Urodynamic examination of the bladder is a set of diagnostic methods aimed at identifying diseases of the genitourinary system.
Unlike most diagnostic methods used in the presence of obvious pathology, UDI helps to detect hidden conditions that can develop into more serious complications.
During such a comprehensive diagnosis, the doctor receives a holistic picture of the organ being examined, including the dynamics of all its functions.
- Contraindications
Goals and indications for urodynamic study
Urodynamics refers to the general process of the bladder and related organs removing urine from the body. Thus, the purpose of a urodynamic study is to assess the storage and evacuation functions of the urinary system.
UDI methods are particularly accurate, which helps to reliably determine the probable preconditions for certain dysfunctions.
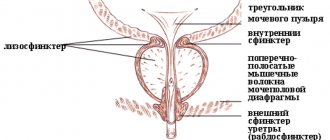
During a urodynamic study, the general sensitivity of the bladder is first determined, the work of the urethra is assessed when it is full, and possible overactivity of the detrusor, the muscular lining of the bladder, .
In addition, urethral resistance during urination and the amount of residual urine are measured. Based on the results obtained, the diagnosis is adjusted and specific treatment methods are selected.
As a rule, a urodynamic study of the bladder is prescribed if the following problems exist:
- Urinary incontinence during exercise or spontaneous muscle contractions.
- Involuntary leakage of urine with a strong urge to urinate.
- Rare or frequent urination.
- Difficulty or painful urination.
- Pain in the bladder area.
- Dullness or complete absence of a feeling of fullness of the bladder,
- Desuria.
- Polyuria.
- Chronic forms of diseases that are not amenable to conventional therapeutic effects (chronic pyelonephritis, cystitis, prostatitis, etc.).
Also, urodynamic examination of the bladder may be prescribed to patients before surgical operations related to the genitourinary system.
Who is recommended to take KUDI?
- in circumstances in which study findings may influence treatment choices, for example towards more invasive interventions for urinary incontinence and urogenital prolapse;
- after an unfavorable outcome of treatment, requiring more detailed information to choose further treatment tactics;
- as part of an early and long-term monitoring regimen for certain types of neurogenic dysfunction of the lower urinary tract;
- in patients with recurrent urinary incontinence, despite surgical treatment to eliminate it;
- with a sharp worsening of symptoms;
- in case of a combination of contradictory symptoms (for example, when urinary incontinence is combined with difficulty urinating);
- in neurological patients with the appearance of dysfunctions of the pelvic organs;
- for differential diagnosis of pathological conditions.
Features and methods of the procedure
A comprehensive urodynamic study (abbreviated CUDI) means an examination of the urinary tract. It is used in the diagnosis of diseases associated with dysfunction of this system.
KUDI includes a set of methods, such as:
- Uroflowmetry. Based on the study of the volumetric flow rate of urine.
- Cystometry. It involves determining intravesical pressure (requires filling the organ with sterile saline solution through a thin catheter). The procedure does not cause pain.
- Profilometry. This method is aimed at determining the pressure that is generated during urine retention through a catheter. They resort to profilometry to determine the nature of incontinence or difficulty urinating.
- Electromyography. This procedure is based on measuring the impulses that the nervous system sends. Prescribed in cases where the doctor suspects that physiological problems are caused by damage to soft tissues or nerves. This test measures muscle activity in the urethra and in the area around it.
- "Pressure-flow". This method simultaneously records 2 different indicators. Actually, it allows you to monitor the flow of urine and the pressure of the soft tissues of the detrusor.
The results of CUDI allow you to obtain information regarding the condition of the urinary organs and determine the causes of problems that have arisen.
Results of the procedure
A comprehensive urodynamic study allows us to detect the cause of urination disorders in the absence of any anatomical changes in the genitourinary organs. This examination is used in diagnosing the most complex cases of functional disorders of urine storage and excretion. This includes, for example, some forms of urinary incontinence (especially in women), problems with the innervation of the pelvic organs caused by diseases of the nervous system, etc. KUDI allows a specialist to accurately determine the existing pathology, and therefore select the most effective treatment regimen for a given patient.
