Causes
The causes of bladder atony are the following factors:
- insufficient influence of the nervous system on contractile muscle fiber formation;
- sacral spinal cord injury;
- prostate adenoma;
- degenerative diseases of the spine;
- damage to the dorsal roots of the spinal cord.
Bladder atony is more common in women than in men. Sometimes the main cause of the disease is frequent cystitis.
Neurogenic Bladder League
Treatment of bladder hypotension
In accordance with the recommendations of the European Association of Urology, there are currently no drugs with proven effectiveness for detrusor hypotension. The results of the studies do not allow us to talk about the advisability of using parasympathomimetics, especially taking into account the frequency and/or severity of possible side effects.
If there is more than 100-200 ml of residual urine in the bladder, periodic catheterization of the bladder should be performed. This method is considered the “gold standard” for the management of patients with impaired bladder emptying due to neurological diseases.
Treatment of detrusor-sphincter dyssynergia
Alpha-blockers (both selective and non-selective) have demonstrated partial effectiveness in reducing intraurethral resistance and residual urine volume (evidence level 2a).
Alpha-blockers include substances that competitively inhibit alpha-adrenergic receptors (alpha-AR). There are two main subtypes of alpha AR. These are alpha1 and alpha2 AR. The alpha1 subtype is the target of conservative therapy for urinary tract diseases. Three groups of alpha1 ARs have been identified: alpha1A, alpha1B and alpha1D. Alpha1A-ARs are dominant in the bladder neck and proximal urethra, while alpha1D-ARs are mainly located in the bladder wall and dome. Blockade of the alpha1A subtype causes a decrease in the tone of the bladder neck and prostate gland and improves urine outflow. Blockade of alpha1D-AR receptors leads to a decrease in irritative symptoms.
In order to reduce the phenomena of bladder obstruction, patients with a neurogenic bladder can be prescribed the following alpha blockers:
Tamsulosin is the only selective alpha1A-AR blocker. It is prescribed once a day. It has virtually no effect on blood pressure, so can be taken in the morning.
Alfuzosin blocks alpha1-AR primarily in the genitourinary organs, but can significantly reduce blood pressure. It is recommended to use prolonged forms of the drug.
Terazosin and doxazosin are selective long-acting alpha1-blockers. They are prescribed once a day at night, as they cause arterial hypotension.
Centrally acting muscle relaxants
Centrally acting muscle relaxants, due to the relaxation of striated muscles, can reduce the tone of the urethral sphincter in patients with detrusor-sphincter dyssynergia.
Baclofen or tizanidine 3-4 times a day may be prescribed.
Due to pronounced side effects, the use of this group of drugs for the correction of urinary disorders is limited.
If drug therapy is ineffective, injections of botulinum toxin type A into the external sphincter of the bladder allow it to relax, facilitate urination, and reduce the volume of residual urine.
Atrophic vaginitis
Postmenopausal atrophic vaginitis is detected in almost 75% of women 5-10 years after the cessation of menstruation.
The condition and functioning of the stratified squamous epithelium in the vagina depends on estrogens. When a woman enters menopause, her ovaries begin to produce less and less estrogen, then the production process stops completely. This leads to the fact that the vaginal epithelium becomes thin, dry (atrophies), loses elasticity and the ability to withstand various inflammations.
In a healthy woman of reproductive age, an acidic environment (pH 3.5-5.5) is maintained in the vagina, which is an obstacle to the penetration of opportunistic and pathogenic microorganisms.
A decrease in the production of female sex hormones in the ovaries leads to the fact that lactobacilli, which produce lactic acid, begin to disappear from the vaginal flora, thanks to which pathogenic microorganisms cannot reproduce. The vaginal environment becomes alkaline, which leads to a decrease in its protective properties and the appearance of various infections.
The most common symptoms of atrophic vaginitis are:
- vaginal dryness (urogenital atrophy);
- itching and burning in the vagina;
- spotting bloody discharge from the genital tract;
- prolapse of the vaginal walls;
- colpitis (inflammation of the vaginal mucosa caused by various infections);
- painful sensations in the vagina during sexual intercourse.
Also, stretching of the pelvic ligaments and weakening of the muscle tone of the ligaments leads to prolapse of organs, frequent urge to urinate and urinary incontinence.
Diagnosis of atrophic vaginitis
Diagnosis of urogenital atrophy is quite simple and includes several examinations, such as:
- gynecological examination;
- extended colposcopy helps to see the thickness of the vaginal mucosa, whether there is bleeding, the condition of the subepithelial vascular network;
- laboratory tests (flora smear and bacterial culture).
