Instructions for use INDAPAMIDE
Saluretics (loop, thiazide), cardiac glycosides, gluco- and mineralocorticoids, tetracosactide, amphotericin B (iv), laxatives when used simultaneously with indapamide increase the risk of hypokalemia.
When taking indapamide simultaneously with cardiac glycosides, the likelihood of developing digitalis intoxication increases; with calcium supplements - hypercalcemia; with metformin – lactic acidosis may worsen.
Indapamide increases the concentration of lithium ions in the blood plasma (decreased urinary excretion), lithium has a nephrotoxic effect.
With the simultaneous administration of indapamide and drugs that can cause aritis, incl. class IA antiarrhythmic drugs (quinidine, hydroquinidine, disopyramide), class III antiarrhythmic drugs (amiodarone, sotalol, dofetilide, ibutilide), antipsychotic drugs - phenothiazines (chlorpromazine, cyamemazine, levomepromazine, thioridizine, trifluoperazine), benzamides (amisulpiride, sulpiride, sultopride, tiapride), butyrophenones (droperidol, halopreridol), other drugs (bepridil, cyazopride, difemanil, erythromycin for IV administration, halofantrine, mizolastine, pentamidine, sparfloxacin, moxifloxacin, IV vincamine), the risk of developing such arrhythmia increases, especially in background of hypokalemia, bradycardia, initially increased QT interval. If it is necessary to prescribe these combinations, the potassium content in the blood plasma and the QT interval should be monitored, adjusting the dosage regimen.
NSAIDs, corticosteroids, tetracosactide, sympathomimetics reduce the hypotensive effect of indapamide, baclofen enhances it.
A combination with potassium-sparing diuretics may be effective in some categories of patients, however, the possibility of developing hypo- or hyperkalemia is not completely excluded, especially in patients with diabetes mellitus and renal failure.
ACE inhibitors when used simultaneously with indapamide increase the risk of developing arterial hypotension and/or acute renal failure (especially with existing renal artery stenosis).
The risk of developing renal dysfunction increases with the simultaneous use of iodine-containing contrast agents in high doses (dehydration). Before using iodine-containing contrast agents, patients need to restore fluid loss.
Imipramine (tricyclic) antidepressants and antipsychotic drugs enhance the hypotensive effect of indapamide and increase the risk of developing orthostatic hypotension.
Cyclosporine, when used simultaneously with indapamide, increases the risk of developing hypercreatininemia.
Indapamide reduces the effect of indirect anticoagulants (coumarin or indanedione derivatives) due to an increase in the concentration of coagulation factors as a result of a decrease in blood volume and an increase in their production by the liver (dose adjustment may be required).
Indapamide enhances the blockade of neuromuscular transmission that develops under the influence of non-depolarizing muscle relaxants.
Indapamide, 30 pcs., 2.5 mg, film-coated tablets
Undesirable combination of drugs
Lithium preparations
With the simultaneous use of indapamide and lithium preparations, an increase in the concentration of lithium in the blood plasma may be observed due to a decrease in its excretion, accompanied by the appearance of signs of overdose. If necessary, diuretic drugs can be used in combination with lithium drugs, and the dose of the drugs should be carefully selected, regularly monitoring the lithium content in the blood plasma.
Combination of drugs requiring special attention
Drugs that can cause aritis:
- class IA antiarrhythmic drugs (hydroquinidine (quinidine), disopyramide), class III antiarrhythmic drugs (amiodarone, dofetilide, ibutilide), sotalol;
- some neuroleptics: phenothiazines (chlorpromazine, cyamemazine, levomepromazine, thioridazine, trifluoroperazine), benzamides (amisulpride, sulpiride, sultopride, tiapride), butyrophenones (droperidol, haloperidol);
- others: bepridil, cisapride, difemanil, erythromycin (iv), halofantrine, mizolastine, pentamidine, sparfloxacin, moxifloxacin, astemizole, vincamine (iv).
Increased risk of ventricular arrhythmias, especially arrhythmias (risk factor: hypokalemia)
The potassium content in the blood plasma should be determined and, if necessary, adjusted before starting combination therapy with indapamide and the above drugs. It is necessary to monitor the patient’s clinical condition, monitor blood plasma electrolytes, and electrocardiogram (ECG) indicators.
In patients with hypokalemia, drugs that do not cause ari should be used.
Non-steroidal anti-inflammatory drugs (when administered systemically), including selective COX-2 (cyclooxygenase-2) inhibitors, high doses of salicylates (≥3 g/day)
The antihypertensive effect of indapamide may be reduced.
With significant fluid loss, acute renal failure may develop (due to a decrease in glomerular filtration rate). Patients need to compensate for fluid loss and carefully monitor renal function at the beginning of treatment.
Angiotensin-converting enzyme (ACE) inhibitors
Prescribing ACE inhibitors to patients with a reduced concentration of sodium ions in the blood (especially patients with renal artery stenosis) is accompanied by a risk of sudden arterial hypotension and/or acute renal failure.
Patients with arterial hypertension and possibly reduced levels of sodium ions in the blood plasma as a result of taking diuretics should: stop taking diuretics 3 days before starting treatment with an ACE inhibitor. In the future, if necessary, diuretics can be resumed. Or start ACE inhibitor therapy with low doses, followed by a gradual increase in dose if necessary.
In chronic heart failure, treatment with ACE inhibitors should begin with low doses with a possible preliminary reduction in the doses of diuretics.
In all cases, in the first week of taking ACE inhibitors in patients, it is necessary to monitor renal function (plasma creatinine concentration).
Other drugs that can cause hypokalemia: amphotericin B (iv), gluco- and mineralocorticosteroids (if administered systemically), tetracosactide), laxatives that stimulate intestinal motility
Increased risk of hypokalemia (additive effect).
Regular monitoring of potassium levels in blood plasma is necessary; if necessary, its correction. Particular attention should be paid to patients concomitantly receiving cardiac glycosides. It is recommended to use laxatives that do not stimulate intestinal motility.
Baclofen
There is an increase in the antihypertensive effect.
Patients need to compensate for fluid loss and carefully monitor renal function at the beginning of treatment.
Cardiac glycosides
Hypokalemia enhances the toxic effect of cardiac glycosides.
With the simultaneous use of indapamide and cardiac glycosides, the content of potassium in the blood plasma, ECG indicators should be monitored, and, if necessary, therapy should be adjusted.
Combination of drugs requiring attention
Potassium-sparing diuretics (amiloride, spironolactone, triamterene, eplerenone (spironolactone derivative))
Combination therapy with indapamide and potassium-sparing diuretics is advisable in some patients, but the possibility of developing hypokalemia (especially in patients with diabetes mellitus and patients with renal failure) or hyperkalemia cannot be excluded.
It is necessary to monitor the potassium content in the blood plasma, ECG indicators and, if necessary, adjust therapy.
Metformin
Functional renal failure, which can occur against the background of diuretics, especially loop diuretics, with simultaneous administration of metformin increases the risk of developed lactic acidosis.
Metformin should not be used if the creatinine concentration exceeds 15 mg/l (135 µmol/l) in men and 12 mg/l (110 µmol/l) in women.
Iodinated contrast agents
Dehydration while taking diuretics increases the risk of developing acute renal failure, especially when using high doses of iodinated contrast agents.
Before using iodinated contrast agents, patients need to compensate for fluid loss.
Tricyclic antidepressants, antipsychotics (neuroleptics)
Drugs in these classes enhance the antihypertensive effect of indapamide and increase the risk of orthostatic hypotension (additive effect).
