Glaucoma is an eye disease associated with increased intraocular pressure and the slow destruction of the retina and optic nerve. The patient's visual acuity decreases, and visual fields also fall out. If left untreated, the pathology can lead to blindness. The disease can affect one or both eyes at once, and, having developed in one eye, in the absence of medical measures it also occurs in the second. Glaucoma is considered a disease of older people, as it is mainly diagnosed in patients over 60 years of age. However, the pathology can develop at any age; it can also be congenital in children.
In this article we will explain what glaucoma is in simple words. You will learn about the mechanism of its development, symptoms, and preventive measures. You will receive a consultation with an ophthalmologist, and if the need arises, you will receive treatment at the Otradnoe Polyclinic. Make an appointment at a time convenient for you by calling the phone number listed on the website.
Glaucoma - what kind of disease is it?
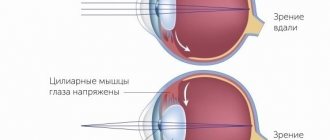
To understand this, you need to understand the structure of the eye. It is shaped like a ball, hence the name - eyeball. This ball consists of many layers, each of which performs its own important function. Visual acuity and overall eye health depend on the combination and coherence of functions.
The outer layer of the eye is called the conjunctiva, and underneath is a white film called the sclera. Its function is protective. The part of the sclera, in the center of the front surface of the eye, is convex and transparent. This is the cornea. It is responsible for ensuring light access into the eye and its refraction. The area connecting the sclera and the cornea is called the limbus, where stem cells are located, thanks to which the outer layers of the cornea are regularly renewed.
The next layer behind the sclera is the choroid. It consists of three sections and is responsible for the blood supply to all ocular structures, as well as for ocular tone. The parts of the choroid include:
- Iris;
- choroid - vascular system;
- ciliary body - responsible for the production of intraocular fluid, which fills the chambers of the eye.
There are two chambers in the eye. The anterior one is located between the cornea and the iris. Its peripheral part is called the anterior chamber angle. The posterior chamber is located between the vitreous humor and the back of the iris. Through the angle of the anterior chamber, where the drainage system is located, the outflow of intraocular fluid occurs. The intraocular fluid is responsible for nourishing the anterior part of the vitreous body, the lens and other structures that do not have blood vessels. It also normalizes intraocular pressure.
The layer next to the choroid is the retina. It consists of nerve cells. It displays images, and the optic nerve carries information about them to the brain. That is, our vision is the “merit” of the retina. Under all the above membranes are the vitreous body and the lens.
Glaucoma occurs due to impaired outflow of intraocular fluid. Due to this failure, the eye chambers become overcrowded, the pressure in the eye increases, which negatively affects the vessels of the optic nerve. They become pinched, which impedes the flow of blood to the optic nerve and disrupts its nutrition. If this continues regularly, the nerve may atrophy. In addition, the transmission of nerve impulses to the brain deteriorates - vision is impaired, and over time blindness may develop.
There are two main forms of the disease (based on the nature of the fluid outflow failure):
- Open-angle glaucoma (90% of cases).
- Angle-closure glaucoma.
With an open-angle form, the quality of operation of the ocular drainage system decreases, but access to it is not blocked. With this type of disease, symptoms may not appear for several years. And then the person realizes that vision has deteriorated or disappeared in one eye. Other patients have the following signs of open-angle glaucoma: the presence of halos around light sources (if you look at them), a slight veil before the eyes.
In the closed-angle form, access to the drainage system of the eye is blocked by the iris. This type of disease is characterized by acute attacks. Intraocular pressure increases sharply, causing pain in the eye and the corresponding half of the head. These symptoms are accompanied by disturbances in vision: it may become blurred or disappear completely. As with the open-angle form, the patient observes halos around light sources.
Reference! There is another form of the disease - normotensive glaucoma. It is distinguished by the absence of an increase in intraocular pressure. In this case, the optic nerve is destroyed and the visual fields are lost. It is believed that the pathology develops with special sensitivity of the optic nerve and circulatory failure. This form is usually characteristic of patients with low blood pressure.
Glaucoma treatment
Modern ophthalmological practice has 3 methods of treating glaucoma: medication, laser and surgery.
Drug (conservative) treatment of glaucoma
It is based on reducing intraocular pressure and improving blood supply to the organs of vision. An important task for the doctor is to normalize metabolic processes in the eye tissues. For this purpose, 3 types of medications are used:
- improving the outflow of intraocular fluid;
- inhibiting (suppressing) the secretion of intraocular fluid;
- combined (cosopt, fotil, normoglaucon, etc.).