Types of urogenital disorders
In the 19th and early 20th centuries. such problems were not relevant, since many women simply did not live to see the postmenopausal period. Currently, urogenital disorders are observed in every third woman who has reached 55 years of age and in seven out of ten women who have reached 70 years of age.
Urogenital syndrome (or urogenital disorders, UGR) is manifested by atrophic vaginitis, urodynamic and sexual disorders. The appearance of UGR is directly related to a deficiency of estrogen, the main female hormones.
1 Urogenital syndrome. Diagnosis and treatment
2 Urogenital syndrome. Diagnosis and treatment
3 Urogenital syndrome. Diagnosis and treatment
Delayed primary bladder closure in children with exstrophy and microcystis
Yu.E. Rudin, Yu.Yu. Sokolov, A.Yu. Rudin, D.V. Marukhnenko, V.I. Runenko, A.S. Kirsanov, E.V. Kartseva, N.V. Medvedev
Information about authors:
- Rudin Yu.E. – Doctor of Medical Sciences, Professor, Head of the Pediatric Urology Group, Research Institute of Urology and Interventional Radiology named after. ON THE. Lopatkina - branch of the Federal State Budgetary Institution "National Medical Research Center of Radiology" of the Russian Ministry of Health; Moscow, Russia; RSCI AuthorID 423343
- Sokolov Yu.Yu. – Doctor of Medical Sciences, Professor, Head of the Department of Pediatric Surgery, Federal State Budgetary Institution RMANPO, Ministry of Health of Russia; Moscow, Russia; RSCI AuthorID 439748
- Rudin A.Yu. – pediatric urologist-andrologist of the State Budgetary Institution of Healthcare of the Children's City Clinical Hospital of St. Vladimir DZM; Moscow, Russia;
- Marukhnenko D.V. – Candidate of Medical Sciences, Head of the Children's Uroandrological Department of the Research Institute of Urology and Interventional Radiology named after. ON THE. Lopatkina – branch of the Federal State Budgetary Institution “National Medical Research Center of Radiology” of the Russian Ministry of Health; Moscow, Russia; RSCI AuthorID 562464
- Runenko V.I. – Candidate of Medical Sciences, Head of the Children's Uroandrological Department of the State Budgetary Institution of Healthcare of the Children's City Clinical Hospital of St. Vladimir DZM; Moscow, Russia;
- Kirsanov A.S. – Head of the surgical department for newborns and premature babies of the State Budgetary Institution of the Children's City Clinical Hospital of St. Vladimir DZM; Moscow, Russia; RSCI AuthorID 1047182
- Kartseva E.V. – Candidate of Medical Sciences, pediatric surgeon of the State Budgetary Institution of Healthcare of the Children's City Clinical Hospital of St. Vladimir DZM; Moscow, Russia; RSCI AuthorID 339435
- Medvedeva N.V. - pediatric surgeon of the State Budgetary Institution of Healthcare of the Children's City Clinical Hospital of St. Vladimir DZM; Moscow, Russia
INTRODUCTION
Bladder exstrophy (BEC) is one of the most severe congenital malformations encountered in pediatric urology. The severity of the condition in this case is due to the large volume of the anatomical defect and the complexity of its adequate and functional correction [1-4].
To date, pediatric urologists have accumulated sufficient experience in the treatment of this malformation. Various options for staged [1-6] and one-stage [7, 8-12] surgical treatment have been proposed. Some techniques for closing the bladder can be supplemented with orthopedic aids [1-6] using special options for immobilization in the postoperative period [2, 13, 14] or performed without reducing the pelvic bones [15, 16]. In the treatment of such patients, new pharmacological drugs are used, as well as endoscopic administration of bulk-forming substances [4, 6]. Despite this, treatment of bladder exstrophy does not always lead to the desired result and remains a challenge [1-10].
EMT requires an integrated approach to correct complex combined defects of the urinary and reproductive systems. In addition to the proven surgical technique, the equipment of the clinic, the preparedness of medical personnel and parents, a balanced and careful selection of patients depending on their initial anatomical data plays an important role. There is an opinion that the small size of the cystic area is a poor prognostic sign for the treatment of exstrophy [1-8].
Primary closure operations in newborns and infants with microcystis are much more often accompanied by complications and relapses [1-6, 13-18]. Many authors recommend excision of the bladder in patients with microcystis and formation of a reservoir from a segment of the intestine already in infancy [1, 2, 4-6]. In this regard, debatable questions remain: is it possible to stretch the cystic area during EMT and try to preserve function during microcystis? Is it advisable to perform primary plastic surgery in patients with EMT with a bladder size of less than 3 cm in the neonatal period or early infancy? What is the optimal timing for a delayed primary closure? In what cases is it worth abandoning attempts to preserve the vesical site in favor of augmentation operations?