Calcium salts
With simultaneous administration, hypercalcemia may develop due to a decrease in the excretion of calcium ions by the kidneys.
Cyclosporine, tacrolimus
It is possible to increase the concentration of creatinine in the blood plasma without changing the concentration of circulating cyclosporine, even with normal fluid and sodium ion levels.
Corticosteroid drugs, tetracosactide (if administered systemically)
Decreased antihypertensive effect (retention of fluid and sodium ions as a result of the action of corticosteroids).
To whom and in what cases is the drug Indapamide prescribed?
The drug Indapamide helps to effectively cope with this disease; doctors often prescribe it.
CHARACTERISTICS OF THE DRUG INDAPAMIDE
This drug has diuretic properties. In addition, it dilates blood vessels, relieves spasms, and improves blood circulation. The drug protects the heart muscle and also eliminates possible heart complications in patients with hypertension.
This drug is prescribed to patients with high glucose levels. Detailed information about the purpose of the drug and instructions are presented at: zdravcity.ru/g_indapamid Taking the drug in small doses, as prescribed by a doctor, reduces blood pressure for a long time, without affecting the increased formation of urine. The diuretic effect occurs at significant doses, and the effectiveness of the effect on blood pressure does not change.
Indapamide is almost completely excreted from the body in the urine, and only a small part of it is absorbed into the stomach and intestines. If the drug is taken before meals, the rate of absorption increases significantly.
The drug in question has the following properties:
- Normalizes kidney function by improving blood circulation. This effect is achieved as a result of relieving spasms and dilating renal vessels;
- Eliminates swelling, as it promotes the removal of fluid from the body
- Increases the number of urinations, thereby helping to improve the condition of patients with hypertension.
Some overweight patients take Indapamide as a weight loss aid. This effect is achieved due to diuretic properties and is temporary.
INDICATIONS FOR USE OF THE DRUG, FEATURES
Indapamide is prescribed for chronic heart disease, which results in edema, for hypertension, as a vasodilator to lower blood pressure.
The effect of the drug lasts for 24 hours. With regular consumption in the prescribed dosage, patients' condition improves seven days after the start of treatment. This medicine can accumulate in the body, so if there is no improvement within thirty days from the date of starting treatment, then you cannot increase the dose or change the dosage regimen without the consent of your doctor. Various unwanted complications are possible.
Since taking the drug is associated with the removal of fluid, it is recommended to drink more water during treatment to maintain balance.
Indapamide is recommended to be taken in the morning.
The beginning of treatment may cause weakness, inhibition of reactions, and dizziness, so it is necessary to refrain from driving or performing work that requires composure, attentiveness and quick reaction.
You should take the drug only after a specialist has prescribed it and according to a prescribed regimen, since an overdose can lead to undesirable negative consequences. There may be a decrease in blood pressure, difficulty breathing, severe dizziness, as well as problems in the functioning of the digestive system.
Long courses of treatment with this drug have a negative effect on potency in men.
For patients with gout, this drug is also undesirable, as it increases the level of uric acid.
Taking into account all the characteristic features of the drug, it is necessary to conclude that it must be taken exclusively as prescribed by a doctor and strictly follow the dosage. This will eliminate possible risks and undesirable consequences.
Indapamide should not be used as a means of losing weight, as it will disturb the water balance in the body and also lower blood pressure.
Journal "Arterial Hypertension" 2(4) 2009
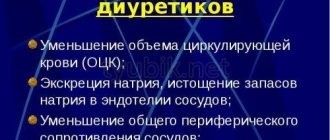
Arterial hypertension (HTN) is a major risk factor for cardiovascular complications and mortality worldwide [1]. In the recommendations of the European Society of Hypertension and the European Society of Cardiology, the concept of a drug of first choice first gave way to the concept of achieving target blood pressure, then to the protection of target organs, and, finally, the final goal is to increase the life expectancy of patients, that is, improve the long-term prognosis [2] . For most patients, a choice should be made from 5 main classes of antihypertensive drugs, depending on target organ damage and associated clinical conditions [2]. According to the British Society of Hypertension algorithm, the choice of drug depends on the age and race of the patient. In white patients under 55 years of age, treatment for hypertension begins with angiotensin-converting enzyme inhibitors (ACEIs). For patients 55 years of age and older or people of black race, therapy with slow calcium channel blockers (CCBs) or diuretics is recommended. Among these drugs, diuretics take pride of place, primarily because they have been used in the treatment of hypertension for much longer than other antihypertensive drugs, namely since the late 50s. Over the years, attitudes toward diuretics as antihypertensive drugs have changed significantly. However, at present we can say with confidence that diuretics are one of the most valuable classes of antihypertensive drugs, as indicated by both international and domestic recommendations for the treatment of hypertension. The value of these drugs and their positive effect on cardiovascular morbidity and mortality have been proven in numerous multicenter prospective studies [3].
How to classify thiazide and thiazide-like diuretics? Thiazide and thiazide-like diuretics, taking into account the characteristics of their renal effects, can be divided into two generations. The first generation includes benzothiadiazine derivatives (hydrochlorothiazide, bendroflumethiazide, polythiazide, etc.) and chlorthalidone, the second generation includes derivatives of chlorobenzamide (indapamide, xipamide, etc.) and quinazolinone (metolazone). Second-generation thiazide-like diuretics differ from first-generation diuretics in that they have significant sodium and diuretic effects in any degree of renal failure. Therefore, in their pharmacodynamic characteristics, indapamide, xipamide and metolazone are more reminiscent of loop diuretics than typical thiazide diuretics. Indapamide is an effective and metabolically neutral antihypertensive drug from the diuretic class with organoprotective effects. Indapamide is a sulfonamide derivative containing an indole ring. According to its pharmacological properties, it is close to thiazide diuretics. This drug has a double effect. On the one hand, it provides a slight increase in natriuresis, like other drugs in this group; this eliminates excess sodium content in the vascular wall. However, to a greater extent it acts as a peripheral vasodilator, while differing from all other thiazide and thiazide-like diuretics. This primary vasodilating effect is associated with the regulation of calcium entry into vascular smooth muscle cells, as well as increased synthesis of prostaglandin E2, produced by the kidneys, and prostacyclin, produced by vascular endothelial cells [4].