Preparatory stage
Preparation for urodynamic examination of the bladder is carried out under the supervision of a physician. In this case, the general condition of the patient is taken into account, on the basis of which, among other things, decisions are made on the appropriateness of taking certain medications before UDI.
To establish a clear clinical picture, the patient is recommended to keep a urination diary for 5-7 days before the start of diagnostic procedures. It should record the time, frequency of urination and volume of urine. It is also advisable to make notes about the liquid you drink.
Urodynamic study
Urodynamic diagnostics studies the movement of urine through the lower parts of the urinary system
It is an important part of the examination not only in urology, but also in other branches of medicine: gynecology, neurology, pediatric practice, general surgery, geriatrics. Unfortunately, these research methods are not carried out in all clinics, although they provide valuable diagnostic information
Complex urodynamic study (CUDI) includes the following methods:
- uroflowmetry;
- cystometry;
- urethral profilometry;
- electromyography.
Urodynamic study is especially indicated for urinary incontinence, interstitial cystitis, and neurogenic bladder.
To carry out these studies, special sensors are placed in the bladder and urethra to record changes in pressure and catheters that supply and drain fluid. Due to the invasiveness of some of the urodynamic testing procedures, the advisability of their use in all patients is discussed.
Uroflowmetry is a non-invasive determination of the speed, volume and time of urination. It suggests the presence of pathology, but cannot clarify its location.
Cystometry shows changes in intravesical pressure when it is filled with a neutral solution through a catheter. It helps to diagnose a violation of the contraction of the muscular wall of the bladder, characterizes the state of the nerve pathways responsible for the formation of the urge to urinate. Cystometry shows the distensibility of the bladder, its hyperreactivity, but does not assess the condition of the urethra.
Mitration cystometry is carried out during urination and helps to identify such important characteristics as the contractility of the bladder muscle, the presence of obstacles to urination, and the coordination of the actions of the muscular wall of the bladder and the urethral sphincter.
Electromyography provides information about the coordination of all parts of the bladder during its filling and emptying.
Profilometry of the urethra - recording the pressure created by its walls. This method allows you to clarify the causes of urinary incontinence.
KUDI allows you to evaluate urinary disorders, establish a diagnosis, and determine treatment tactics. As a result of identifying 7 forms of urination disorders based on the results of CUDI, conditions such as cerebrovascular accident, multiple sclerosis, Parkinson's disease, spinal cord diseases, polyneuropathy (for example, in diabetes mellitus), discirculatory encephalopathy, vertebrobasilar insufficiency can be diagnosed. The listed diseases of the nervous system cause urinary disorders, the cause of which is usually searched for a long time and unsuccessfully by urologists, without resorting to this study.
For overactive bladder, neurophysiological testing of somatosensory evoked potentials and brain imaging are also useful. Such a comprehensive analysis will help to accurately determine the cause of frequent urination for no apparent reason. He will evaluate how much the functioning of the bladder is controlled by the brain. A neurologist can prescribe these research methods.
Types of research
Urodynamic studies are divided into 2 types: inpatient and outpatient, depending on the location of the diagnosis.
Inpatient urodynamics
Traditional urodynamic testing is performed in the clinic. In this case, the doctor fills the bladder with a special liquid of a certain temperature through a catheter, regulating the speed of its passage through the urinary tract.
Standard urodynamic diagnostics include studies such as uroflowmetry, cystometry, cystoscopy, pressure-flow, electromyography, etc.
Outpatient urodynamics
Outpatient urodynamic study of the urination process is carried out on an outpatient basis. In this case, the natural process of filling the bladder and eliminating urine is examined.
The patient needs to keep a special diary in which he records how much fluid is consumed per day and how much is excreted from the body.
The duration of keeping a diary is 2-3 days. The method allows you to assess the functional volume of an organ.