MATERIALS AND METHODS
During the period from 1994 to 2021, we operated on 265 children with bladder exstrophy. In newborns from 2 days to 30 days, 123 patients were hospitalized at the clinic for primary closure of the bladder. The remaining 142 children were not included in this study, since they were admitted to the clinic over the age of 1 year and were operated on at the age of 12 months. up to 18 years old. Of these, 46 children required primary or secondary closure; the remaining 96 children (previously operated on in other clinics) underwent various stages of correction of penile defects and urinary incontinence.
Among 123 newborn patients with EMF analyzed, there were 84 boys (68.2%), twice as many as 39 girls (31.7%). The distribution of patients depending on the form of the defect was as follows: classic exstrophy of the bladder was detected in 112 patients (91%), partial exstrophy - in 8 (6.5%) children, exstrophy of the cloaca - in 3 (2.4%) patients. All these children had no previous surgical interventions. To create a homogeneous group, patients with cloacal exstrophy and partial exstrophy were not included in the study.
All newborn patients with the classic form of EMF (112 cases) were divided into two groups depending on the size of the bladder area. The first group included 75 (67%) patients with large and medium-sized bladder areas.
34 (30.3%) children had large (more than 5 cm) bladder sizes; the average size of the exstrophied area (31-50 mm) was detected in 41 (36.6%) patients.
The second group consisted of 37 (33%) children with microcystis - small sizes of the bladder area - 30 mm or less (Fig. 1). It is precisely the tactics of treating patients with microcystis that we decided to analyze in this work.
Rice. a 1 month old boy 1. Male newborn 1 month old with bladder exstrophy (BE), microcystis
Various management tactics were proposed for children with microcystis; we conditionally divided the patients in this group into two subgroups.
The first subgroup included 30 patients with microcystis, operated on from 1994-2017, who underwent primary closure of the bladder in the immediate period after birth (3-15 days), an average of 6.4 days. (Fig. 2).
Rice. 2. Distribution of newborn patients with EMF and microcystis by age at the time of surgery 2. Distribution of newborns with bladder exstrophy, microcystis by age according to the moment of surgery
The scope of the operation in patients of the first subgroup was: isolation and closure of the bladder, complete or partial reduction of the symphysis pubis by suturing and tightening the pelvic bones, suturing the defect of the anterior abdominal wall. Plastic surgery of the bladder neck and reimplantation of the ureters were not performed due to the small size of the bladder platform.
The second subgroup included 7 patients with microcystis, observed in the clinic between 2017 and 2021, 5 of whom underwent delayed primary closure of the bladder. Newborns were discharged home with recommendations to stretch the bladder platform
In order to increase the size of the bladder platform, methods were used to mechanically stretch the wall of the vicious bladder through manual pressure - by immersing a finger in a rubber glove into the inside of the open eventrated bladder at the initial stages (Fig. 3 A), and then using the inflatable balloon of the Foley catheter. The attending physician previously explained in detail the technique of immersing the finger and stretching the bladder area with a Foley catheter and showed it to the parents, and monitored the correctness of the procedure. The effectiveness of stretching the bladder wall was assessed at face-to-face consultations, and more often – remotely using photographs sent to the doctor’s email address.
The use of a Foley catheter to stretch the bladder platform with measurement of the volume of liquid injected into the inflatable balloon in milliliters and determination of the level of immersion of the balloon into the developing cavity made it possible to more reliably assess the change in the size of the bladder platform according to the depth of immersion than measurement with a flexible tape or ruler.
The principle of the technique was as follows: physiological solution was injected into the balloon of the Foley catheter 10-12 Ch, starting with a volume of 3 ml - the estimated capacity of the bladder. The vesical area was pre-treated with a lubricating anesthetic (for example, Kategel gel, Instillagel). The catheter balloon was placed in place of the bladder platform and, gradually pressing on it from above with fingers, was immersed in the pelvic cavity, thereby more accurately determining the volume of the hemisphere (Fig. 3B)
Initially, the volume of the bladder platform was 5-6 ml (the 10 ml Foley catheter balloon was only half immersed) in 6 children, one child had a volume of 8 ml (the 10 ml balloon was 4/5 immersed in the pelvic cavity).