What evidence-based medicine is available on the effectiveness of indapamide? The organoprotective effect of indapamide has been proven. In the randomized, double-blind, placebo-controlled PATS study (Post-stroke Antihypertensive Treatment Study, n = 5665, history of stroke or transient ischemic attack, mean age 60 years, follow-up 3 years), a decrease in blood pressure by 5/2 mmHg . during therapy with indapamide at a dose of 2.5 mg/day was accompanied by a decrease in the risk of recurrent fatal and non-fatal stroke (RR 0.71; p < 0.001) [5]. The results of the PATS study served as the basis for establishing in the guidelines the indication for the use of thiazide diuretics for secondary prevention of strokes. According to the results of the LIVE study (Left Ventricular Hypertrophy: Indapamide versus Enalapril, n = 505, treatment duration 12 months), in patients with mild and moderate hypertension with LVH verified by echocardiography with a comparable decrease in blood pressure, a significantly more pronounced regression of LVH during treatment with indapamide was established. midom SR (1.5 mg/day) versus enalapril (20 mg/day) (–6.5 g/m2; p = 0.013; –4.3 g/m2 when normalized to baseline values; p = 0.049) [6]. Since LVH is an independent risk factor for cardiovascular complications, the proven ability of indapamide to influence the regression of LVH is an important advantage of the drug. Another independent risk factor for cardiovascular complications is microalbuminuria (MAU), which is an early marker of renal dysfunction [7]. MAU suggests the presence of endothelial dysfunction, insulin resistance, hyperinsulinemia, dyslipidemia, hypercoagulation. According to the recommendations of the European Society of Cardiology and the European Society of Hypertension, the presence of MAU indicates target organ damage [2]. The randomized, double-blind comparative study NESTOR (Natrilix SR vs Enalapril Study in Type 2 Diabetic Hypertensives with L Microalbuminuria, n = 570, treatment duration 12 months) for the first time demonstrated the ability of the thiazide-like diuretic indapamide to significantly (by 35%) reduce MAU, assessed by the ratio “albumin - creatinine” in night urine in hypertensive patients with type 2 diabetes [8]. In terms of antiproteinuric effect, indapamide was not inferior to enalapril, a representative of the reference nephroprotective class of ACEI (OR 1.08; 95% CI 0.89–1.31). Confirmation of the pronounced antihypertensive activity, metabolic neutrality and nephroprotective effect of indapamide was obtained, which makes it possible to use it as one of the first-choice drugs for the treatment of patients with hypertension and type 2 diabetes, and potentially as an additional drug to ACE inhibitors if combination therapy is necessary. The randomized, double-blind, placebo-controlled X-cellent study (n = 1758, n = 388, mean age 59 years) compared the antihypertensive efficacy and tolerability of indapamide SR, amlodipine and candesartan in patients with hypertension, including those with isolated systolic arterial hypertension (ISAH). ) [9]. The decrease in systolic blood pressure in the general group and in patients with ISAH during therapy with the study drugs is comparable. In the overall group, therapy with indapamide SR compared with amlodipine was accompanied by a more pronounced decrease in pulse blood pressure (by 9.3 and 7.3 mmHg, respectively, p < 0.1). In patients with ISAH (n = 388) in the treatment group with indapamide SR, compared with amlodipine and candesartan, a more pronounced decrease in pulse blood pressure was also observed (by 17.4, 13.3 and 13.7 mm Hg, respectively, the differences were significant between indapamide SR and amlodipine p < 0.1) due to a lesser effect on diastolic blood pressure. During therapy with indapamide SR in patients with ISAH, there were no significant changes in diastolic blood pressure compared to the initial values (increase by 0.5 mm Hg, not significant) in contrast to therapy with amlodipine and candesartan (decrease by 3.0 and 2. 6 mmHg respectively). The differences in the dynamics of diastolic blood pressure between indapamide SR and amlodipine are significant. According to 24-hour blood pressure monitoring (ABPM), in the group of patients with ISAH, indapamide SR is more effective than amlodipine in reducing systolic blood pressure (by 9.8 and 2.9 mm Hg, respectively) [9]. Indapamide is certainly an effective antihypertensive agent, since it meets the most stringent criteria for the effectiveness of antihypertensive drugs and is not inferior in effectiveness to enalapril at a dose of 20 mg and amlodipine at a dose of 5 mg. In addition, it remains highly effective with long-term use. The drug does not affect the lipid spectrum and carbohydrate metabolism. It can be considered the safest diuretic for the treatment of patients with hypertension [10]. According to many authors, only 1% of patients taking indapamide develop hypokalemia, and the average decrease in potassium levels is only 0.3 mmol [11]. Of particular note is the effect of indapamide 1.5 mg sustained release on left ventricular myocardial hypertrophy, proven in the LIVE study [12].
Use of indapamide in elderly and senile patients There are a large number of studies in the literature concerning the use of indapamide in elderly patients [13, 14]. The 2007 ESH/ESC guidelines note that there are no data on the effect of antihypertensive therapy on the risk of cardiovascular complications in patients over 80 years of age [2]. The purpose of the recently completed Hypertension in the Very Elderly Trial (HYVET) was to study the effect of antihypertensive therapy on the risk of stroke in hypertensive patients over 80 years of age [15]. The study included persons 80 years of age and older (with supporting national documents) with constant hypertension and a systolic blood pressure level of more than 160 mm Hg. After randomization, patients received either indapamide sustained release 1.5 mg or a similar placebo. The HYVET study showed that indapamide sustained release 1.5 mg with and without perindopril 2–4 mg was associated with a 30% reduction in the risk of fatal and nonfatal stroke (95% CI (–1)–51; p = 0.06); 21% reduction in the risk of death from all causes (95% CI (-4)-35; p = 0.02); 23% reduction in the risk of death from cardiovascular causes (95% CI (-1)-40; p = 0.06) and 64% reduction in the risk of developing heart failure (95% CI 42-78; p < 0.001 ). Thus, reducing high blood pressure in people over 80 years of age leads to a significant reduction in overall mortality, the incidence of fatal stroke and heart failure, and an improvement in the prognosis of patients. The results of the HYVET study support the need to reduce high blood pressure in patients over 80 years of age using sustained-release indapamide alone or in combination with perindopril. These data should be taken into account in new guidelines for the treatment of hypertension.
Is it possible to treat arterial hypertension with thiazide and thiazide-like diuretics in adolescents? Some authors believe that 3 main classes of diuretics can be used to treat hypertension in adolescents: thiazide and thiazide-like diuretics, loop diuretics and potassium-sparing diuretics [16, 17]. However, only thiazide and thiazide-like diuretics are considered effective for essential hypertension in adolescents. Until recently, the dominant view regarding adolescents and young people was that they should be classified as a low risk group for CVD. However, the results of a number of studies that have appeared in recent years make us look at this problem in a new way and draw attention to the need to take into account risk factors for cardiovascular diseases, and especially hypertension, already at a young age and adolescence. Thus, in a study by the Center Investigations Preventives et Cliniques (IPC), which lasted from 1978 to 1996, it was shown that at the age of 18–55 years, the lowest mortality from cardiovascular causes is observed in patients with normal blood pressure [18]. Moreover, in terms of the degree of influence on the end points, hypertension in the group of young patients turned out to be a more significant risk factor than an increase in total cholesterol levels. This study marked the beginning of the proclamation of new goals in preventing the development of CVD starting in adolescence. It has become obvious that hypertension in adolescents should begin to be treated as early as possible - not only to improve the quality of life of patients, reduce blood pressure and relieve existing symptoms, but also to prevent long-term cardiovascular diseases. Based on these positions, the use of diuretics, which have proven their positive effect on the incidence of CVD and mortality from them, in adolescents finds additional justification. In this regard, the use of indapamide in adolescents and young adults with hypertension is of particular interest; As for the assessment of its effectiveness in hypertension in adolescence and young adulthood, this issue is under study. When conducting a study of the effectiveness of indapamide in 18 adolescents and young adults (16–21 years old) with isolated systolic hypertension, which is especially common in children, adolescents and young adults, according to the results of the Ziac Pediatric Hypertension Study [19], it was found that that, according to the results of daily monitoring, the maximum effectiveness of indapamide after 12 weeks of treatment with this drug is observed in terms of reducing SBP per day, day, night, as well as the SBP time load index (IVSAD).