Advantages and disadvantages
Cystostomy as a method of urine removal has its pros and cons. If we talk about the advantages of cystostomy, we can note the following points:
- catheterization and evacuation of urine through a tube in the abdomen does not have a negative effect on the urethra, but with prolonged excretion of urine through a regular catheter, complications arise - in this, a suprapubic cystostomy definitely wins;
- the location of the urethral balloon near the neck of the bladder inevitably leads to further leakage of urine and its removal out along the outer walls of the catheter, which does not occur with a cystostomy;
- careful handling of the catheter significantly reduces the risk of it being pulled out;
- when the suprapubic catheter is obstructed, there are additional ways - the outflow of urine can be established through the urethra (very often such catheterization is carried out urgently if the patient cannot cope with the maintenance of the epicystostomy on his own);
- when installing a suprapubic cystostomy, men have the opportunity to be sexually active;
- It is easier for patients to maintain a catheter at the level of the suprapubic zone than below - caring for a cystostomy is possible without outside help, which cannot be said about catheterization through the urethra;
- the procedure for applying a cystostomy is not traumatic - if it is necessary to remove the tube from the bladder, then after the stoma a small scar remains, almost invisible;
- To prevent the possible consequences of tube blockage, a larger diameter, more suprapubic catheter can be used, which cannot be inserted into the urethra.
Disadvantages of the procedure
Cystostomy also has disadvantages that should also be taken into account when installing it:
- in patients in the area where the cystostomy is applied, skin sensitivity increases, but most patients note that the discomfort goes away after a while;
- if a cystostomy is used incorrectly, there is a possibility of pushing the tube into the urethra and damaging it, but such cases are rare;
- some men may have problems with installation if they have significant body weight or fat deposits in the suprapubic area;
- the place where the tube is installed sometimes gets wet - this can be easily eliminated if you apply a bandage, but in other patients the wetting stops on its own;
- in rare cases, a suprapubic catheter causes spasmodic contractions of the bladder;
- there is still a risk of tube clogging, so men should carefully care for the system;
- According to some patients, cystostomy is less convenient than frequent catheterization, but this point of view is subjective.
Analysis of urine
Morning urine accumulated overnight is best suited for laboratory research - its analysis provides the most objective data. A general urine test allows you to determine the presence of abnormalities associated with inflammatory processes, identify the pathogen, and also detect long-term signs of some diseases not related to the genitourinary system.
Features of preparation
Typically, KUDI does not require compliance with any special rules or preliminary measures. However, it is recommended to undergo a general urine test before the procedure. Against the background of its results, it is possible to determine or exclude the occurrence of inflammatory processes in the body at the time of the urodynamic study.
Before the manipulations themselves, you will need to cleanse the body and perform genital hygiene. Women need to monitor their cycle; KUDI is not performed during menstruation.
In some cases, after an examination, the doctor may prescribe a short-term course of antibiotics to prevent inflammatory processes.
Urodynamic study
If a person has complaints and the doctor suspects any pathologies of the genitourinary system, then a urodynamic study is prescribed. Proper preparation is necessary to avoid skewed results. Let's consider a urodynamic study - what it is and how it is done.
Indications
The purpose of the bladder is to store urine and release it. If these processes are disrupted, unpleasant symptoms appear. The patient comes with them to see the doctor.
After collecting an anamnesis, a urodynamic examination is prescribed, thanks to which the doctor will see the condition of the organ and channels that excrete urine.
After the manipulations, it will be possible to begin treatment, since the diagnosis becomes immediately clear.
Find out what problems this procedure can help solve:
- inability to hold urine;
- difficulty passing urine;
- loss of sensitivity of the organ when there is no urge to go to the toilet;
- inflammatory pathologies.
Procedures
Urodynamic studies - what they are - can be understood by learning about their types.
- Standard examination. It is also called stationary. It is necessary to obtain data on the pressure in the bladder.
- Diagnostic type of examination. In this case, the bladder is filled with a special solution. The results are more accurate.
- Outpatient view. The doctor examines the filling of the bladder, as well as its ability to empty.
Patients often ask where - what kind of examination is this? The deciphering of the abbreviation sounds like a complex urodynamic study. It includes several diagnostic methods, thanks to which the doctor can get a complete picture of the disease. Below we will look at all of them.
If you ask a doctor how a comprehensive urodynamic study is done, he will definitely tell you to keep a diary first.
In addition to indicating the number of urges and the volume of urine excreted over 5-7 days, it is also necessary to indicate how much fluid was drunk per day. The patient also writes down his feelings.
Thanks to this information, it is easier for the doctor to choose the right method of examination, and subsequently treatment.
Pressure
Tests of urine flow and pressure are called “pressure-flow”. With its help, a specialist will be able to figure out what pressure is created in the organ during urination. The rate of urine output itself is also assessed.