As the bladder wall stretched, the volume of injected fluid and the diameter of the catheter were increased. Once deep immersion of the catheter with a small amount of saline is achieved, the volume of the balloon can be further increased to provide further distension. A napkin or tourniquet consisting of several napkins was placed on the balloon and, in the maximum immersed state, it was fixed to the skin of the anterior abdominal wall with an adhesive plaster (Fig. 3 C, D) in order to ensure a longer mechanical effect. The stretching time was gradually increased from 5 to 10, then 20, 30 minutes or more. After this manipulation, the vesical area was lubricated with antibacterial ointment (Levomekol, Baneocin). These procedures were carried out daily in order to create a long-lasting effect that simulates the filling of the bladder and gradually stretches its wall.
Rice. 3. Stretching of the vesical area in a 6-month-old child with exstrophy and microcyssm A – stretching using finger immersion. B – installation of a 5 ml balloon. C, D – immersion and fixation of the balloon with adhesive tape 3. Bladders plate tension in 6 months old newborn with bladder exstrophy and microcystis. A – tension by finger. B – tension using Foley's сatheter balloon 5 ml. C, D – immersion and fixation of the balloon with an adhesive plaster
To enhance the result of manual stretching of the bladder wall, we used injections of Botulinum toxin type A (BTA, BOTOX, Lantox). Needling the muscular wall of the bladder area allows you to remove excess tone, and in combination with mechanical stretching helps to achieve greater growth and stretching of the bladder wall in less time. Due to the peculiarities of the pharmacological properties of the active substance, the most effective is two or three times injection at 10-12 points, no more than once every 6 months. Depending on the age and weight of the child, we used 50-100 units of the active substance diluted in 4-8 ml of saline solution (Fig. 4). The use of BTA was carried out on the basis of the children's uroandrology department of the St. Vladimir Children's City Clinical Hospital after preliminary obtaining the informed consent of the patients' parents and approval by the local ethical committee.
Rice. 4 Incision of the bladder wall with polypous growths with botulinum toxoid type A in a 7-month-old child with exstrophy and microcystis. Fig. 4 Injections of Botulinum toxin type A in bladders plate with polyps. Male newborn 7 months old with bladder exstrophy, microcystis
The use of BTA and mechanical impact on the walls of the bladder allowed us to achieve gradual stretching of the bladder platform to volumes (sizes) allowing us to perform the operation of primary closure of the bladder according to the expanded protocol we presented earlier [18]. We considered an increase in the size of the bladder area to 6-7 cm or immersion of a Foley catheter balloon with a volume of 9-11 ml into the pelvic cavity as an indication for delayed surgery.
Surgical intervention according to the protocol included: isolation and closure of the bladder, excision of large polyps, reimplantation of the ureters from the area of Lietaud’s triangle into the bottom of the bladder with anti-reflux protection according to Cohen, plastic surgery of the bladder neck according to Kelly with mobilization of the corpora cavernosa from the pubic bones (in boys), bilateral osteotomy of the iliac bones with fixation of fragments with knitting needles, reduction and fixation of the pubic bones with absorbable thread, plastic surgery of the anterior abdominal wall, formation of the navel.
Delayed closure of the bladder was performed in 5 children out of 7 patients in the second subgroup with microcystis. Operations were performed on three children aged 12-16 months. Botulinum toxin injections were performed twice in this group of patients. The other two patients underwent delayed closure later, at 21 and 26 months of age, respectively. The stretching of the bladder wall was too slow and they were injected with botulinum toxin three times.
In two patients, at this stage of treatment, it was not possible to stretch the platform to a size of 4-5 cm. The tissues remain dense and rigid, and polypous growths fill most of the platform. In case of further absence of positive dynamics, these children are planned to have bladder augmentation with the formation of a wet stoma.
RESULTS
The results of primary bladder closure in patients with microcystis were monitored over a period of 6 months. up to 15 years.
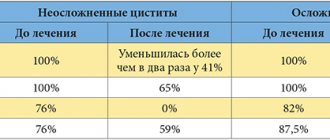
In the first subgroup of 30 children with microcystis operated on as newborns, complications were observed in 13 (43.3%) patients. Relapse of exstrophy occurred in 10 (33.3%) patients. Dehiscence of the postoperative wound of the anterior abdominal wall was observed in 3 (10%) children (Table 1).
Table 1. Results of primary closure surgery in children with bladder exstrophy and microcystis
| Nature of complications Complications Groups of patients Patients' groups | Relapse of exstrophy | Postoperative wound dehiscence Wound dehiscence | Failure of the bladder neck | Total Total |
| Group 1: Microcystis < 3 cm Microcystis < 3 cm 30 patients operated on newborns | 10 (33,3%) | 3 (10%) | – | 13 (43,3%) |
| Group 2: Microcystis < 3 cm Microcystis < 3 cm 5 patients (deferred operations in 1 year and later) | – | – | 1 (20%) | 1 (20%) |
| Total: 35 Total: 35 | 10 (28,6%) | 3 (8,6%) | 1 (2,9%) | 14 (40%) |
Repeated surgeries for secondary bladder closure with bilateral osteotomy were successful in all children. However, upon further follow-up, 24 children maintained complete urinary incontinence and minimal bladder capacity. To achieve urinary continence, 13 patients required from 3 to 5 operations each, including re-plasty of the bladder neck, resulting in an increase in bladder volume to 150 ml and urinary continence for more than 2 hours. Augmentation of the bladder with a segment of the small intestine with appendicovesicostomy for catheterization of the bladder was performed in 11 children from this subgroup.