Is it possible to use indapamide in combination therapy in patients with type 2 diabetes mellitus? The search for methods that increase the effectiveness of treatment for patients with diabetes is of great importance. The most important factors influencing the risk of cardiovascular complications in patients with type 2 diabetes are the level of blood pressure, the state of carbohydrate metabolism and the lipid spectrum of the blood plasma. To study the effect of intensive regimens of antihypertensive and hypoglycemic therapy on the risk of developing cardiovascular complications in patients with type 2 diabetes, a large-scale randomized clinical trial, Action in Diabetes and VAscular disease - preterax and Diamicron MR Controlled Evaluation (ADVANCE), was undertaken. In order to reduce blood pressure in the group of intensive antihypertensive therapy, a drug was used that was a combination of perindopril and indapamide. In the group of active hypoglycemic therapy, in order to achieve the target HbA1c level (<6.5%), the slow-release drug gliclazide was added to standard hypoglycemic therapy. The study included 11,140 patients with type 2 diabetes and a high risk of cardiovascular disease: 40% of patients had a history of macro- and microvascular diseases, 25% of patients had microalbuminuria [20, 21]. During long-term (mean 4.3 years) follow-up, the relative risk of major macrovascular and microvascular cardiovascular events (primary endpoint) was significantly reduced by 9% (861 events, or 15.5%, in the active treatment group versus 938 events , or 16.8%, in the placebo group; risk ratio 0.91; 95% CI 0.83–1.00; p = 0.04). Treatment with a combination of perindopril and indapamide in patients with type 2 diabetes led to a significant reduction in the risk of death from cardiovascular causes by 18% (211 cases, or 3.8%, in the active treatment group and 257 cases, or 4.6%, in the placebo group; p = 0.03) and the risk of death from all causes by 14% (408 cases, or 7.3%, in the active treatment group, 471 cases, or 8.5%, in the placebo group; p = 0 ,03). In the active treatment group, the risk of developing coronary complications was significantly lower by 14% (p = 0.02) and renal complications by 21% (p < 0.0001), mainly due to a reduction in the risk of microalbuminuria by 21% ( p < 0.0001). The effect of therapy did not depend on the initial blood pressure level and the therapy used before inclusion in the study. It should be noted that the study participants received all modern preventive therapy without significant differences between the main group and the placebo group: at the final stage, about 61% of patients received antiplatelet agents, about 52% - lipid-modifying drugs, about 91% - oral hypoglycemic drugs, about 33% - insulin. The antihyperglycemic therapy portion of the ADVANCE trial was presented in June 2008 [20, 21]. In the intensive glucose-lowering therapy group, there was a significant 10% reduction in the risk of developing the combined primary endpoint (see above) compared to the standard therapy group (p = 0.013). With intensive control of HbA1c, there was also a significant reduction in the relative risk of microvascular complications (14%, p = 0.014), mainly due to a decrease in the risk of renal complications (21%, p = 0.006) - one of the most dangerous and severe consequences of diabetes, which is the cause of death in every fifth diabetic patient. There was also a 30% reduction in macroalbuminuria (p < 0.001), a known marker of increased cardiovascular risk. Treatment with high-dose gliclazide was well tolerated: hypoglycemia was observed in only 2.7% of patients, which is 3 times less compared to the UKPDS study. In patients receiving intensive glucose-lowering therapy, there was no increase in weight compared to baseline. Thus, the administration of a fixed combination of perindopril with indapamide to patients with type 2 diabetes was well tolerated and significantly reduced the risk of major cardiovascular events, including death. According to the results obtained, such therapy in 79 patients with diabetes for 5 years would prevent one death from all causes. Calculations have shown that if this combination is used in at least half of the world population of patients with type 2 diabetes, it will be possible to prevent more than 1 million deaths over the next 5 years. More intensive control of HbA1c (about 6.5%) also translated into a reduction in the risk of major micro- and macrovascular complications of type 2 diabetes. This is a convincing argument for the widespread introduction of such treatment for patients with type 2 diabetes into routine clinical practice. Is it possible to extrapolate the results of studies conducted with the retardated form of indapamide to indapamide 2.5 mg? As evidence of this position, we can cite data from a clinical trial conducted at two large medical institutions: the State Research Center for Preventive Medicine of the Federal Agency for Health and Social Development (Moscow) and the Yaroslavl State Medical Academy (Yaroslavl). ), approved by the director of the Federal State Institution GNITS PM Roszdrav R.G. Oganov dated November 11, 2005 [22]. A comparison was made of the clinical effectiveness of the original drug of indapamide - Arifon® and Arifon® retard (Les Laboratories Servier, France), long known in Ukraine, in which the delayed release of indapamide from the active substance allows maintaining a relatively stable concentration of the drug in the blood, which ensures a uniform therapeutic effect in within 24 hours. However, the widespread use of the drug Arifon® and its retarded form in our country is hampered by the high cost of the drugs. Now there is a drug on the Ukrainian pharmaceutical market - generic Arifona® Indap® (PRO.MED.CS Praha as, Czech Republic). Bioequivalence studies conducted in Russia in 2001 demonstrated its full compliance with the original drug. In addition, the clinical equivalence of monotherapy with Indap® (indapamide, PRO.MED.CS Praha as, Czech Republic) was assessed in comparison with Arifon® and Arifon® retard (indapamide, Les Laboratories Servier, France) in patients with mild and moderate hypertension . The results of this study, in which treatment with the study drugs lasted about six weeks, showed that the prescription of the drug Indap® in everyday clinical practice, for which, along with good bioequivalence data, there is also objective evidence of therapeutic equivalence to the original drug, can be considered fully justified if the doctor chooses the thiazide-like diuretic indapamide for the treatment of hypertension [22].
What evidence is there of the clinical effectiveness of Indap®? It is known that during therapy with Indap® in elderly patients, 46% of patients with mild and moderate hypertension achieved the target level of office blood pressure after 4 weeks, and in 86% - after 12 weeks. Analysis of 24-hour blood pressure monitoring indicators revealed a significant decrease in systolic blood pressure per day (initial - 138.26 ± 1.67 mm Hg, after treatment - 127.79 ± 2.16 mm Hg) during the day and night hours, diastolic blood pressure at night (initial - 68.9 ± 1.79 mm Hg, after treatment - 63.74 ± 1.83 mm Hg) [23]. During treatment with Indap®, there was no significant change in the variability of both systolic and diastolic blood pressure. A significant decrease in pressure load indicators was recorded: IVSBP per day, day and night - by 37.7; 33.9 and 45.9%, respectively; IVDAD - by 52.71% and IPDAD - by 49.5% at night. There was a decrease in the left heart, myocardial mass index by 7%, and an increase in left ventricular ejection fraction. At the end of the 12-week course of treatment, a significant decrease in the level of daily microalbuminuria was registered. There was a positive effect of Indap® on the autonomic homeostasis of patients (LF/HF initially - 5.20 ± 0.75, after treatment - 2.70 ± 0.68). Biochemical parameters of carbohydrate, lipid and purine metabolism did not change significantly during treatment with Indap®. A slight decrease in the level of potassium in the blood was detected (4.61 ± 0.12 and 4.17 ± 0.12, respectively), but these changes remained within normal limits. According to the results of the MOS SF-36 questionnaire, the quality of life of patients before treatment with Indap® was 45.9 ± 3.0, after treatment - 47.9 ± 3.2 points. When analyzing individual scales, we observed clear positive dynamics in role-based physical and emotional functioning (increase in scores by 7 and 6%, respectively), general health and love of life - by 7% for each of them. During therapy with Indap®, an increase in a number of indicators was revealed, reflecting an improvement in the state of cognitive-mnestic functions. The most favorable dynamics were observed on the delayed recall scale (increase in score by 22%) [23]. Thus, the availability in Ukrainian pharmacies of an effective, safe and at the same time affordable form of the thiazide-like diuretic indapamide expands our capabilities in the treatment of hypertension, including in the presence of concomitant conditions and complications.
ROLE OF CALCIUM, VITAMIN D AND THIAZIDE DIURETICS IN THE PREVENTION AND TREATMENT OF OSTEOPOROSIS
The paper shows the most adequate approaches to prevent and treat osteoporosis, gives data on the efficacy and significant adverse effects of currently available drugs used in the disease.
