reaches the junction of one neuron with another, a fluid is released - a neurotransmitter. If a sufficient amount of this substance is released in the next neuron, the impulse moves on.
Treatment of retinal detachment
Source: mediest.ru
Retinal detachment is considered a dangerous disease of the retina. It is important to remember that with such a diagnosis, the patient can only be cured through surgery, and no medications or folk remedies can eliminate such a disease.
Any self-medication will only lead to the loss of precious time, because detachment is considered fresh only in the first few months after its appearance. If pathology is detected at such a time, the chances that vision will be fully restored after treatment increase.
In a situation where it is possible to diagnose an old retinal detachment, surgical intervention is much more difficult for both the doctor and the patient.
Long-term retinal detachment results in the death of a large number of light-sensitive cells and this creates certain difficulties in restoring vision.
Drug treatment is used as an adjunct to surgical treatment. For eye injuries, fibrinolysis inhibitors are used to stop intraocular bleeding. Drugs to improve cellular nutrition and vitamin complexes are also prescribed.
Conservative methods of treating detachment are not effective. The main way to preserve vision is to undergo surgery.
Delaying or ignoring the symptoms of the disease can lead to complications: atrophy of the eyeball, persistent decrease in pressure, secondary cataracts and blindness. During the operation, the attending physician reduces the distance between the light-sensitive cells and the pigment epithelium.
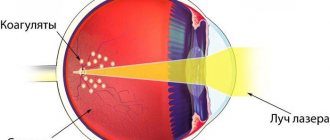
Adhesions are created in the area of the rupture. This allows you to normalize vision. The cost of treatment depends on the type of surgery. The most commonly performed eye surgeries are:
- laser therapy;
- scleroplasty;
- extrascleral filling;
- ballooning;
- vitrectomy;
- vitreoretinal intervention;
- cryocoagulation.
Laser coagulation of the retina also refers to surgical methods, but has its own characteristics. This is an outpatient operation that does not require a long rehabilitation period.
It is carried out in the ophthalmology office of the clinic. It is used independently for small detachments, and in addition to operations for better fusion of the retina with the underlying layers.
Treatment of this retinal disease is carried out using the following groups of operations:
- extrascleral interventions are performed on the surface of the sclera;
- endovitreal interventions are performed inside the eyeball.
Even after a successful operation, a person needs to visit an ophthalmologist twice a year and undergo a thorough examination of all blocked retinal tears.
In addition, such patients are advised to undergo courses of conservative therapy, which combines the use of retinoprotective, metabolic and vitamin tissue preparations.
After eye surgery, the patient will have to avoid any physical activity on the body and heavy lifting. The prognosis of developed retinal detachment will depend on the duration of the disease and the timeliness of treatment.
When retinal disease is diagnosed at the very beginning of its development during surgery, the outcome is usually favorable. It is possible to prevent the disease in people by following preventive measures and timely contacting a specialist when the first signs of retinal detachment appear.
The size of the detachment increases over time, leading to further deterioration of vision. Therefore, if symptoms appear, it is better to immediately consult a specialist. If the detachment has already occurred, only surgical treatment is possible.
And the faster it is carried out, the greater the chance of preserving the viability of the retinal cells, and therefore its functionality.
The most common retinal diseases
In most cases, the retina is susceptible to the development of the following diseases:
- degenerative-dystrophic changes;
- damage to the choriocapillaris;
- development of tumors.
Dystrophies
The pathological process is a gradual depletion and death of neurosensitive cells on the retina. At the same time, visual acuity deteriorates until complete blindness occurs.
Dystrophic disorders in most cases are associated with insufficient blood supply to the retina or the presence of hereditary diseases of the visual organs. In some cases, endocrine disorders such as diabetes mellitus can trigger the pathological process.
Retinal diseases
The visual organs, including the retina, are affected by multiple diseases. The causes are hereditary and acquired factors.