In the second subgroup of 7 patients, 5 children underwent a delayed operation of primary closure after preliminary preparation and stretching of the bladder platform; no complications in the form of relapse of exstrophy were observed. A bladder fistula occurred in 1 (20%) child, which closed on its own 2 months after the intervention. Partial incompetence of the bladder neck was diagnosed in 1 (20%) patient. The remaining children retain urine for up to 20 minutes and urinate in portions. All these patients experience slow growth of bladder capacity.
As an example, we present a clinical observation of the treatment of a girl with classic bladder exstrophy and microcystis. The child was admitted to the clinic on the 5th day after birth. Considering the small size of the bladder platform, less than 30 mm (Fig. 5 A), it was decided to postpone the operation and begin stretching the bladder wall. At the age of 6 months. The bladder wall was punctured at 12 points with botulinum toxoid type A 100 U and, against the background of mechanical stretching of the bladder and botulinum therapy, it was possible to increase the size of the bladder (it was possible to immerse a 10 ml Foley catheter balloon into the pelvic cavity). The size of the bladder area increased to 50 mm (Fig. 5 B).
Rice. 5. A. - 5-day-old girl with classic exstrophy, microcystis, area size 28 mm. B. - the same child aged 8 months. after carrying out a set of measures to stretch the bladder wall. Fig. 5. A — female newborn 5 days old with bladder exstrophy, microcystis; the size of bladders plate – 28 mm. B – The same child at the age of 8 months after tension
At the age of 1.5 years, an operation was performed for primary closure of the bladder with bilateral replantation of the ureters with anti-reflux protection according to Cohen, plastic surgery of the bladder neck, bilateral iliac osteotomy of the pelvic bones according to Chiari with fixation of fragments with knitting needles, reduction of the pubic bones (Vicryl 2), plastic surgery of the anterior abdominal walls (Fig. 6 AD)
Rice. 6. A 1.5-year-old girl with classic bladder exstrophy and microcystis at birth. A. — view of the site before surgery after a set of measures to stretch the bladder. C. – stage of the operation of primary closure of the bladder; The ureters are moved to the bottom of the bladder, and the bladder neck is formed. D. is the result of primary closure of the bladder and bilateral osteotomy. Fig. 6. Female 1.5 yo with bladder exstrophy, microcystis, A, B – bladder's plate after tension, before surgery. C – surgery stage view; ureter replaced to the bottom of the bladder, bladders neck formed. D – view after primary bladder's closure and bilateral supra-acetabular osteotomy
The pelvic bones are additionally immobilized with a coxite plaster cast. The postoperative period proceeded smoothly. The child was discharged home on the 14th day. The plaster cast was removed on the 45th day. Kirschner wires were removed on the 50th day after surgery. The child urinates in 25 ml portions. Dry intervals 15-20 minutes.
DISCUSSION
There are different opinions on the timing of primary bladder closure. Some authors recommend surgery in the first days or weeks after birth. The main argument for justifying such early operations is the possibility of complete reduction of the pubic bones without performing an iliac osteotomy and the prevention of inflammatory changes and the development of polypous growths on the bladder mucosa [1-3, 5-7, 11-14]. Other authors insist on the possibility of performing these operations at the age of 2-4 months. and later [4, 5, 10, 15, 16]
It is known that children with bladder exstrophy, who did not undergo primary closure during the first year of life, and often a much longer period of life, did not have a decrease in kidney function, impaired patency of the ureters, any gross polypous growths and irreversible inflammatory changes mucous membrane of the bladder and urethra with proper care of the mucosa. There were no acquired orthopedic deviations of the hip joints, disturbances in gait or natural growth of the spine [1-3, 5, 7]. Our survey data confirmed these ideas. No renal dysfunction or expansion of the collector system was detected. We did not observe any irreversible changes in the bladder mucosa in children with primary or secondary exstrophy operated on at the age of 1-2-3 years and older (boy 12 years old).