During the examination, two types of pressure are obtained - inside the bladder and outside. The doctor will see how active the bladder is and whether there are any pathological changes.
Volume
CUDI (complex urodynamic study) is impossible without determining the residual urine. For this purpose, either an invasive method is used, which involves inserting a catheter, or residual urine is examined using an ultrasound machine.
The first option is rarely used, because the manipulations are quite traumatic and painful. During these procedures, the position of the bladder is carefully monitored.
Having received information on the monitor, the doctor calculates the necessary parameters using special formulas.
Urofluometer
This diagnosis is important for urinary incontinence that occurs either due to surgery or due to some disease. To carry out the procedure, you need to insert a catheter into the bladder, and a balloon equipped with a catheter into the rectum.
To monitor urine output, a uroflowmeter device is needed, and a video urodynamic study is also immediately performed. A device that sensitively reacts to the onset of urination is also relevant here. The doctor injects the solution into the bladder until the patient can tolerate it. All of these devices will eventually show the data necessary for analysis.
Urofluometry
Urofluometry is a relatively simple diagnostic test that measures the rate of urination and the volume of urine excreted. An hour before the start of the procedure, the subject must drink at least one liter of liquid.
Measurements are carried out using special equipment that records all the required parameters. The patient can perform the necessary manipulations in private on his own by pressing the start button of the urofluometer when ready to urinate. Data in the form of graphs is displayed on the computer screen.
Contraindications for performing CODI
A comprehensive urodynamic examination, like any other diagnostic procedure, cannot be performed on everyone.
Contraindications include infectious inflammation of the lower urinary tract (including the urethra) in acute form.
Other contraindications include the presence of neoplasms in the lower urinary tract and congenital anatomical pathologies.
Cystometry
With this examination method, such parameters of the bladder as capacity, sensitivity of its walls, intravesical pressure in the empty and filled state, as well as the functional characteristics of the detrusor and urethra are studied.
Using cystometry, you can determine the presence of pathological conditions such as detrusor hyperreflexia (the occurrence of detrusor contractions when there is a relatively small amount of fluid in the bladder) or detrusor areflexia (the absence of detrusor contractions when the bladder is full).
Recently, new scientific studies of the morphology of the muscular layer of the bladder and the development of diagnostic technologies have contributed to the wider use of cystometry in clinical practice.
The technique itself is as follows. At the beginning of diagnostic procedures, the patient is asked to empty the bladder. Urofluometric measurements can be taken during urination. After this, an isotonic saline solution is injected into the organ being examined through a catheter connected to a cystometer.
In some cases, carbon dioxide is used as a filling substance. The cystometer should detect the occurrence of the first urge to urinate - as a rule, it appears when about 200 ml is administered. liquids _ The cystogram then records the maximum volume of the bladder, determined by the greatest intensity of urge.
With maximum fullness of the bladder and normal functional state of the muscular membrane, a person, by force of will, can maintain a contraction of the detrusor for 50 seconds .
At this stage, if necessary, to excite the detrusor reflex and clarify the full clinical picture, the patient should move a little, after which he is allowed to urinate.
When urinating, the cystometer records the increase in pressure caused by contraction of the bladder muscles. At peak pressure levels, the patient must again suppress detrusor contraction. The bladder can then be emptied completely.
Methodology:
When performing KUDI
Thin sensor catheters are inserted into the patient's bladder and rectum to measure bladder and intra-abdominal pressure. Next, the bladder is filled with saline at a certain speed (through a bladder catheter).
At the same time, pressure in the bladder is recorded (bladder reactivity), and provocative tests (for example, cough) are performed. Upon achieving an adequate urge to urinate, the patient is asked to urinate into a special device - a uroflowmeter, which allows one to assess the volumetric rate of urination. When urinating, the adequacy of the contractile function of the bladder and the presence/absence of organic or functional obstacles to the flow of urine are assessed. The KUDI procedure may cause slight discomfort, but it is absolutely painless.
If you want to get even more information about Urodiamic examination, we recommend watching the video report of the doctor of our center Zaitseva A.O.