E.L. Nasonov Department of Rheumatology MMA named after. THEM. Sechenov (Rector - Academician of the Russian Academy of Medical Sciences M.A. Paltsev)
Ye.L. Nasonov, Department of Rheumatology, IM Sechenov Moscow Medical Academy (Rector is MA Paltsev, Academician of the Russian Academy of Medical Sciences)
ABOUT
Steoporosis is a systemic skeletal disease characterized by a decrease in bone mass and disruption of the microarchitecture of bone tissue, leading to an increase in bone fragility and the risk of fractures [1]. The high prevalence of osteoporosis and associated skeletal bone fractures in the population makes this problem one of the most important for modern medicine [2, 3]. A variety of drugs are currently being tested to prevent and treat osteoporosis. They can be conditionally divided into two main groups: drugs that suppress bone resorption: hormone replacement therapy, calcitonin (miacalcic), bisphosphonates (fosamax), ipriflavone (osteoquin), ossein-hydroxyapatite (osteogenon); drugs that enhance bone tissue formation: fluoride derivatives, anabolic steroids, etc. [4]. The most adequate approach to preventing the early development and rapid progression of osteoporosis (as well as many other chronic diseases) is its prevention, an important component of which is ensuring sufficient intake of calcium and vitamin D in the body. An important area of antiresorptive therapy is associated with the use of active metabolites of vitamin D - calcitriol and alfacalcidol (alpha D3-Teva)
Calcium supplements and vitamin D
Calcium is the most common substance for the prevention, and possibly treatment, of osteoporosis. It is necessary for bone mineralization, promotes an increase in peak bone mass, and has a certain antiresorptive potential, helping to increase the level of ionized calcium in the blood and suppressing the secretion of parathyroid hormone (PTH) [5]. The results of several controlled studies indicate that regular long-term use of calcium supplements in sufficient doses not only inhibits bone resorption, but also reduces the risk of bone fractures [6, 7]. The choice of calcium preparation is important, since dosage forms vary significantly in elemental calcium content, bioavailability and effect on bone metabolism [8]. For example, the highest calcium content is in calcium carbonate (400 mg per 1 g of salt), slightly lower in calcium citrate (211 mg), while calcium gluconate contains only 90 mg of elemental calcium [9]. However, the absorption of calcium carbonate decreases with a decrease in gastric secretion in elderly patients and during treatment with H2-histamine receptor blockers. In contrast, the absorption of calcium citrate is less dependent on the state of gastric secretion, and its bioavailability is higher than calcium carbonate. In addition, calcium citrate, unlike calcium carbonate, suppresses the secretion of PTH, and therefore has a higher antiresorptive potential. Vitamin D and its active metabolites play a very important role in the regulation of calcium homeostasis [9]. In elderly people and in patients treated with glucocorticoids (GC), there is a decrease in intestinal absorption of calcium. Vitamin D deficiency is one of the main causes of secondary hyperparathyroidism, increased bone turnover and bone loss in the elderly. Treatment with vitamin D (10 – 17.5 mcg/day) of women in the late period of menopause leads to a significant reduction in bone loss in the femoral neck [7, 10]. There is evidence of a beneficial effect of vitamin D intake on skeletal bone fractures. According to an 18-month study of 3,270 healthy older women (mean age 84 years), the incidence of hip fractures was 43% and non-vertebral fractures 32% lower in women taking calcium (1.2 g/day) and vitamin D3 (20 μg) than in the control group receiving placebo [11]. The results of a 36-month follow-up of the same group of patients were recently published. In the main group, compared with the control group, the probability of femoral neck fractures decreased by 29% (p <0.01) and non-vertebral fractures - by 24% (p <0.01) [12]. Annual intramuscular administration of vitamin D (150,000-300,000 IU) leads to a reduction in the incidence of upper limb fractures in elderly people [13]. There are some general recommendations regarding the use of calcium and vitamin D supplements for the prevention of osteoporosis. To improve absorption, taking calcium supplements should not be combined with taking foods (with the exception of calcium carbonate) and laxatives that inhibit calcium absorption. Until recently, it was believed that it was best to take calcium in small portions throughout the day in a single dose of no more than 600 mg. However, there have recently been reports that evening calcium supplementation is preferable to suppress the circadian increase in bone resorption at night [14]. While taking calcium, you need to take more fluids. You should keep in mind a certain risk of developing urolithiasis, especially when taking a high dose of the drug (more than 2000 mg/day). Therefore, in persons with a family history of nephrolithiasis, treatment with calcium supplements should be carried out with extreme caution. In this case, it is better to use calcium citrate, which reduces the risk of kidney stones. If constipation develops, you should increase your fluid intake, plant foods high in fiber, or replace your calcium supplement. Reducing calcium excretion from the body is a universal approach to the prevention of GC-induced osteoporosis [15]. This is achieved by both increasing the absorption of calcium in the intestine and reducing its excretion in the urine. To achieve this goal, limiting the intake of sodium chloride is indicated, since this helps to increase the intestinal absorption of calcium, as well as the combined administration of calcium and vitamin D supplements, which enhance the intestinal absorption of calcium and reduce the secretion of PTH [15]. Thus, calcium intake (1000-1500 mg/day) in combination with vitamin D (400-800 IU/day) should be recommended for all women after menopause, but it is especially indicated for elderly people with low absorption of calcium in the gastrointestinal tract and reduced urinary calcium excretion (<2.5 mmol/day) [7, 8]. Similar recommendations can be made regarding the use of calcium and vitamin D for the prevention of GC-induced osteoporosis. Patients with high urinary calcium excretion (> 7.5 mmol/l) are prescribed calcium supplements (500-1000 mg/day) in combination with hypothiazide (25 mg 2 times a day), which has the ability to inhibit urinary calcium excretion. Patients with hypocalciuria should be prescribed calcium supplements in high doses (up to 2000 mg/day) in combination with vitamin D (50,000 IU 1-3 times a week). Calcium intake (at least 500 mg/day) is a mandatory component of the prevention and treatment of osteoporosis using drugs such as estrogens, calcitonin, bisphosphonates, fluorides, etc. It must also be borne in mind that calcium intake after cessation of therapy with anti-osteoporetic drugs allows you to slow down the reactive increase in bone resorption (the “rebound” phenomenon). A very successful calcium preparation is calcium sandoz forte, which is available in the form of “effervescent” tablets. One tablet of this drug contains calcium lactate/gluconate (2.94 g), calcium carbonate (300 mg), which corresponds to 500 mg of ionized calcium.
Thiazide diuretics
Thiazide diuretics, which are widely used by elderly people for the treatment of arterial hypertension (AH) and heart failure, also have a certain antiosteoporetic activity. According to retrospective epidemiological studies in patients with hypertension, long-term use of thiazides is associated with higher bone mineral density (BMD) in various parts of the skeleton [16] and a decrease in the incidence (by 30–50%) of femoral neck fractures [17–19]. The mechanisms that determine the beneficial effect of thiazides on bone mass are not completely clear. Their action is associated primarily with an increase in renal tubular reabsorption of calcium, which in turn can lead to an increase in serum calcium levels, a decrease in the concentration of PTH and 1,25-(OH)2D. Another potential mechanism of action of thiazides is associated with the inhibition of carbonic anhydrase, an enzyme involved in osteoclast-mediated bone resorption.