An important prognostic factor is considered not only the size of the bladder area, but also the ability of the bladder wall to stretch (its elasticity) [1-3, 5, 6, 14-16]. It is also necessary to take into account the characteristics of the mucous membrane, the presence of granulations, dense, large polypous growths on its surface [14-16, 18-22]. With large bladder sizes, single polypous growths in individual areas of the mucosa are of no practical importance and can be excised. In children with microcystis of three centimeters, growths over an area of 2 cm² transform the entire functional surface of the vesical area of the bladder into dense, rigid tissue incapable of either stretching or contracting.
In most newborns, the bladder mucosa at birth does not have polypous growths and granulations; these inflammatory changes can occur if the mucous membrane is not properly cared for. Applying gauze pads with antiseptics (chlorhexidine, miramistin, etc.) contributes to changes in the mucous membrane - it becomes dense, loses its elasticity and ability to stretch. It is advisable to cover the surface of the bubble area with a thin (food) film of polyethylene with pinholes in the center. This method allows you to preserve the surface of the bladder from the traumatic effects of a diaper and clothing for a long period (up to 10-15 months or more), and prevents the occurrence of inflammation [18, 20, 22]. Children with exstrophy can take baths and showers and lead a normal lifestyle. Diaper rash on the skin, often occurring around the bladder, is not associated with exposure to urine, but is caused by fungal infections. The use of antifungal ointments (clotrimazole, mycoseptin, myconorm) and regular diaper changes can eliminate hyperemia, erosion and other irritations on the skin.
The high risk of postoperative complications, urinary incontinence in all patients with microcystis and the problems of poor growth (increase in volume) of the bladder in the future, the difficulty of performing effective plastic surgery of the bladder neck, and the increased number of re-operations forced us to abandon primary closure of the bladder in newborns in children. with a bladder area size of 3.0 cm or less. In the presence of pronounced polypous growths and granulations, combined with a lack of elasticity of the bladder tissue, we consider delayed treatment at the age of 6-18 months more preferable. or later, provided that the effect of stretching and increasing the size of the bladder area is achieved [18, 21-23].
If the cystic area cannot be stretched, we considered methods for correcting exstrophy using augmentation plastic surgery with a segment of the intestine [1-4, 22, 23]. Delayed primary closure of the bladder during exstrophy is performed quite often for various reasons and at various times [1-4, 11-13, 17, 21-23], but in the available literature we have not found a description of methods for gradual stretching of the bladder platform.
Preserving your own bladder and the ability to urinate independently with high-quality urinary retention is an extremely difficult problem for patients with microcystis. Difficulties arise in this group of patients during the formation of the urethra with mobilization of the corpora cavernosa of the penis due to the frequent formation of urethral fistulas in the cervical area [24]. It is very difficult to create a bladder neck in the absence of sufficient detrusor volume [25-29]. Some surgeons simply solve this problem, using intestinal plastic surgery even in infants [1-4, 17, 30]. Perhaps reducing the number of operations and preserving the psycho-emotional status of the child is important, but we should not forget that bladder augmentation operations are not so harmless and are also accompanied by a number of complications of the postoperative period and may require repeated surgical interventions. Scarring of the appendicostomy, rupture of the reservoir due to overflow, formation of stones in it, if the container is not properly washed of mucus, etc. are possible [1, 2, 4, 5, 8]. We believe that the formation of an intestinal reservoir or bladder augmentation is more preferable for children with exstrophy at an older age, when achieving high-quality urinary continence becomes socially significant for the child. In the first years of a patient’s life, it is important to try to preserve his own bladder and the ability to urinate independently, without the participation of adults in performing catheterization to empty the vesicointestinal reservoir.
Our experience in delayed operations allows us to determine the ability of a small bladder to stretch and grow, and methods of mechanical impact on the bladder wall in combination with injecting the bladder with botulinum toxin (BTA) can speed up this process. It is extremely difficult to achieve stretching of an already closed small-volume bladder without a formed neck. It takes several years and a series of complex operations to obtain noticeable results [1, 2, 5, 17, 22].
CONCLUSIONS
Thus, delayed primary closure of the bladder in children with microcystis after mechanical stretching of the bladder platform in combination with injection of the detrusor wall with botulinum toxoid type A can improve the results of correction of exstrophy in the most complex group of patients with small sizes of the bladder platform. In most clinical observations, it was possible to achieve accelerated growth of the bladder area with the prospect of developing the act of independent urination and improving the mechanism of urinary continence.
LITERATURE
- Purves JT, Gearhart JP. The bladder exstrophy-epispadias-cloacal exstrophy complex. In Pediatric Urology, 2nd edition. . Elsevier Inc 2010. P. 386-415. https://doi.org/10.1016/B978-1-4160-3204-5.00030-X.
