Bladder tumors are a common disease. The incidence in the countries of the European Union ranges from 11.7 cases per 100 thousand population in Ireland to 24.9 cases in Italy. In the CIS countries, the maximum indicators were registered in Ukraine - 15.0, Belarus - 14.0. In Russia this figure is 10.9 per 100 thousand population.
The increase in the prevalence of bladder tumors, which has been observed in many countries of the world over the past 20 years, is the result of the influence of unfavorable environmental factors, socio-economic conditions, as well as characteristics of demographic processes, including the aging of the population.
Transurethral resection (TUR) of the bladder is an endoscopic operation that is performed to remove a tumor (polyp) of the bladder, followed by microscopic examination of the resulting tissue.
What is the preparation for transurethral resection of the bladder?
To perform the operation, you will have to spend several days in the urological hospital (from 3 to 10). Before transurethral resection of the bladder, all patients must undergo blood tests (including for syphilis, HIV (AIDS) and hepatitis) and urine, electrocardiography (ECG), and a chest x-ray.
Patients are also examined by a therapist and an anesthesiologist, who determines the type of anesthesia (spinal, intravenous or general anesthesia). The evening before the operation, a cleansing enema is performed and the hair below the navel is shaved. From 0 o'clock on the day on which the operation is scheduled, you are not allowed to eat or drink. On the morning of the transurethral resection of the bladder, antibacterial therapy begins (intramuscular or intravenous antibiotics).
Benefits of Bladder Biopsy
Cystoscopy, a method of visually examining the bladder using a cystoscope, cannot provide all the answers. Obtaining reliable information is often hampered by hematuria or the turbid environment of the bladder, the presence of clots in it, and adenomatous prostate nodes protruding into the cavity. In addition, the results of cystoscopy are characterized by subjectivity and depend on the qualifications of the urologist conducting the endoscopic examination.
The main advantage of a biopsy is that histological analysis of the formation under study is the most reliable diagnostic method, which allows us to clarify the diagnosis and stage of the tumor process with 100% certainty.
Types of bladder biopsy
A bladder biopsy can be performed by removing a piece of diseased tissue during cystoscopy for further examination. The disadvantage of this diagnosis is the inability to determine the depth of damage to the walls of the bladder by the tumor process.
When performing a transuretal biopsy (TUR biopsy), the specialist tries to remove the entire tumor within healthy tissue. Despite the most pronounced diagnostic and therapeutic value of this technique, TUR biopsy can be accompanied by complications:
- hematuria;
- infection;
- perforation of the bladder wall, etc.
The quality of the study is largely determined by the qualifications of the urologist.
Recovery period
The nature of rehabilitation measures depends on the general condition of the patient and the volume of removal performed. Immediately after the intervention, bladder catheterization is performed. Depending on the condition of the bladder contents, it can be set for 2 hours or several days. The duration of bed rest is also decided on an individual basis. The result of a histological examination of the removed lesion is prepared within 3-5 days, after which the final treatment tactics will be developed.
In order to carry out a bladder biopsy with the highest quality possible, you can make an appointment with a urologist at City Clinical Hospital 31. Experienced clinic specialists will perform a cystoscopy, take a biopsy sample, or perform a complete resection of the tumor at the highest level, and highly qualified pathohistologists will reliably and within a short time clarify complex pathology. Timely initiation of treatment contributes to a more optimistic prognosis in the most severe pathology.
How is transurethral resection of the bladder performed?
Transurethral resection of the bladder is a high-tech intervention. During the operation, the patient lies on his back with his legs apart and bent at the knees. Through the external opening of the urethra, the doctor inserts a special instrument into the bladder - a resectoscope. All manipulations are performed under visual control. Using a resectoscope, the tumor is removed (“shaved off”) and the bleeding vessels are coagulated (cauterized).
If necessary, a biopsy of various parts of the bladder wall is taken. The resulting tissue is sent for consultation to a morphologist. At the end of the operation, a catheter (a hollow latex or silicone tube through which urine flows into a urinal bag) is installed into the bladder through the urethra.
results
After the procedure, the resulting tissue sample is delivered to the histology laboratory. In order for it to be examined under a microscope, paraffin blocks must first be prepared, cut into thin sections and stained. This process takes a relatively long time - up to 5-7 days.
At the final stage, the preparations go to a morphologist, who examines the bladder under a microscope and fills out a report. In it, the specialist reflects all the changes that he discovered. After this, the conclusion is transferred to the attending physician, who, in turn, begins planning treatment tactics.
Book a consultation 24 hours a day
+7+7+78
How does the postoperative period proceed?