Retinal detachment
A pathological process in which the retina is separated from the choroid. Under the influence of trauma, intraocular tumors or dystrophic changes, the retina ruptures. As a result of this rupture, fluid from the vitreous body penetrates under the retina, which provokes a detachment.
Symptoms of the disease:
- Veil before the eyes;
- The appearance of luminous points, sparks;
- Distortion of images, objects;
- Entire areas disappear from view.
Detachment is characterized by the death of nerve cells. The longer the process lasts, the less hope there is for recovery even after a successful operation.
The success of therapy depends on timely detected pathology.
Surgery is the only way to preserve and restore vision. Detachment cannot be treated with medication.
Detachment can be caused by myopia or degeneration of the retinal layer. In this case, the best way is prevention - regular examination by an ophthalmologist and prescribed treatment measures.
Cone dystrophy
A hereditary disorder in which the suppression and death of cones—conical photoreceptors that convert light stimuli into a nerve signal—occurs.
Symptoms:
- Decreased visual acuity at any age;
- Increased sensitivity to bright light;
- Impaired color rendering, poor color perception.
The disorder can be primary and develop as a result of other ophthalmological diseases. In this case, the outer nuclear layer of photoreceptors practically disappears, and changes also occur in the pigment layer.
The best test in diagnosing dystrophy is considered to be electroretinography, a method based on the study of the biopotentials of the retina during light stimulation.
The consumption of omega-3 fatty acids, beta-carotenoids, and lutein can slow down the progression of dystrophy, but not cure the disease. Foods with a low glycemic index are recommended.
Retinitis pigmentosa
A degenerative hereditary disease characterized by severe deterioration of visual acuity and possible development of blindness. Symptoms can be observed already in childhood.
This is one of the forms of retinal dystrophy caused by the abnormal structure of photoreceptors or the pigment layer. With the disease, a person does not adapt well to light or darkness, and they may lose peripheral or central vision.
Other symptoms:
- Lack of clarity and contrast;
- Unclear color vision;
- Constant eye fatigue.
Retinitis pigmentosa can reduce visual acuity both from the edge to the center and from the center to the periphery. Vision loss is progressing.
The process can be slowed down by taking the right vitamin supplements, including vitamin A.
Future treatment includes the possibility of retinal implantation.
Macular degeneration
This is a group of diseases that affect the retina and affect the quality of central vision. The development of pathology lies in vascular disorders and lack of nutrition of the retina in the central zone. As a result of macular degeneration, blindness develops.
Risk factors are heredity and old age.
The body's vulnerability is increased by a lack of vitamins with antioxidant properties, zinc, and pigments. For prevention, it is recommended to eat a diet with sufficient amounts of fatty acids, as well as avoidance of foods with a high glycemic index. Researchers also associate the development of macular degeneration with the presence of cytomegalovirus in the body.
Symptoms:
- Feeling of fog before the eyes;
- Difficulty reading;
- Difficulty recognizing the face of a person standing close to you;
- Distorted perception of straight lines.
The specially created drug ranibizumab is used for treatment. It is intended for introduction into the eye cavity, suppressing the growth of modified vessels. Despite the effectiveness of treatment, the disease may recur.
Retinoblastoma
A malignant tumor in the development of which tissue of embryonic origin plays a major role. Develops mainly in children. Most often, a mutant gene is found in the genetic code. Heredity is to blame for the development of bilateral retinoblastoma.
Ultrasound, CT, and MRI are used for diagnosis. The priority in treatment is to preserve life, secondly - the organ, thirdly - visual functions.
For retinal diseases, patients are offered a wide diagnostic program. In addition to determining visual acuity, color perception and contrast sensitivity, patients are photographed with fundus photographs, loss of visual fields are detected, and vascular changes in the retina are assessed. Timely examination and treatment in the early stages can completely get rid of the disease or maintain optimal eye health.
How many neurons does the visual pathway consist of? Where are the subcortical and cortical vision centers located?
The visual pathway consists of the bodies of 4 neurons and their processes.
- Axons of I and II neurons (short) together with their bodies are located in the retina.