- Gearhart JP, Jeffs RD. The bladder exstrophyepispadias complex. In Campbell's Urology, 9th ed. , Philadelphia: W. B. Saunders; 2007: 560.
- Cuckow P. The bladder-exstrophy-epispadias-complex. Essentials of Pediatric Urology. Volume Chapter 15, 2nd edition. London: Informa healthcare 2008. P.199-212.
- Menovshchikova L. B., Rudin Yu. E., Garmanova T. N., Shaderkina V. A. Clinical guidelines for pediatric urology-andrology. M.: Pero Publishing House, 2015 p. 196-219. .
- Mushtaq I, Garriboli M, Smeulders N, Cheria A, Desai D., Eaton S, Cuckow P. Primary bladder exstrophy closure in neonates: challenging the traditions. J Urol 2014;191(1):193-7. https://doi.org/10.1016/j.juro.2013.07.020.
- Rensley F., Barretini A. Strategy and tactics for the management of patients with bladder exstrophy. Pediatric urology. Modern surgical techniques: from the intrauterine period to puberty. Part 3. Bladder. [ed. M. Lima, G. Manzoni; lane from English edited by S.G. Vrublevsky]. M.: GEOTAR-Media, 2021, pp. 166-183. . Moscow: GEOTAR-Media, 2021. pp. 166-183 (In Russian)].
- Grady RW, Carr MC, Mitchell ME. Complete primary closure of bladder exstrophy. Epispadias and bladder exstrophy repair. Urol Clin North Am 1999;26(1):95-109. https:// doi.org/10.106/S0094-0143(99)80009-3.
- Pippi-Salle JL, Chan PT. One stage bladder exstrophy and epispadias repair in newborn male. The Can J Urol 1999;6(2):757–60.
- Kibar Y, Roth CC, Frimberger D, Kropp BP. Our initial experience with the technique of complete primary repair for bladder exstrophy. J Pediatr Urol 2009;5(3):186-9. https://doi.org/10.1016/j.jpurol.2008.11.005.
- Leclair MD, Faraj S, Sultan S, Audry G, Héloury Y, Kelly JH, Ransley PG. One-stage combined delayed bladder closure with Kelly radical soft-tissue mobilization in bladder exstrophy: preliminary results. J Pediatr Urol 2018;14(6):558- 64. https://doi.org/10.1016/j.jpurol.2018.07.013.
- Gargollo PC, Borer JG, Diamond DA, Hendren WH, Rosoklija I, Grant R, Retik AB. Prospective followup in patients after complete primary repair of bladder exstrophy. J Urol 2008;180(4 Suppl):1665-70. https://doi.org/10.1016/j.juro.2008.05.076
- Suson KD, Preece J, Baradaran N, Di Carlo HN, Gearhart JP. The fate of the complete female epispadias and exstrophy bladder – is there a difference? J Urol 2013;190(4 Suppl):1583-89. https://doi.org/10.1016/j.juro.2013.01.093.
- Zaman M, Kasprenski M, Maruf M, Benz K, Jayman J, Friedlander D., et al. Impact of pelvic immobilization techniques on the outcomes of primary and secondary closures of classic bladder exstrophy. J Pediatr Urol 2019;15(4):382.e1-382.e8. https://doi.org/10.1016/j.jpurol.2019.04.009.
- Alam A, Blachman-Braun R, Delto JC, Moscardi PRM, Castellan M, Tidwell MA, et al. Bladder exstrophy closure in the newborn period with external pelvic fixation performed without osteotomy: a preliminary report. J Pediatr Urol 2018;14(1);32-e1-32,e7. https://doi.org/10.1016/j.jpurol.2017.08.012.
- Nikolaev V.V. A less invasive technique for delayed bladder exstrophy closure without fascia closure and immobilisation: can the need for prolonged anaesthesia be avoided? Pediatr Surg Int 2019;35(11):1317–25. https://doi.org/10.1007/ s00383-019-04530-0.
- Rösch WH, Promm M. Bladder exstrophy: quality of primary care and long-term prognosis. Urologe A 2016;55(1):53-7. https://doi.org/10.1007/s00120-015-0010-4. (In German).
- Oesterling JE, Jeffs RD. The importance of a successful initial bladder closure in the surgical management of classical bladder exstrophy: analysis of 144 patients treated at the Johns Hopkins Hospital between 1975 and 1985. J Urol 1987;137(2):258-62. https://doi.org/10.1016/S0022-5347(17)43972-3.
- Rudin Yu.E., Sokolov Yu.Yu., Rudin A.Yu., Kirsanov A.S., Kartseva E.V., Medvedeva N.V. Scope of surgery for primary closure of the bladder in children with bladder exstrophy. Pediatric Surgery 2020;(1):21-28. .