Who is prescribed KUDI
The doctor recommends a CUDI test if symptoms indicate problems with the lower urinary tract. Lower urinary tract symptoms include:
- Urine leakage;
- Frequent urination;
- Painful urination;
- Sudden strong urge to urinate;
- Problems related to urine flow;
- Inability to completely defecate;
- Recurrent infections.
But in order to schedule a procedure, you should make an appointment with a urologist who will determine the indications for the procedure and, if necessary, prescribe additional tests.
What can prevent you from performing KUDI?
UROSCREEN device
- frequent urination, accompanied by an imperative (uncontrollable) urge to urinate;
- rare, difficult urination (you have to strain and squeeze out urine), absence or weakening of the feeling of filling the bladder, the urge to urinate;
- urinary incontinence due to the occurrence of an imperative (uncontrollable) urge to urinate, at the sound of pouring water;
- urinary incontinence that occurs during physical activity, straining, coughing, laughing, running, sneezing, etc.
But first, you need to come for a consultation with our specialist - a urologist or neurourologist, who will conduct a full examination, determine the indications for the study and, if necessary, prescribe tests before performing the procedure.
To perform CODI, our clinic uses a modern UROSCREEN device (made in Germany).
- measure urine flow rate - uroflowmetry
- study the functioning of the bladder - cystometry
- assess the relationship between bladder pressure and urine flow rate using a pressure/flow study
- determine the pressure in the internal lumen of the urethra necessary for urinary retention - profilometry of intraurethral pressure (3-D image)
- assess muscle function and the quality of transmission of nerve impulses along peripheral nerves and pathways of the brain and spinal cord - electromyography
- record and save the urodynamic study report on electronic media (electronic diagnostic patient record)
An insurmountable obstacle along the urethra in men (narrowing, urethral stricture, large size of the lateral lobes of the prostate with hyperplasia, contraction of the bladder sphincter, etc.)
- Urodynamic studies (cystometry, pressure-flow studies) should not be performed in patients with an active urinary tract infection.
- Movement and active conversations during urodynamic studies can lead to distortion of recordings and, as a consequence, test results.
- Taking certain medications may change the results of urodynamic tests. Tell your doctor if you are taking any medications, herbs, or supplements; You may be advised to stop taking some of them before the test.
- It is advisable for pregnant women not to resort to such procedures.
Cystoscopy
Cystoscopy is an endoscopic method for examining the inner surface of the bladder. The procedure helps to identify the presence of pathological formations such as inflammation, foci of infection, tumors, etc. inside the organ under study, as well as to recognize some renal complications.
This method allows you to visually examine the bladder itself, the urethra and the ureters.
Cystoscopy is performed using endoscopic equipment, which includes a catheter with lighting and optical devices. The cystoscope is inserted into the bladder cavity through the urethra. To reduce sensitivity during such manipulations, local anesthesia is used. If necessary, general anesthesia or spinal anesthesia may be used.
On average, a cystoscopy session lasts 30 minutes . However, with a rigid or fibrocystoscopic type of examination, when it is necessary to perform a biopsy or surgery, this may take up to two hours.
Often, after a cystoscopic examination, patients experience aching pain, burning or stinging when urinating. Typically, such symptoms subside within a day, otherwise you should consult a doctor.
Preparing for the examination
A bowel movement is required before the test. If this cannot be done naturally, it is recommended to give an enema.
In addition, it is necessary to empty your bladder and not drink any liquid for an hour before the test.
Before a urodynamic study, the patient must undergo the appropriate tests and appear on the appointed day with the results:
- ultrasound examination of the bladder, kidneys, prostate (for men);
- general urinalysis;
- bacteriological examination of urine;
- blood test for prostate specific antigen (for men).
Before and after the study, the patient must take antibiotics, which helps prevent the development of infection. No other preparatory activities are provided.
How to prepare for research?
- On the eve of the study day, in the evening at 22-00, drink Monural 3 g (a broad-spectrum antibacterial agent) - in order to prevent infectious and inflammatory complications.
- In the evening, do a cleansing enema or have an independent bowel movement in the morning (cleanse the rectum of feces) in order to avoid artifacts (incorrect results) of intra-abdominal pressure values.
- Fasting is not required for the study.