- Axons of III neurons form the optic nerve: Eyeball => optic canal => cranial cavity => partial optic chiasm (between two nerves) => an optic tract is formed at the base of the skull, heading to the subcortical centers of vision.
- The bodies of IV neurons are in the subcortical centers of vision: lateral geniculate bodies,
- superior colliculus,
- the posterior nuclei of the thalamus are in the thalamic cushion.
- Axons of IV neurons form the central visual pathway. It goes through the posterior 1/3 of the posterior limb of the internal capsule => the corona radiata is formed. It goes to the cortical center (along the banks of the calcarine groove).
Vascular pathologies
Vascular diseases of the retina are associated with damage to the choriocapillaris and blockage of blood flow by thromboembolism.
Diabetic retinopathy
Expert opinion
Kim Oksana Alexandrovna
Head of the ophthalmology clinic. Ophthalmologist with more than 10 years of experience.
The pathology occurs in patients who have suffered from diabetes mellitus for a long time and do not correct the level of glucose in the body. Hyperglycemia in the blood plasma disrupts the permeability and density of the walls of the choriocapillaris. As a result, they can rupture, causing hemorrhages into the vitreous cavity. As a compensatory mechanism, the formation of new vessels that grow through the retina begins. But during this period, photosensitive cells become cut off from the supply of oxygen and nutrients. As a result, dystrophic changes develop in the nervous tissue.
There are 3 stages of development of the pathological process:
Useful video
The retina is a complex organ, despite its small size. In addition to the 10 layers in the structure of the visual organ, it contains nerve fibers for various purposes. Retinal diseases are not accompanied by pain, which emphasizes the need for routine visits to the ophthalmologist. The most complex pathologies of the organ are atrophy, macular degeneration and detachment. When such diseases are complicated, complete and irreversible loss of vision is possible.
Author's rating
Author of the article
Alexandrova O.M.
Articles written
2031
about the author
Was the article helpful?
Rate the material on a five-point scale!
( 3 ratings, average: 5.00 out of 5)
If you have any questions or want to share your opinion or experience, write a comment below.
Task No. 6
Monitor the work of the lens.
- Holding the sheet at a distance of 15 cm from your eyes, so that the letters are clearly visible, and the board with the text is visible through the hole, close one eye.
Assignment: Read the writing on the board and answer the question: Why do the letters surrounding the hole appear blurry when reading?
(The lens becomes flatter when we look at a distant object, and near objects, projected on the retina, are out of focus.)
(The letters are clearly visible, but the writing on the board is blurry.)
- What conclusion can be drawn?
Group 4: light-perceiving system.
Methods for diagnosing diseases
To diagnose the cause of decreased visual acuity, the ophthalmologist examines the fundus of the eye using a slit lamp and a mirror ophthalmoscope. For convenience, the pupil is forcibly dilated with Irifrin.
More accurate and highly informative instrumental studies allow us to assess the condition of intraocular structures:
- Echoscopy. It is a type of ultrasound diagnostics. The procedure allows you to determine the condition of the optic nerve head and will show the vitreous body. Using this method, we can tell whether there are areas of retinal detachment, areas of retinal thickening and inflammation.
- Optical coherence tomography (OCT). The diagnostic procedure is based on the use of infrared radiation. Modern devices make it possible to assess the condition of all layers of the retina separately. Thanks to this approach, it is possible to accurately determine the location of degenerative changes.
- Fluorescein angiography. Before the procedure, the patient is injected intravenously with a contrast agent. After 1-2 minutes, the medicine will reach the central retinal artery. At this time, several photographs of the fundus are taken. The procedure determines the patency of blood flow, eliminates the risk of thrombosis or shows the location of blockage of blood vessels.
Symptoms
Old age and high degrees of myopia, people undergoing eye surgery, and hypertension are the main risk groups for retinal detachment. Emerging symptoms in the early stages will allow you to urgently respond to the pathology and promptly prevent vision loss.
Signs of retinal detachment:
- Light shadows, flashes, glare, lightning and spots occur at the very beginning of the peeling process.