Table. Types of Osteoporosis
| Type I | Type II | |
| Age (in years) | 51-75 | 70 |
| Sex ratio (female:husband) | 6 : 1 | 2 : 1 |
| Type of bone loss | Mainly trabecular | Trabecular and cortical |
| Rate of bone loss | Accelerated | Not accelerated |
| Typical fracture sites | Vertebrae (compression) and radius | Vertebrae (wedge formation) and femoral neck |
| Function of the parathyroid glands | Reduced | Promoted |
| Calcium absorption | Reduced | Reduced |
| Metabolism of 25-OH-D to 1,25-(OH)2D3 | Secondarily reduced | Primary reduced |
| Main reasons | Factors related to menopause | Factors related to age |
Active metabolites of vitamin D
Despite the positive results of using calcium for the prevention of osteoporosis and its complications, monotherapy with calcium drugs is still not effective enough to reduce bone loss. This is evidenced, in particular, by the results of numerous controlled trials of various anti-osteoporetic drugs, during which patients in the control group were usually prescribed calcium supplements as a placebo. One of the promising areas in the prevention and treatment of osteoporosis is associated with the use of active metabolites of vitamin D. Currently, 2 synthetic active analogues of vitamin D—calcitriol and alfacalcidol (a-D3-Teva)—are used in clinical practice. Calcitriol is identical to the most active metabolite of vitamin D, 1,25-dihydroxycholecalciferol [1,25-(OH)2D3], which is formed in the kidneys and is the end product of vitamin D metabolism. Alphacalcidol (1a-hydroxycholecalciferol) is a biochemical precursor of calcitriol, which is found in the human body quickly transforms in the liver and bones into 1,25-(OH)2D3 [9, 20]. Vitamin D metabolites have a wide range of biological effects beyond the regulation of bone metabolism [20]. The mechanisms of their action are very diverse and are associated with effects on both calcium metabolism and PTH secretion [9], and on the functional activity of osteoclasts and osteoblasts, as well as on muscle tissue, the central nervous system and the immune system [20]. The effects of active vitamin D metabolites in vitro and in vivo are summarized below, determining the advisability of their use for the prevention and treatment of osteoporosis [20]:
- Suppression of bone resorption
- Enhancing calcium absorption in the gastrointestinal tract
- Suppression of parathyroid cell proliferation
- Improved bone quality
- Suppression of trabecular plate perforation
- Strengthening bone reparation
- Enhancing bone matrix synthesis
- Strengthening the synthesis of growth factors
Other effects
- Increased muscle strength
- Increased joint mobility
- Improving neuromuscular conduction
- Suppression of cytokine synthesis (IL-1, IL-2, IL-6, IL-12, g-interferon)
According to multicenter controlled studies, treatment with calcitriol (0.62-0.8 μg/day) in women with postmenopausal osteoporosis for 2 years is associated with an increase in lumbar spine BMD [21, 22] compared to controls.
Factors controlling calcium balance.
PTH – parathyroid hormone CT – calcitonin 1,25(OH)2D3 – vitamin D GH – growth hormone Units are indicated in mg/day
Calcitriol has also been found to have a dose-dependent effect on bone mass [23]. Particularly important results were obtained in a prospective multicenter controlled study [24], which included 622 women (age 50–79 years) with a history of vertebral fractures. In the group treated with calcitriol (0.25 mcg 2 times a day), by the end of the third year of therapy, there was a significant decrease in the incidence of new vertebral fractures (by 70%), starting from the second year of treatment, compared with the group of patients receiving only calcium. (1 g/day). Moreover, a particularly significant reduction in the incidence of spinal fractures was noted in patients with impaired calcium absorption. A positive effect of calcitriol (0.5 – 1.0 mcg/day) in combination with calcium on the incidence of spinal fractures in postmenopausal women [25] and a decrease in the intensity of pain in the spine was found. The latter is associated with the ability of calcitriol to induce the synthesis of calcitonin, which in turn has analgesic activity. A meta-analysis of several of the largest clinical trials suggests that calcitriol reduces the incidence of vertebral fractures by 54% over three years [26]. The use of active metabolites of vitamin D in GC-osteoporosis seems especially promising, since calcitriol suppresses the GC-induced decrease in calcium absorption in the intestine. A recent randomized trial of 103 patients showed that the greatest bone loss (4.3% per year) occurred in patients receiving only 1000 mg of elemental calcium, while patients started on calcitriol (0.6 mcg/day) in combination with calcium during the first 4 weeks of GC therapy, lost only 0.2% of bone mass per year (lumbar spine), and those treated with calcitriol alone lost 1.3% [27]. Treatment with calcitriol (0.5 μg/day) in liver transplant patients is associated with an increase in BMD in the femoral head and lumbar spine [28]. A preliminary analysis of the results suggests that alfacalcidol may have certain advantages over calcitriol, primarily in terms of reducing the incidence of adverse events (hypercalcemia and hypercalciuria). It is hypothesized that calcitriol, by binding directly to vitamin D receptors in the intestine, increases intestinal calcium absorption more strongly than it inhibits PTH synthesis. In contrast, alfacalcidol has no direct effect on intestinal calcium absorption because it must first undergo conversion to 1,25-(OH)2D in the liver. Therefore, alfacalcidol has a more physiological effect, increasing calcium absorption and inhibiting PTH synthesis to approximately the same extent [29]. It has been established that treatment with alfacalcidol is associated with an increase in spinal BMD in postmenopausal women, a decrease in the incidence of spinal fractures [30], and prevention of the progression of osteoporosis; the drug reduces the incidence of postmenopausal fractures in women suffering from rheumatoid arthritis (RA) [31] and in heart transplant patients [32]. When comparing calcitriol (0.5 mg/day) and alfacalcidol (1 mcg/day), it was found that both drugs inhibit bone loss in cortical and trabecular bones to an approximately equal extent, improve the general condition of patients and reduce the intensity of pain in the skeletal bones. The use of active vitamin D metabolites in RA has another important aspect associated with the immunomodulatory effect of the drugs [20, 32]. Calcitriol potentiates the immunosuppressive effect of cyclosporine A [33], which is widely used in clinical practice, both in transplantology and in the treatment of various chronic inflammatory human diseases [34]. The most significant side effects are hypercalcemia and hypercalciuria, the development of which is associated with individual drug overdose [26]. Prolonged hypercalcemia and hypercalciuria can lead to nephrolithiasis and nephrocalcinosis with subsequent development of renal failure. These complications occur especially often due to excessive intake of calcium supplements or when taking thiazide diuretics in combination. This dictates the need for very careful titration of the drug dose in each patient [26, 35]. However, if all necessary recommendations are followed, the rate of treatment interruption is quite low. According to M. Tilyard et al. [24], during 3 years of treatment, the withdrawal rate in patients treated with calcitriol was only 8.6%, and in patients in the control group (who received calcium supplements as a placebo) – 6.5%. It is noteworthy that the most common reasons for treatment interruption were not hypercalcemia and hypercalciuria, but gastrointestinal and neurological symptoms. The recommended dose of calcitriol is 0.5 mcg/day (2 times 0.25 mcg). When limiting dietary calcium intake to 600 mg/day, the dose can be increased to 0.6–1 mcg/day. Alfacalcidol (a-D3-Teva) is effective at a dose of 0.75–1 mcg/day. During drug treatment, it is necessary to monitor serum calcium levels every 4 weeks, 3 and 6 months after the start of therapy, and then every 6 months. If calcium levels exceed 2.7 mmol/L (10.5 mg%), medications should be suspended until they return to normal. Then treatment can be resumed at a dose of 0.25 mcg/day with a gradual (over 1 month) increase to the original dose. Thus, the use of calcium and vitamin D supplements is an important area of prevention, and the use of active metabolites of vitamin D (primarily alfacalcidol) is a very promising approach to the treatment of osteoporosis and associated skeletal bone fractures.