Laser treatment of glaucoma
Laser iridotomy
In some people, the drainage zone is narrowed due to anatomical features, which leads to fluid retention and increased pressure. The laser iridotomy procedure involves creating an additional hole in the periphery of the iris (near the root) to improve the circulation of intraocular fluid in this drainage area. The ultimate goal is to control normal intraocular pressure. Artificial holes are extremely small (0.5 mm) and cosmetically invisible. They remain for life and do not cause discomfort.
Selective laser trabeculoplasty (SLT)
A new level in ophthalmology, the use of a laser to apply laser applications, due to which intraocular pressure is reduced in the same way as with medication. It is characterized by absolute harmlessness and the absence of a traumatic factor. It does not have a thermal effect on surrounding tissues and does not cause changes in their structure. The experience of leading ophthalmologists has proven the effectiveness of the SLT technique even when performing repeated surgery on the trabecula, which is not possible when using other laser techniques.
It is carried out on an outpatient basis, under local anesthesia with pain-relieving drops; after implementation, it is necessary to come to the hospital several times for a follow-up examination.
It must be understood that SLT cannot completely replace drug treatment or the necessary microsurgical intervention. This is impossible due to the variety of clinical scenarios for the development of glaucoma and its extremely complex pathogenesis.
Laser trabeculospasis
Improves the functioning of the drainage zone of the eye, normalizes IOP. By applying a dosed effect on the drainage area, its activation is achieved and the removal of fluid from the eye is facilitated.
Shallow penetrating laser sclerectomy (LPLS)
An operation in which the eyeball does not open. A special valve is created in the inner lining of the eye to restore the balance of intraocular fluid. The procedure requires the highest precision as it is carried out manually.
Often all of the above laser treatment methods are combined to achieve maximum effect.
Glaucoma surgery
The so-called penetrating surgical methods include trabeculotomy and trabeculectomy. During penetrating operations on the trabecular mesh area, part of the trabeculae is surgically removed to create a channel for the removal of aqueous humor. These types of procedures may require hospitalization. After operations, there are some restrictions on the patient’s physical activity; stress should be avoided.
Separately, it is worth highlighting operations using microdrainage Ex-PRESS (Excessive Pressure Regulation Shunt System). This is a relatively new technique that involves implanting a special metal device inside the eye. The technique is quite simple to perform, gentle, and has a minimum of postoperative complications.
The success of surgical treatment depends on the type and stage of glaucoma, accompanying circumstances (cataracts), the experience of the surgeon and the general condition of the patient. Different types of glaucoma require different surgical techniques.
An analysis of modern world medical practice clearly demonstrates that preserving vision in glaucoma is possible. Methods are already being used to slow the development of pathology, significantly delaying the threshold of complete loss of vision. But, as mentioned above, the following are critically important for this: timely diagnosis of glaucoma, professional treatment with accompanying careful monitoring, and patient compliance with all doctor’s recommendations.
Types and stages of development of glaucoma
The origin of the disease can be:
- Congenital - develops as a result of genetic disorders, intrauterine and birth injuries, failures in the development of eye structures, usually detected in children under 3 years of age.
- Primary – occurs due to age-related changes.
- Secondary – develops against the background of other eye or general pathologies, after operations and taking certain medications.
4 stages of glaucoma development:
- Initial – associated with a periodic increase in intraocular pressure, there are defects in the central field of vision, the boundaries of the visual field are not violated.
- Developed - lateral vision suffers, the field of vision as a whole narrows.
- Neglected – there is a significant narrowing of the field of view.
- Terminal – complete blindness or preservation of only sensitivity to light.
Types of glaucoma
This eye pathology is classified into congenital, juvenile, primary and secondary adult glaucoma.
Congenital glaucoma is detected in infancy. Causes: genetic predisposition, diseases during fetal development or injury during childbirth.
Juvenile glaucoma is diagnosed between 3 and 35 years of age. Usually it is determined by poor heredity or is concomitant with such systemic pathologies as Hippel-Lindau disease, Frank-Kamenetsky syndrome.
The primary form develops in mature and elderly people. Secondary glaucoma is called glaucoma that accompanies other eye diseases.
Experts, depending on the profile of the anterior chamber angle, distinguish several types of disease.