- If you are scheduled for a pressure-flow study, you must shave your perineum (in the anus area) the day before the test, because Recording sensors are placed in this area to assess the function of the pelvic floor muscles.
How is KUDI carried out?
Urodynamic studies are divided into several types, each of which has its own specific procedure:
- Uroflowmetry. The person is taken into a special room where a research device is installed. After the doctor gives the command, the patient should begin to urinate within 5 seconds. To improve the accuracy of the results, you must remain still. There is no need to strain your muscles while urinating. The duration of the test is no more than 10 minutes.
- Cystoscopy. The diagnostic procedure is carried out using a cystoscope - a thin tube with an optical system for displaying images on a monitor screen. A special instrument is inserted into the urethra, through which they enter the bladder cavity. Cystoscopy allows you to get a real picture of the condition of all parts of the bladder.
- Cystometry. After emptying the bladder, the patient needs to lie down on the couch. The doctor then inserts a thin, soft tube (catheter) through the urethra and into the bladder. After removing residual urine, the catheter is connected to a device - a cystometer. It helps measure the pressure level in the organ. Then, a saline solution is injected into the bladder through a tube and wait until the patient has a desire to void. After this, the liquid is stopped, and the person is asked to urinate into the uroflowmeter. The duration of the procedure is no more than 45 minutes.
- Determination of pressure level in the urethra. A thin soft tube is inserted through the urethra, which is attached on the reverse side to a special device that controls the pressure level. Next, liquid is passed through the catheter, while a sensor measures the pressure inside the urinary canal. The duration of the procedure is no more than 15 minutes.
- Electromyography of the bladder. Based on the diagnostic results, the work of the muscles of the organ, as well as the urethral sphincters (internal and external), is assessed. Electrodes are applied to the muscles, examining their contraction at rest and at the moment of stimulation of the corresponding muscles. There are no restrictions for the study. In addition, the diagnosis does not require preliminary preparation.
Other urodynamic studies are no less simple and safe. In addition, if the diagnosis is carried out by a qualified doctor, it will be possible to avoid discomfort during the procedure and the development of complications.
How is the procedure done?
The KUDI program involves a number of analytical procedures, the selection of which is carried out in each individual case based on the results of previous laboratory tests and medical history. A complete urodynamic study of the bladder includes the following:
- Urinalysis This procedure consists of identifying substances in urine that may indicate the presence of various pathologies. For example, protein or blood cells in the urine indicate kidney problems, white blood cells and a number of bacteria indicate inflammation and infections, and glucose indicates the presence of diabetes.
- Cystoscopy During this procedure, an ultra-thin biometric instrument, a cystoscope, is inserted into the cavity of the urethra and bladder, which makes it possible to examine these organs from the inside.
- Cystometry One of the most popular methods of complex urodynamic research, during which the bladder itself is studied. The doctor inserts an ultra-thin catheter into the organ, through which the organ is filled with saline solution. During the procedure, the level of pressure in the organ, the moment when the urge to empty it appears, as well as its maximum volume are assessed. This manipulation is absolutely painless.
- Urethral profilometry is necessary to determine the level of pressure required to retain urine within the walls of the urethra using a catheter. It is profilometry that makes it possible to find out the main cause of difficulties in emptying the bladder or urinary incontinence.
- Uroflowmetry Using a special electronic measuring device, this procedure determines the rate of emptying and the amount of urine excreted.
- Ultrasound During the study of CUDI, ultrasound makes it possible to determine the general condition of the urinary tract and the bladder itself.
- Studying the residual volume of urine After complete natural emptying, a thin catheter is inserted into the bladder to determine the volume of remaining fluid in it. Sometimes the residual volume is determined by ultrasound.
- Stress Test To accurately test the symptoms of urinary incontinence, the patient will need to perform certain physical actions, such as laughing or coughing.
- “Pressure-Flow” technique This procedure allows you to simultaneously record the pressure of the flow of urine and the muscle tissue of the bladder.
To date, CUDI is the only technique that makes it possible to make an accurate urodynamic diagnosis and exclude the functional etiology of urinary disorders. When performing surgical treatment of urinary incontinence or other diseases of the urinary system, this study is mandatory in many clinics. The price of a urodynamic study depends on the set of measures included in it and can reach 25 thousand rubles.