Literature:
1. Consensus Development Conference: Diagnosis, prophylaxis, and treatment of osteoporosis. Am. J. Med. 1993;94:646-50. 2. Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. Report of a WHO Study Group, WHO Tech. Report. Series, 1994;843 (130 pages). 3. Riggs BL., Melton LJ. III. Involutional osteoporosis. N.Engl. J Med 1986;314:1676-86. 4. Kanis JA. Osteoporosis. Blackwell Science, 1994. 5. Nilas L. Calcium intake and osteoporosis. In. Osteoporosis: Nutritional aspects. Ed. Simopouls AP, Galli C. 1993;73:1-26. 6. Chevalley T., Rizzoli R., Nydegger V., et al. Effects of calcium supplements on femoral bone mineral density and vertebral fracture rate in vitamin D-repleted eldery patients. Osteoporosis Int. 1994;4:245-52. 7. Dawson-Hughes B. Calcium, vitamin D and vitamin D metabolites. Osteoporosis 1996. Ed. SE Papapoulos et al. Elsevier. Amsterdam, Lausanne, New York. 1996;299-303. 8. Heaney Rp. Calcium in the prevention and treatment of osteoporosis J. Int. Med. 1992;231:169-80. 9. Rozhinskaya L.Ya., Rodionova S.S., Marova E.N. The role of active metabolites of vitamin D in the pathogenesis and treatment of metabolic osteopathies. Moscow, 1997. 10. Ooms ME., Roos JC., Bezemer D., et al. Prevention of bone loss by vitamin D supplementation in older women: a randomized double-blind trial. J. Clin. Endocrinol. Metab., 1995;80:1052-8. 11. Chapuy MC., Arlot ME., Duboef F., et al. Vitamin D3 and calcium prevent hip fractures in older women. N.Engl. J. Med. 1992;327:1637-42. 12. Chapuy MC., Arlot ME., Delmas P., Meunier PJ. Effect of calcium and cholecalciferol treatment for three years on hip fractures in older women. Br. J Med 1994;308:1081-2. 13. Heikinheimo RJ, Inkovaara JA, Harju EJ, et al. Annual injection of vitamin D and fractures of aged bones. Calcif issue int. 1992;51:105-10. 14. Blumsohn A, Herrington K, Hannon RA, et al. The effect of calcium supplementation on the circadian rhythm of bone resorption. J Clin Endocrinol. 1994;79:730-5. 15. Dequeker J, Westhovens R. Low dose corticosteroid associated osteoporosis in rheumatoid arthritis and its prophylaxis and treatment: bone of contention. J. Rheumatol. 1995;22:1013-9. 16. Cauley JA, Cummings SR, Seeley DG, et al. Effects of thiazide diuretic therapy on bone density, fractures, and falls. Ann. Intern. Med. 1993;118:666-73. 17. LaCroix ZZ, Weinpahl J, White LR, et al. Thiazide diuretic agents and incidence of hip fracture. New Engl. J Med 1990;322:286. 18. Rey WA. Thiazide diuretics and osteoporosis: time for clinical trial. Ann. Int. Med 1991;115:64. 19. Wasnich RD, Davis JW, He YF, Petrovich H, Ross PD. A randomized, double-masked, placebo-controlled trial of chlorthalidone and bone loss in elderly women. Osteoporosis Int. 1995;5:247-51. 20. Dambacher MA, Schacht E. Osteoporosis and active vitamin D metabolites. EULAR Publishers, Basle, Switzerland, 1996. 21. Aloia JF, Vaswani A, Jeh JK, et al. Calcium supplementation with and without hormone replacement therapy to prevent postmenopausal bone loss. Ann. Intern. Med. 1994;120:97-103. 22. Gallagher JC, Goldgar D. Treatment of postmenopausal osteoporosis with high doses of synthetic calcitriol. Ann. Intern. Med 1990;113:649-55. 23. Ott SM, Chesnut CH. Tolerance to dose of calcitriol is associated with improved bone density in women with postmenopausal osteoporosis. J. Bone Miner. Res., 1990;5(suppl. 2): S 186. 24. Tilard MW, Spears GF, Thompson J, Dovey S. Treatment of postmenopausal osteoporosis with calcitriol or calcium. N.Engl. J. Med. 1992;32:357-62. 25. Cannigia A, Nuti R, Lore F, et al. Long-term treatment with calcitriol in postmenopausal osteoporosis. Metabolism 1990;39(suppl. 1):43-9. 26. Dechant K, Goa KL, Calcitriol. A review of its use in the treatment of postmenopausal osteoporosis and its potential in corticosteroid-induced osteoporosis. Drug & Aging 1994;5:300-17. 27. Sambrook P, Birmingham J, Kelly P, et al. Prevention of corticosteroid osteoporosis: a comparison of calcium, calcitriol and calcitonin. N.Engl. J. Med. 1993;328:1747-52. 28. Neuhaus R, Lohmann R, Platz KR, et al. Treatment of osteoporosis after liver transplantation. Transplant. Proc. 1995;27:1226-7. 29. Baylink DJ, Akesson K, Pettis JL. Rationale for active vitamin D analogue therapy in osteoporosis. Osteoporosis Int. 1996;6(suppl. 1):313. 30. Orimo H, Shiraki M, Hayshi Y, et al. Effects of 1a-Hydroxy vitamin D3 on lumbar bone mineral density and vertebral fractures in patients with postmenopausal osteoporosis. Calcif. Tissue Int. 1994;54:370-6. 31. Dequeker J, Linthoudt H, Vanschoubroeck I, et al. Prevention of postmenopausal bone loss by 1alpha vitamin D3. Akt. Rheumatol. 1994;19(suppl.):19-22. 32. Dequeqer J, Declerk K, Mbuyi-Muamba JM. Role of alfa-calcidol in autoimmune diseases and organ transplantation on bone quality and immunomodulation. Osteoporosis Int. 1996;6(suppl. 1):314. 33. Gupta S, Fass D, Shimizu M, Vayuegula B. Potential of immunosuppressive effects of cyclosporin by 1 alpha, 25-dihydroxyvitamin D3. Cellular immunology 1989;121:290-7. 34. Nasonov E.L., Shturman V.Z., Nasonova V.A. Cyclosporine A in the treatment of rheumatic diseases. Wedge. honey. 1994. 35. Rozhinskaya L.Ya., Marova E.I., Mishchenko B.P., et al. Experience in the treatment of osteopenic syndrome with 1a-hydroxycholecalciferol (a D3-Teva). Wedge. Pharmacol. Therapy 1996;5:75-8.
Clinical efficacy of indapamide in patients with hypertension
G
Hypertension (HD) is one of the leading causes of disability and mortality. A prolonged increase in blood pressure (BP) leads to target organ damage and the development of cardiovascular complications (heart failure, myocardial infarction, cerebral stroke and renal failure) [2, 3, 8].
Drugs for the treatment and prevention of complications of hypertension should have high therapeutic efficacy, a long-lasting antihypertensive effect throughout the day, and the absence of metabolic side effects [3, 4, 8].
The listed requirements are fully met by the drug belonging to the second generation of thiazide and thiazide-like diuretics, indapamide
. The mechanism of its antihypertensive action is associated with inhibition of sodium reabsorption in the distal convoluted tubules and the development of peripheral vasodilation [6]. Unlike hydrochlorothiazide, indapamide does not affect lipid and carbohydrate metabolism [7, 9]. One of the advantages of the drug is the ability to reduce the mass of hypertrophied left ventricular myocardium [5].