Open-angle glaucoma (OG)
Among residents of Russia, this form, according to statistics, is most common. The reason is high IOP, which appears as a result of disruption of the drainage system of the eye. If measures are not taken to reduce it, damage to the optic nerve occurs, narrowing of the boundaries of the visual field, and blindness.
Factors contributing to the development of this type of glaucoma are genetic predisposition, old age, diseases of the cardiovascular system, and diabetes. Open-angle glaucoma, according to experts, develops asymmetrically, affecting both eyes.
Stages of primary open-angle glaucoma
The initial, first, stage of OH does not affect peripheral vision. There are only minor changes in the paracentral region, and the process of excavation of the optic nerve has begun.
In the second, advanced stage of OH, peripheral vision becomes worse on the side of the nose or its concentric narrowing occurs.
For the third (so-called advanced) stage, the field of vision in one or several segments is greatly narrowed.
At the terminal (fourth) stage, vision is completely absent, or the person’s color perception is greatly distorted.
Angle-closure glaucoma (AC)
This type of glaucoma occurs in 25% of cases of identified pathology, and it is more often diagnosed in the fairer sex. Develops due to blocking the angle through which fluid flows out. Factors in the development of MH include structural features of the eye, excessive amounts of ocular fluid, etc.
The main symptom of MH is increased IOP. At first it occurs briefly, but gradually the duration of the attack increases.
As a result of a jump in IOP, an acute attack of glaucoma can occur. The cause of this condition is stress, overwork, etc. The patient may complain of headache, nausea, and a sharp decrease in vision. IOP can jump to 50-60 mmHg (with the norm being 21-27 mm). If a person does not receive immediate help, he may lose his sight forever.
Experts distinguish normotensive glaucoma, which is characterized by normal IOP. Atrophy of the optic nerve occurs due to its poor blood supply or hypersensitivity to normal pressure. Often people suffering from this form of the disease are hypotensive.
Causes of glaucoma development
For now, we can only say for sure that there is a hereditary predisposition to this pathology. The exact causes of glaucoma have not yet been determined. Possible causes include:
- aging processes of the body;
- endocrine and cardiovascular diseases;
- defects in the structure of the eye structures.
Glaucoma most often develops in people:
- with a significant degree of farsightedness or myopia (after 40 years);
- over 60 years of age (even with healthy eyes);
- with diagnosed diseases of the nervous, cardiovascular and endocrine systems;
- with hypotension (low blood pressure);
- undergoing long-term treatment with hormonal drugs;
- with increased intraocular pressure;
- with eye injuries and pathologies, as well as those who have undergone eye surgery.
Important! People at risk should visit an ophthalmologist regularly. Also, preventive visits are necessary for patients whose relatives suffer from glaucoma, since a genetic predisposition has been precisely proven.
Algorithms for examining patients with suspected glaucoma and glaucoma
NATIONAL GUIDE TO GLAUCOMA Edited by E.A. Egorova Yu.S. Astakhova A.G. Shchuko Authors and contents Moscow. 2008
The detection of increased intraocular pressure in the absence of characteristic changes in the ONH and in the state of the visual field does not allow a diagnosis of glaucoma. However, GON of the optic nerve can also occur at a normal level of intraocular pressure. During dynamic observation of the patient, a diagnosis of “ophthalmic hypertension” or “preglaucoma” is made. The diagnosis of “suspicious glaucoma” is not a clinical diagnosis and is made for the period of examination, which should not be extended over time. The decision to prescribe antihypertensive treatment for these diagnoses is made individually.
If glaucoma is suspected, the goal of diagnosis is to determine the presence or absence in the patient of signs of impaired hydrodynamics of the eye characteristic of glaucoma and the development of glaucomatous optic neuropathy and subsequent atrophy of the optic nerve head (with excavation), accompanied by characteristic functional changes in the form of typical visual field defects. As a rule, the diagnosis of “suspicious glaucoma” is made at the time of the examination, which should last no more than 1-1.5 months.