- Rudin Yu. E. Epispadias and exstrophy of the bladder. In: Urology. National Guidance [ed. ON THE. Lopatkin]. M.: “GEOTAR Media”; 2009: 273-293. – Moscow: “GEOTAR media” Publisher house 2009: 273-293. (In Russian)].
- Rudin Yu.E., Marukhnenko D.V., Chekeridi Yu.E., Runenko V.I. Primary plastic surgery of the bladder for exstrophy in children. Pediatric Surgery 2009;(4):26-31. .
- Baradaran N, Cervellione RM, Stec AA, Gearhart JP. Delayed primary repair of bladder exstrophy: ultimate effect on growth. J Urol 2012;188(6):2336-42. https://doi.org/10.1016/j.juro.2012.08.037.
- Di Carlo HN, Maruf M, Jayman J, Benz K, Kasprenski M, Gearhart JP. The inadequate bladder template: its effect on outcomes in classic bladder exstrophy. J Pediatr Urol 2018;14(5):427.e1-427.e7. https://doi.org/10.1016/j.jpurol.2018.03.023.
- Ahn JJ, Shnorhavorian M, Katz C, Goldin AB, Merguerian PA. Early versus delayed closure of bladder exstrophy: a National surgical quality improvement program pediatric analysis. J Pediatr Urol 2018;14(1):27.e1-27.e5. https://doi.org/10.1016/ j.jpurol.2017.11.008.
- Rudin Yu. E., Marukhnenko D. V., Aliev D. K., Chekeridi Yu. E. Complex staged treatment of penile defects in boys with epispadias and bladder exstrophy. Experimental and Clinical Urology 2016;(4):128-36. .
- Inouye BM, Lue K, Abdelwahab M, Di Carlo HN, Young EE, Tourchi A, et al. Newborn exstrophy closure without osteotomy: is there a role? J Pediatr Urol 2016;12(1):51.e1-4. https://doi.org/10.1016/j.jpurol.2015.07.010.
- Novak TE. Failed exstrophy closure. Semin Pediatr Surg 2011;20(2):97-101. https://doi.org/10.1053/j.sempedsurg.2010.12.004.
- Frimberger D, Gearhart JP, Mathews R. Female exstrophy: failure of initial reconstruction and its implications for continent. J Urol 2003;170(6):2428-31. https://doi.org/10.1097/01.ju.0000090195.72919.f5.
- Varma KK, Mammen A, Venkatesh SKK. Mobilization of pelvic musculature and its effect on continuity in classical bladder exstrophy: a single-center experience of 38 exstrophy repairs. J Pediatr Urol 2015;11(2):87.e1-5. https://doi.org/10.1016/j.jpurol.2014.11.023.
- Khemchandani S.I. The long-term outcomes after staged repair of exstrophy-epispadias complex. J Indian Assoc Pediatr Surg 2016;21(4):158-163. https://doi.org/10.4103/0971-9261.186544.
- Osipov I. B., Kazachkov S. A., Smirnova L. P., Popova E. D. The choice of method of surgical treatment of bladder exstrophy. Urology and Nephrology 1996;(5):21-3. .
Topics and tags
Pediatric urology
Magazine
Journal "Experimental and Clinical Urology" Issue No. 4 for 2020
Comments
To post comments you must log in or register
Treatment of urogenital disorders
If the cause of urogenital disorders lies in a deficiency of estrogenic influences, then it is necessary to select adequate estrogen therapy . The use of local forms of estriol in the form of suppositories, ointments and gels is very effective. Unlike other types of estrogens, estriol “works” in the tissues of the genitourinary tract for only 2-4 hours and has no effect on the myometrium and endometrium. According to numerous studies, estrogen replacement therapy using vaginal administration of drugs containing estriol (for example, Ovestin) leads to an improvement in the condition of the mucous membranes of the urethra and vagina, an increase in the number of lactobacilli, a decrease in the pH environment of the vagina and helps eliminate infection.
In severe cases, surgical treatment can be used to correct urinary incontinence and pelvic organ prolapse.
Don't let your illness reduce your quality of life! Entrust the prevention and diagnosis of urogenital disorders to professionals! At MedicCity, the professional experience of the best gynecologists and other medical specialists is at your service!
Prevention
To prevent bladder astonia, preventive measures should be taken in relation to diseases that can lead to the first problem. For women, for example, this means following the rules of personal hygiene, avoiding hypothermia and infectious diseases.
This article is posted for educational purposes only and does not constitute scientific material or professional medical advice.