Indapamide has high bioavailability (90–95%) and a long half-life (15–25 hours), which allows for a stable antihypertensive effect throughout the day [4].
The purpose of the study conducted in our clinic was to evaluate the effectiveness and safety of indapamide under conditions of 24-hour blood pressure monitoring (ABPM), studying central hemodynamics under the control of a number of parameters of the biochemical spectrum of blood.
The study included 30 patients (12 men and 18 women) with stage I and II hypertension (according to WHO classification). The average age of the group was 47.1±11.5 years, the duration of the disease was 8.0±7.05 years. 10 patients had mild and 20 had moderate arterial hypertension (AH). Patients with symptomatic hypertension, unstable angina, previous myocardial infarction or acute cerebrovascular accident in the last 6 months, a history of liver and kidney diseases, and intolerance to sulfonamides were excluded from the study. The duration of observation was 8 weeks.
After an introductory period, during which patients did not receive antihypertensive therapy, indapamide (Hemofarm, Yugoslavia) was prescribed at a daily dose of 2.5 mg, once in the morning. If monotherapy was ineffective for 1 month, enalapril (Hemofarm, Yugoslavia) was added at a daily dose of 5–20 mg. At baseline and after 8 weeks of treatment, antihypertensive efficacy using ABPM, the effect on central hemodynamic parameters, and levels of electrolytes and blood lipids were assessed in all patients.
ABPM was carried out using a portable recorder ABRM-04 from Meditech (Hungary), which records blood pressure and heart rate during the decompression phase using the oscillometric method. Measurements began at 9–10 am. The intervals between blood pressure and heart rate measurements were 15 minutes during the day and 30 minutes at night. Based on ABPM data, we analyzed the average indicators of systolic blood pressure (SBP), diastolic blood pressure (DBP), heart rate during periods of wakefulness, sleep and for the day as a whole, standard deviation to assess the variability of blood pressure and heart rate; degree of nocturnal reduction in blood pressure (SNS – percentage of reduction in blood pressure at night); percentage of blood pressure measurements exceeding the upper limit of normal in the total number of registrations; variability index. Blood pressure levels below 140/90 mmHg are considered normal. Art. during the day and below 120/70 mm Hg. Art. at night. Central hemodynamics were studied using an Acuson apparatus (USA).
Results and discussion
Before starting treatment, patients complained of headache (63%), dizziness (37%), pain in the heart of various types (27%), decreased performance (50%). 23% of patients had no complaints. According to ABPM data (Table 1), there was an increase in the average daytime, average nighttime and average daily values of SBP and DBP. The proportion of measurements that exceeded the norm, as well as the variability index, exceeded the permissible normative values, which indicated an increase in hypertensive load. The degree of nocturnal decrease (NNR) for SBP was 10.0±6.0%, for DBP – 13.0±7.5%, which corresponds to the “dipper” group. Initially, indicators of central hemodynamics (Table 2) such as average blood pressure per day and total peripheral vascular resistance (TPVR) were significantly increased.
After 8 weeks of therapy, clear positive dynamics were noted in the patients’ condition. The general well-being of the patients improved, dizziness decreased or disappeared (in 82%), headaches (in 58%), cardialgia (in 100%), and performance increased (in 80%). All patients had good tolerability of treatment, there were no side effects.
When assessing the data obtained, normalization of DBP (decrease to 90 mm Hg or lower) was considered a good result of treatment; a satisfactory result was a decrease in DBP by 10 mm Hg. Art. and more (but not to normal values), unsatisfactory - a decrease in DBP by less than 10 mm Hg. Art. or increased blood pressure. In 16 patients receiving monotherapy with indapamide, the antihypertensive result was assessed as good, in 2 patients - as satisfactory. Thus, 60% of patients achieved an effect during treatment with indapamide, which corresponds to the available literature data on the effectiveness of monotherapy [8].
There was a significant decrease in SBP per day, day, night by 14.5, 14.9 and 18 mm Hg. Art., respectively. Average daily, daytime, and nighttime DBP decreased by 8.8, 8.9, and 14.3 mmHg, respectively. Art. A significant decrease in the blood pressure variability index was revealed. Particularly noteworthy is the decrease in the absolute value of DBP and the DBP variability index, since changes in these indicators correlate with target organ damage [10]. During treatment, an unreliable increase in the SNS was noted, not exceeding 20%. The above indicates that a single dose of indapamide 2.5 mg is sufficient to maintain normal blood pressure throughout the day without affecting the physiological circadian rhythm of blood pressure.
When analyzing central hemodynamics during monotherapy with indapamide, a significant decrease in average blood pressure per day (p <0.01) and total peripheral resistance (p <0.05) was revealed, which largely explains the predominant effect of indapamide on DBP (Table 2). The dynamics of shock and cardio indices were statistically insignificant.
Twelve patients received combination therapy (indapamide 2.5 mg/day + enalapril 5–20 mg/day). At the same time, there was a significant decrease in SBP and DBP per day, day and night (Table 1), and the BP variability index. SNS increased slightly within the “dipper” group, that is, there was also no change in the circadian rhythm of blood pressure. According to echocardiography, there was a significant decrease in average blood pressure per day by 7.2% (p<0.01), peripheral vascular resistance by 13.3% (p<0.05), other indicators changed unreliably (Table 2). In 8 patients receiving combination therapy with indapamide and enalapril, the antihypertensive result was assessed as good, in 2 patients as satisfactory, in 2 patients as unsatisfactory, and therefore required the addition of verapamil at a dose of 120 mg per day. After 8 weeks of indapamide therapy, an insignificant decrease in the levels of sodium (from 142.4±2.9 to 140.4±2.3 mmol/l) and potassium (from 4.4±0.4 to 3.96±0.3) was noted mmol/l) in blood serum. Not a single patient had electrolyte levels (and, most importantly, potassium) that dropped below normal values. There were also no significant changes in the content of cholesterol and triglycerides compared to the initial level.
conclusions
1. Indapamide is a highly effective antihypertensive drug for the treatment of patients with mild and moderate forms of hypertension.
2. Considering the effect of indapamide on the peripheral vascular resistance, the drug can be prescribed primarily for diastolic hypertension.
3. The metabolic inertness of indapamide, unlike thiazides, makes it possible to recommend it to patients with hypertension in combination with metabolic disorders.
4. Adding enalapril to indapamide (if monotherapy is insufficiently effective) allows you to achieve the target blood pressure level.
Indapamide -
Indapamide (trade name)
(Hemofarm)
Literature:
1. Bulkina O.S., Dobrovolsky A.B., Britareva V.V., Marenich A.V., Karpov Yu.A. Ross. cardiol. magazine 1999; 1:39–42.
2. Gogin E.E. Hypertonic disease. M.; 1997.
3. Makolkin V.I., Podzolkov V.I. Hypertonic disease. – M.; 2000.
4. Sidorenko B.A., Preobrazhensky D.V. Diagnosis and treatment of arterial hypertension. Part two. Diuretics. M.; 2000.
5. Campbell DB, Brackman FJ Clin. Pharmacol. 1991; 31: 751–757.
6. Campbell DB, Moore R. Am. J. Hypertens. 1981; 57: 7–17.
7. FuJii S., Kaku K., Andou S., Nakayama H. et al. Clin. Ther. 1993; 15:6.
8. Hanson L., Hedner T. Hypertension Manual. 3rd ed., 2000.
9. Weidmann P., M. De Courten, P. Ferrari, Lorenz Bohlen. J. Cardiovasc. Pharmacol. 1993; 22(Suppl. 6): 98–105.
10. White WB, Dey HM, Schulman P. Am. Heart J 1989; 118:782–795.