- Trembling and blurring of the boundaries of objects, curvature of outlines, oscillation of objects when examining them.
- Flickering of flies before the eyes, which interferes with concentration. The symptom does not disappear even after proper rest and sleep.
- A black line or spot forms in the eyes; this is the visible area of detachment. This symptom tends to grow until the field of vision is completely narrowed.
- When reading, individual letters or sections of the text being read fall out of the visual field.
- Partial or complete loss of lateral vision.
- A progressive decline in visual acuity, blindness can occur in just a few hours.
Important point! If a veil appears in your eyes, you need to concentrate and understand from which side it spread. It is important for the doctor to know about the source of the pathological process - it started from the center or began from the edges of the retina.
Cones
The coordinated work of rods and cones, despite the fact that their structure differs significantly, helps a person to see the entire surrounding reality in full qualitative volume. Both types of retinal photoreceptors complement each other in their work, this helps to obtain the most clear, clear and bright image possible.
Cones get their name because their shape is similar to the flasks used in various laboratories. The adult retina contains about 7 million cones. One cone, like a rod, consists of four elements.
Iodopsin is divided into several types, which allows for full sensitivity of the cones of the visual pathway when perceiving different parts of the light spectrum.
Based on the dominance of different types of pigment elements, all cones can be divided into three types. All these types of cones work in concert, and this allows a person with normal vision to appreciate the richness of the shades of the objects he sees.
Layers of the retina
The visual area of the retina has a layered structure.
It is possible to recognize 10 thin layers only with the help of a microscope. Each layer has its own purpose.
Pigmentary
Consists of epithelial cells containing pigment. Designed to provide nutrients to photosensitive sensors. Most tightly connected to the choroid.
Layer functions:
- Absorbs light, promotes contrast and clarity of visible images;
- Recycles waste membrane disks of photoreceptors, ensures phagocytosis;
- Stores vitamin A, necessary for the quality of vision;
- It is an intermediate point for the delivery of nutrients from the choroid and the removal of decay products in the opposite direction;
- Removes water from the intercellular space, normalizes osmotic pressure;
- Normalizes the temperature in adjacent tissues.
Photosensory
Consists of outer and inner segments of photoreceptor cells. Most metabolic reactions occur in the internal one. The segments are connected to each other by a thin cilium, through which substances are transported in the direction from internal to external.
External limiting membrane
Designed to maintain the structure of the retina. Under a microscope it looks like a border plate with cones and rods breaking through it.
External granular
Contains the largest number of cell nuclei. The peripheral processes, rods and cones, are located parallel to each other. In this case, the cores of the sticks are placed in layers, in 6-8 layers.
External plexus-shaped
It is formed by synapses - the point of contact between photoreceptors and bipolar cells. Contains a network of retinal capillaries. The vessels are located strictly on the surface of this layer, without penetrating into other layers.
Internal grainy
The nuclei of the cells contained in this layer, when viewed under a microscope, have a granular-looking structure. The cells decipher nerve impulses coming from other layers and ensure the normal functioning of the nervous tissue of the retina.
Internal plexus-shaped
Formed by intertwining cell endings. The last stage of processing the received information before transmitting it to the brain's visual centers.
Ganglion cell
A retinal neuron adapted to generate nerve impulses in the retina. The layer of ganglion cells is adjacent to the vitreous body of the eye, so light hits it first. These cells collect information along vertical and horizontal pathways from all layers of the retina. It is on them that a person’s visual acuity and color perception depend.
Nerve fiber layer
The layer acts as a conductor of information received from photoreceptors to the central parts of the brain. The nerve fibers in the layer do not have a myelin sheath and only after leaving the organ of vision are covered with a protective myelin layer. Damage to the layer means irreversible changes in vision and is characteristic of diseases such as glaucoma.
Internal limiting membrane
It is formed by the membranes of Müller cells - auxiliary nerve cells. The layer contains complex proteins and collagen fibers. In appearance, the layer is quite homogeneous and serves as a kind of boundary between the retina and the vitreous body. The membrane is connected to the retina by an intermediate layer consisting of an adhesive substance.