1. The presence of several of the following symptoms in a patient over 40 years of age (over 35 years of age if there are direct relatives suffering from primary glaucoma):
- The patient complains of discomfort, blurred vision;
- IOP is higher than tolerant, or there is IOP asymmetry in both eyes of 5 mm Hg. Art. and more;
- Field of vision suspicious in terms of the presence of early glaucomatous changes (scotomas in the central field of vision, in the Bjerrum zone, etc.);
- Changes in the optic disc, which can be considered as signs of incipient glaucoma, including:
- expansion of excavation of the optic disc, especially in its upper or lower sections, more than 0.5DD;
- asymmetry of optic disc excavation in two eyes;
- hemorrhage in the layer of nerve fibers along the edge of the optic disc;
- Biomicroscopic and gonioscopic changes characteristic of glaucoma:
- atrophic changes in the stroma of the iris and the pigment border of the pupil, their pronounced asymmetry in both eyes, elements of pseudoexfoliation;
- beak-shaped or narrow UPC; the presence of goniosynechia;
- intense pigmentation of trabeculae.
Risk factors for the development of glaucoma are:
- hereditary predisposition,
- age over 65 years,
- thin cornea (central thickness less than 520 µm),
- vertical E/D ratio is greater than 0.5,
- decrease in general sensitivity or the presence of specific scotomas in the Bjerum zone, expansion of the blind spot during examination on the computer perimeter.
The examination should also take into account the presence of other less significant risk factors - arterial hypertension, cardiovascular diseases, myopia, migraine and other vasospastic conditions, diabetes, and a tendency to arterial hypotension.
Criteria and signs that determine the diagnosis of ocular hypertension: The patient meets all of the following criteria:
- IOP is constantly above 25 mmHg. Art. (true IOP above 21 mm Hg) with repeated measurements on different days;
- IOP is symmetrical or IOP asymmetry in both eyes is no more than 2 - 3 mm Hg. Art.;
- absence of signs of glaucomatous optic neuropathy - characteristic changes in the visual field and/or optic disc;
- open CPC;
- the absence of established factors acting as possible causes of secondary glaucoma, for example, traumatic recession of the anterior chamber angle, lens subluxation, etc.
The purpose of diagnosis is to confirm the diagnosis of ocular hypertension, determine its causes, and exclude possible signs of primary or secondary glaucoma. The difficulties of early diagnosis of glaucoma are largely associated with the existence of benign ocular hypertension, which includes any non-glaucomatous increase in IOP that goes beyond generally accepted standards.
Mandatory conditions for ocular hypertension are an open anterior chamber angle and the absence of changes in the visual field and optic disc characteristic of glaucoma, not only during the first study, but also during long-term observation of the patient over several years.
Particular attention in cases of ocular hypertension (including more frequent examinations) should be given to patients with the presence of one or more features that are considered to be major risk factors for the development of glaucoma.
These factors include:
- IOP is above 28 mm Hg. Art. ;
- hereditary predisposition;
- age over 65 years;
- thin cornea (thickness in the center less than 520 microns);
- the vertical E/D ratio is greater than 0.5;
- presence of scotomas in the field of view;
- daily fluctuations in IOP more than 5 mm Hg. Art.
With regular monitoring, a number of patients develop symptoms of primary or secondary glaucoma. In the presence of pathology of the thyroid gland, pathological menopause, diencephalic syndrome, the necessary treatment is carried out by an endocrinologist and neurologist. In case of steroid hypertension, it is necessary to reduce the dosage of GCS or discontinue them, if possible. All medical services are provided on an outpatient basis.
Minimum required examination for ocular hypertension:
1. tonometry is carried out repeatedly during the initial diagnosis, with further observation at each follow-up examination by an ophthalmologist.
2. Tonography in the case of symptomatic or essential bilateral hypertension is performed once to confirm hypersecretion and the absence of disruption of the outflow of intraocular fluid in both eyes.
3. daily tonometry is performed on an outpatient basis for 3-5 days.
4 . stress tests to study IOP regulation are informative in the differential diagnosis of ocular hypertension and glaucoma (preglaucoma) [Volkov V.V. et al., 1985].
5. computer perimetry is performed during the initial consultation with an ophthalmologist; in the future, if necessary, reapply 1-2 times a year. Used for differential diagnosis of ophthalmic hypertension and glaucoma. In institutions that are not equipped with a computer perimeter, the central field of vision is examined using campimetry.
6. Keratopachymetry allows a more correct assessment of eye tonometry data. Tonometry data in eyes with a cornea with a central thickness of more than 570 km requires downward correction. Tonometric IOP 26-28 mm Hg. Art. in such eyes, in many cases it can be considered as a variant of the norm.