It is possible that after the operation you will be installed with a system of continuous irrigation of the bladder (with a special solution or furacillin), when the flushing liquid enters through one of the internal channels of the catheter into the bladder and is released through another channel out into the urinary bag along with small blood clots. The duration of operation of such a system is determined by the doctor and can range from several hours to 2-3 days.
1.5-2 hours after the operation, in the absence of nausea and vomiting, you can drink (in small portions; until the evening you are allowed to drink approximately 1500 ml of still water). You can usually resume eating the next morning (sometimes in the evening of the day of surgery). For 7-10 days after surgery, avoid eating salty, fried, smoked foods, try to drink at least 2000-3000 ml of liquid per day (water, tea, fruit drink, juice, etc.). In any case, it is better to check your diet and fluid intake with your attending physician: it is possible that, due to any concomitant diseases you have or features of the operation, the doctor will give recommendations that differ from the above.
Antibacterial therapy usually lasts 5 to 15 days.
Removal of the urethral catheter is carried out after 1 - 5 days (on average - 2 days). After removing the catheter, the urine may be either light or mixed with blood. You may urinate frequently, in small portions, feel a burning sensation and pain in the urethra and perineum when urinating, and a strong urge to urinate. These phenomena are caused by the surgery and usually disappear within 7 to 14 days.
Episodes of blood in the urine can persist for up to 3 weeks, when the patient, as a rule, is already at home. In such a situation, you should increase the amount of fluid you drink and avoid heavy physical activity, and if you think that the bleeding is threatening, immediately contact your doctor by phone or (at night) go to the nearest urological hospital.
A conclusion from a morphologist on the results of a biopsy of a bladder tumor can be expected in 2-7 days (depending on where the histological examination is performed). You can find out the result of the biopsy and the final diagnosis from your attending physician.
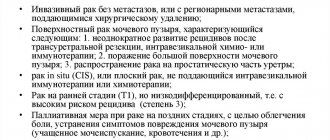
If a bladder tumor turns out to be malignant, additional treatment is often required - instillations (infusions) of various medications into the bladder (so-called “intravesical therapy”), about which you will be informed additionally. In some cases, the doctor may advise injecting some medicine into the bladder directly on the operating table, without waiting for a morphological response.
Forms of bladder cancer
The pathology, depending on the histological structure of the neoplasm tissue, may have one of the forms of cancer:
- Transitional cell carcinoma. Diagnosed in most cases. Neoplasia is found on the lining of the bladder and is limited to epithelial cells. It is easy to treat and does not spread beyond the affected organ.
- Squamous cell carcinoma. Formed from a glandular layer. Diagnosed in 2-3% of cases. May occur due to prolonged inflammation in the bladder.
- Adenocarcinoma. Formed from glandular tissue compounds. Occurs least often. More often it manifests itself in the form of papillary growths, easily spreading to the bones, liver, and lungs.
What are the possible risks and complications of the surgery?
Any operation, as well as anesthesia, is always associated with a certain risk of complications, including life-threatening ones, associated not only with your disease, but also with the individual characteristics and reactions of the body, which are not always possible to foresee.
The anesthesiologist will explain the possible risks of anesthesia to you.
Complications of the bladder tumor itself and transurethral resection include:
- Bleeding, which may require a blood transfusion or repeat surgery;
- Damage to the wall of the bladder or any abdominal organ, which necessitates immediate open surgery;
- Urinary infection (acute pyelonephritis, acute prostatitis, acute orchiepididymitis, sepsis);
- Subsequent formation of a stricture (narrowing) of the urethra;
- Recurrence of bladder tumor.
Indications and contraindications
A biopsy is prescribed to differentiate between benign and malignant tumors. These diseases may be suspected if the following symptoms are present:
- Presence of blood or pus in the urine.
- Acute urinary retention.
- Pain when urinating.
- Constant desire to empty the bladder.
This clinical picture may be characteristic of various diseases of the genitourinary system, so non-invasive diagnostic methods (ultrasound, X-ray, CT, MRI, PET-CT, etc.) are first prescribed. If the results of the study indicate oncology, the doctor may prescribe a biopsy, which will help confirm the diagnosis. Using this method, you can diagnose not only tumors, but also many other diseases, including:
- Precancerous diseases of the bladder (malakoplakia, leukoplakia).
- Ulcers, cysts, diverticula.
- Bladder polyps.
- Chronic cystitis, predominantly interstitial.
- Bladder tuberculosis.
Contraindications include acute inflammatory and infectious processes in the genitourinary tract, pathology of the blood coagulation system, damage to the urinary tract, urethral obstruction and some other diseases.
How to be monitored after surgery?
In most cases, after transurethral resection of the bladder, you should regularly contact a urologist to perform control cystoscopy (examination of the bladder with the eye using a special instrument on an outpatient basis) in order to timely detect possible tumor recurrence. The first cystoscopy is usually performed 3 months after surgery; It is advisable to check the timing of subsequent studies with your doctor.