Ionotropic channels
Another type of cellular receptors are ionotropic channels located in the membrane that can open or be blocked under the influence of signaling chemicals, for example, H-cholinergic receptors, vasopressin and insulin receptors.
Intracellular sensing structures include transcription factors that bind to the ligand and then enter the nucleus. Their connections with DNA are formed, which enhance or inhibit the transcription of one or more genes. Thus, the main functions of cell receptors are the perception of signals from the external environment and the regulation of plastic metabolic reactions.
Mediators
These are biologically active substances that transmit excitation from one neuron to another in special structures - synapses. They are secreted by the axon of the first neurocyte and, acting as a stimulus, cause nerve impulses in the receptor endings of the next nerve cell. Therefore, the structure and functions of mediators and receptors are closely interrelated. Moreover, some neurocytes are capable of secreting two or more transmitters, for example, glutamic and aspartic acids, adrenaline and GABA.
Sensory hearing system
With age, hearing acuity decreases. The human ears consist of 2 sensory organs: hearing and balance.
The organ of Corti is part of the receptor apparatus of the internal structure of the ear. The function of the receptors is to receive sound stimuli from the external environment. Auditory cells are mechanoreceptors of the secondary sense. They are divided into internal and external. The internal ones come in one row in the amount of 3500 pieces, the second ones are 5 times larger in number. The hairs transmit mechanical vibrations to neighboring receptors, which increases the sensitivity of each cell.
Symptoms of retinal pathology
With congenital retinal pathology, the following signs of the disease may be present:
- Albiotonic fundus.
- Retinal coloboma.
- Myelin fibers of the retina.
Acquired changes in the retina include:
- Retinoschisis.
- Retinitis.
- Retinal detachment.
- Disruption of blood flow through the arteries and veins of the retina.
- Retinopathy caused by systemic pathology (diabetes mellitus, blood diseases, hypertension, etc.).
- Berlin's opacification of the retina due to traumatic injury.
- Phakomatoses.
- Focal retinal pigmentation.
When the retina is damaged, there is most often a decrease in visual function. If the central zone is affected, then vision is especially affected and its impairment can lead to complete central blindness. At the same time, peripheral vision is preserved, so a person can navigate in space. If, with a retinal disease, only the peripheral area is affected, then the pathology can be asymptomatic for a long time. This disease is often detected during an ophthalmological examination (peripheral vision test). If the area of damage to peripheral vision is extensive, then there is a defect in the visual field, that is, some areas become blind. In addition, the ability to navigate in space in low light conditions decreases, and in some cases color perception changes.
How cells perceive stimuli
Their membranes (or cytosol) contain special molecules consisting of proteins, as well as complex complexes - glycoproteins. Under the influence of environmental factors, these substances change their spatial configuration, which serves as a signal for the cell itself and forces it to respond adequately.
Some chemical substances, called ligands, can act on the sensory processes of the cell, as a result of which transmembrane ion currents arise in it. Plasma membrane proteins, which have receptive properties, together with carbohydrate molecules (i.e., receptors) perform the functions of antennas - they perceive and differentiate ligands.
The mystery of smell
Just like the taste, the olfactory analyzer reacts with its nerve endings to molecules of various chemical substances. The very mechanism by which odorous compounds irritate the olfactory bulbs has not yet been fully studied. Scientists suggest that odor signaling molecules interact with various sensory neurons in the nasal mucosa. Other researchers associate irritation of olfactory receptors with the fact that signaling molecules have common functional groups (for example, aldehyde or phenolic) with substances included in the sensory neuron.
The functions of the olfactory receptor are to perceive irritation, differentiate it and translate it into the process of excitation. The total number of olfactory bulbs in the mucous membrane of the nasal cavity reaches 60 million, and each of them is equipped with a large number of cilia, thanks to which the total area of contact of the receptor field with molecules of chemical substances - odors - increases.