The frequency of repeat examinations is individual and depends on the cause of hypertension, the degree of increase in IOP and the presence or absence of risk factors for the development of glaucoma. For symptomatic or essential hypertension with a low level of IOP, it is necessary to conduct an examination once every 6 months, and for a long-term, stable course of more than 1 year - once a year. Patients with risk factors require examination once every 3 months.
Leading importance in the diagnosis of glaucoma is given to perimetry (optimally the use of computer static perimetry), studies of IOP and hydrodynamics of the eye (taking into account keratopachymetry data), and studies of the fundus (preferably using visualization methods).
In patients with glaucoma, the goal of diagnosis is to identify signs characteristic of OAG of impaired regulation of IOP and hydrodynamics, the state of the anterior chamber angle, the presence and severity of glaucomatous optic neuropathy, characteristic changes in the visual fields, and, based on the data obtained, to determine the form of glaucoma, its clinical stage , level of IOP compensation and process stability.
Examination for glaucoma should be comprehensive, not extended over time, and carried out as planned.
Diagnosis of OAG stages II-III - B-C does not require a large number of additional examinations, since at these stages there are manifest clinical signs of a developed and advanced glaucomatous process.
In cases of stage 1 OAG, there may be a need for further examination in highly qualified ophthalmological institutions or specialized glaucoma centers to clarify the diagnosis or carry out differential diagnosis with ocular hypertension of various etiologies. In such patients, as well as in patients with suspected glaucoma, along with traditional methods, it is necessary to use visualization methods of the RNFL and ONH, computer static perimetry and other highly sensitive diagnostic methods.
You can contact an ophthalmologist online: the doctor will answer any of your questions about the symptoms and treatment of glaucoma within an hour.
Symptoms
Signs of congenital glaucoma include:
- corneal clouding;
- increased photosensitivity of the eyes;
- enlargement of the eyeball;
- tearfulness;
- corneal edema.
Symptoms of acquired glaucoma:
- pain or a feeling of heaviness in the eyes and nearby areas;
- redness of the eyes;
- blurred vision, the patient sees a veil or grid before the eyes;
- feeling that the organs of vision are full of moisture;
- narrowing of the field of view;
- blurred vision at dusk or darkness;
- the appearance of halos around light sources.
In an acute attack of glaucoma the following are observed:
- sharp pain in the eye and corresponding part of the head;
- deterioration in general health;
- discomfort in the heart area;
- nausea and vomiting.
In case of an acute attack, you should immediately consult a doctor, as intraocular pressure should be urgently reduced. Without medical attention, complications may occur.
Advantages of glaucoma treatment at the clinic of JSC "Medicine"
Qualification – admission, treatment and surgical intervention are performed by qualified ophthalmologists of the highest category. Consultations are held with the participation of leading experts, professors, and academicians. Research and experimental work is carried out at the clinic, and advanced treatment methods are being introduced.
Technical support – JSC “Medicine” (clinic of academician Roitberg) is equipped with the latest generation diagnostic and treatment equipment. Thanks to this, diagnosis is carried out in the shortest possible time, and it is possible to achieve the most effective treatment results.
One of the key factors in effectively monitoring the dynamics of glaucoma treatment in a particular patient has become computer recording of the results of studies performed at all stages of treatment. This makes it possible to create an individual database (for each individual case), which greatly facilitates comparative analysis and increases its accuracy. After all, many indicators are taken into account, which, when combined, can serve as the basis for a correct prognosis, and therefore for choosing the right treatment tactics.
Remember: changes in glaucoma are irreversible, the sooner you see a doctor, the greater the percentage of vision you can save!
Diagnostics
To identify the disease, the following diagnostic tests are necessary:
- fundus examination;
- assessment of intraocular pressure;
- Ultrasound of the eye, Dopplerography (study of blood flow in the eye vessels);
- measurement of the thickness of the lens, anterior eye chamber;
- visual field examination;
- measurement of refraction (refractive power of the eye);
- gonioscopy – assessment of the condition of the anterior ocular chamber.
Diagnosis of glaucoma
Timely diagnosis and observation of glaucoma in the clinic is carried out using the following research methods:
- Dynamic contour tonometry (DTC) is an ultra-precise measurement of intraocular pressure with an ophthalmic tonometer. Tonometry can be performed using a device that is suitable for independent outpatient measurements. This makes daily tonometry possible, which greatly simplifies the choice of medications.