To date, mitomycin C, doxorubicin, and immunomodulators based on the BCG vaccine have proven effective in preventing relapses and progression of bladder tumors.
The antitumor effect of BCG was first described by Holmgren. In 1966, Coe and Feldman showed that the bladder, like the skin, can develop a delayed immune response to antigen stimulation. First reported in 1976 by Morales et al. about successful local use by instillation of BCG for bladder cancer.
Examination and treatment of interstitial cystitis at URO-PRO
When visiting the URO-PRO clinic, a patient with interstitial cystitis
fills out special questionnaires (O'Leary-Sant, Analog Scale for Rating Symptoms of Interstitial Cystitis, urination diary).
Then a cystoscopy
under general anesthesia (intravenous or spinal).
If the diagnosis is “interstitial cystitis”
confirmed – the treatment plan is selected.
Treatment of interstitial cystitis
depends on the severity of the disease, but
the principles of treatment
always consist of:
- Symptomatic therapy;
- Pathogenetic therapy;
- Combating complications;
- Treatment of concomitant diseases.
Symptomatic therapy
interstitial cystitis is very important, since it is the symptoms of interstitial cystitis, such as pain when filling the bladder and frequent urination (pollakiuria), that make the patient’s life unbearable. There are various drugs to treat the symptoms of interstitial cystitis, m-anticholinergics, tricyclic antidepressants, serotonin reuptake inhibitors. An individual approach is required here; in addition, these drugs have serious side effects, so medical supervision is necessary. A new method of symptomatic treatment of interstitial cystitis is self-instillation. In Europe and the USA, self-catheterization of the bladder is widely used; there are special gel-coated catheters for this. The procedure is simple and painless, which can be performed several times a day. During self-catheterization, patients inject the drug Urolife (sodium hyaluronate) into the bladder, which protects the bladder wall from the irritating effects of urine and reduces inflammation in the urothelium.
Pathogenetic therapy
interstitial cystitis is aimed at the processes underlying this disease. One of them is the destruction of the protective membrane of the bladder, the so-called. glycosaminoglycan layer that covers nerve endings in the urothelium. This results in constant exposure of urine to receptors in the urothelium, causing pain and frequent urination. The glycosaminoglycan layer of the bladder consists of hyaluronic acid, chondroitin sulfate, heparan sulfate. To restore it, instillations of hyaluronic acid and/or chondroitin sulfate into the bladder are used. In addition, with prolonged exposure to urine on the nerve endings of the bladder, they become more sensitive and even in the absence of exposure generate pain. This phenomenon is called “peripheral nervous system sensitization” and underlies any chronic pain syndrome. To treat hypersensitivity of the bladder, we use injections of botulinum neuropeptide (BOTOX) into the so-called. Lieto triangle. This is the area of the bladder responsible for the perception of pain. A BOTOX injection, which is performed through a cystoscope using a special needle, helps reduce the increased sensitivity of the receptors in Lieto's triangle.
Combating complications
interstitial cystitis is also an important part of therapy.
One of the most severe complications of interstitial cystitis is spasm of the pelvic floor muscles,
the so-called. myofascial pain syndrome. Its essence is that in response to pain in the bladder, the pelvic muscles reflexively contract, and since the pain continues, they cannot relax on their own. Muscle spasms cause additional pain in the perineum, anus, lower abdomen, and sometimes even in the lower extremities. Physiotherapy and osteopathic methods are used to relax spasmed muscles. In addition, BOTOX injections are used using the UroTENS electromyograph - a joint development with the company FUJI DYNAMICS.
With interstitial cystitis, irritable bowel syndrome develops in 50% of cases. To diagnose and treat irritable bowel syndrome, the URO-PRO clinic has a qualified gastroenterologist, “sleep” colonoscopy and virtual colonoscopy.
The URO-PRO clinic actively cooperates with foreign clinics specializing in the treatment of interstitial cystitis; our specialists participate in international congresses. An example is the ESSIC 2021 congress in Budapest, where we presented the report “Comparison of efficacy of intravesical, oral and combined GAG-replenishment therapy as Painful Bladder Syndrome treatment modality.” as a therapy for Painful Bladder Syndrome").
Interstitial cystitis is an extremely severe and difficult to treat disease. We cannot promise that we will completely cure all of our patients from it. But we guarantee that the methods of diagnosis and treatment of interstitial cystitis used in the URO-PRO clinic meet the standards of the best European clinics, which means that we will improve the quality of life of our patients and most of them, after a course of treatment for interstitial cystitis, will begin to live without pain !
Questionnaire for the assessment of painful bladder syndrome Questionnaire for the diagnosis of interstitial cystitis
Checked the article and commented