- Optical coherence tomography (OCT) – assesses the condition of the retina and optic nerve head, the most effective method in modern ophthalmology. The feasibility of its use has been confirmed in world ophthalmology. Scientific works of specialists clearly demonstrate that OCT is the leading technique in determining the initial form of glaucoma.
- Digital flicker perimetry is an innovative method of studying the visual field, the only one of its kind, which makes it possible to detect glaucomatous disorders in the preclinical period. Combined use in conjunction with Heidelberg retinotomography has made it possible to reach a new level of functional diagnostics, characterized by selectivity and hypersensitivity in determining glaucoma at an early stage.
- Ophthalmoplethysmography is a basic method for diagnosing blood supply, based on continuous monitoring of the volume of the eyeball.
- Ophthalmologists have confirmed in practice the decisive role of this study in monitoring the progression of glaucoma. It is thanks to this that a reliable forecast is possible.
- Tonography – determination of the movement of intraocular fluid and pressure with simultaneous graphic registration.
Glaucoma
How is glaucoma diagnosed?
An eye doctor (ophthalmologist) can identify people at risk of developing glaucoma (for example, due to a narrow filtering angle or increased intraocular pressure) before nerve damage occurs. The doctor also monitors patients with glaucoma.
Various painless tests can be used to detect glaucoma.
Tonometer
determines the pressure in the eye by measuring the hardness of its surface. After the eye is numbed with an ophthalmic anesthetic, the tonometer probe is placed against the front surface of the eye.
The stiffer the surface of the eye, the higher the pressure.
Measuring the thickness of the cornea
is a relatively new test used to manage glaucoma. This method determines the thickness of the cornea. After the eye is numbed, the tip of the thickness measuring device lightly touches the front surface of the eye (cornea).
Recent studies have shown that corneal thickness may influence intraocular pressure measurements. Thicker corneas may give falsely high eye pressure results, and thinner corneas may give falsely low eye pressure results.
Additionally, thin corneas may be an additional risk factor for glaucoma.
Gonioscope
placed in the anesthetized eye. A gonioscope is a special thick contact lens with mirrors. Mirrors allow the doctor to view the eyes from all sides. The purpose of this test is to examine the drainage angle and drainage area of the eye.
With this procedure, the doctor can determine whether the angle is open or narrow. As noted earlier, people with narrow angles have an increased risk of sudden angle closure, which can cause acute development of glaucoma.
The gonioscope can also determine whether anything, such as abnormal blood vessels, might be blocking the drainage of aqueous humor.
Ophthalmoscopy
– an examination in which the doctor uses a handheld device to look directly through an opening in the colored iris of the eye. This procedure is done to examine the optic nerve (which looks like the optic disc) of the eye. This procedure can detect damage to the optic nerve.
A change in cup shape (deepening of the optic disc) may be caused by increased intraocular pressure. Additionally, a pale nerve color may indicate nerve damage from poor blood flow or increased intraocular pressure.
Special cameras may be used to take photographs of the optic nerve and then compare changes in the nerve that have occurred over time.
Visual examination
Using this method, it is possible to determine the visual signs of glaucoma before damage to the optic nerve. This test can be done in the following way: the doctor looks closely at the patient's eye, while the patient needs to count the fingers shown by the doctor to the side.
Currently, this type of examination is computerized. For this procedure, patients close one eye and place their chin into the ball. When the patient sees lights of varying intensities and in different locations, he or she presses a button.
This process produces a computerized map of the visual area.
Other, more complex studies may also be used. All these tests must be repeated after a certain time to assess the progression of the disease and the effect of treatment.
How often should people be tested for glaucoma?
Ages 20-29: People of African descent or people with close family members with glaucoma should have an eye exam every three to five years. Other people should be examined at least once during this period. Ages 30-39: People of African descent or people with close family members with glaucoma should have an eye exam every two to four years. Other people should be examined at least twice during this period. Ages 40-64: People should be tested every two to four years. Age 65 or older: People should be screened after two years.
These routine eye exams are essential because glaucoma usually causes no symptoms (asymptomatic) in the early stages. Once damage to the optic nerve occurs, glaucoma is not completely cured.
Therefore, to preserve vision, glaucoma must be diagnosed early and monitored at all times. Patients with glaucoma should know that it is a lifelong disease.
These patients must comply with scheduled eye doctor visits and prescribed treatment regimens to ensure they do not lose their vision.
Source: //da-med.ru/diseases/cat-56/d-176/page-3.html