Tuberculosis of the genitourinary organs
Mycobacterium tuberculosis (MBT) is a facultative intracellular parasite. Mycobacterium tuberculosis (MBT) belongs to the family of bacteria Micobacteriacae, order Actinomycetalis, genus Mycobacterium. The genus Mycobacterium has over 100 species, most of which are saprophytic microorganisms widely distributed in the environment.
Etymologically, the word “mycobacterium” comes from the Greek words myces - mushroom and bacterium, bactron - stick, twig. The "mushroom" component of the name comes from the tendency of these microorganisms to form filamentous and branching mold-like forms.
From the standpoint of clinical medicine, Mycobacterium tuberculosis, discovered by the German scientist Robert Koch, is the most important type of actinomycetes, which are united in a complex that includes M. tuberculosis (MBT); M. bovis and its variant BCG (Bacillus Calmette-Guerin); M. africanum and M. microti. This group of mycobacteria is distinguished by pronounced genetic similarity.
M. microti is considered non-pathogenic to humans, but causes a disease in mice resembling tuberculosis. BCG culture is not pathogenic for humans. Mycobacterium tuberculosis (MBT) is the cause of human tuberculosis in up to 95% of cases, depending on the area of residence. However, M. bovis and M. africanum cause a disease in humans that is clinically no different from classical tuberculosis.
Mycobacteria not included in the M. Tuberculosis complex can cause mycobacteriosis. Such mycobacteria are combined into complexes, the most important of which are: M. avium, M. fortinatum and M. terrae, M. leprae, M. ulcerance.
The materials presented below on tuberculosis are relevant only to the disease caused by M. tuberculosis (MBT) - Koch bacteria (KB), typus humanus.
The natural reservoir of mycobacterium tuberculosis is humans, domestic and wild animals, and birds.
MBTs are externally thin, curved sticks that are resistant to acids, alkalis and drying. The outer shell of the bacterium contains complex waxes and glycolipids.
MBT can multiply both in macrophages and outside cells.
MBT reproduce relatively slowly. Reproduction occurs mainly by simple cell division. On enriched nutrient media, MBT multiply with a doubling period of 18 to 24 hours. For growth in culture of Mycobacterium tuberculosis obtained in clinical conditions, it takes 4 to 6 weeks.
The genetic structure of MBT has been established. The nucleotide sequence of MBT can be found in international data banks. The nucleotide sequence of MBT (strain H37Rv) is 4,411,529 bp
MBTs do not have independent movement. Temperature limits for growth are between 29 and 42 °C (optimal - 37-38 °C). MBT are resistant to physical and chemical agents ; they remain viable at very low temperatures, and can withstand increases up to 80 °C for 5 minutes.
In the external environment, Mycobacterium tuberculosis is quite stable. It can survive in water for up to 150 days. Dried mycobacteria cause tuberculosis in guinea pigs after 1-1.5 years, lyophilized and frozen are viable for up to 30 years.
With intense sun irradiation and high ambient temperatures, the viability of MBT decreases sharply; on the contrary, in darkness and dampness their survival rate is very significant. Outside a living organism, they remain viable for many months, especially in dark, damp rooms.
MBTs are detected by a unique staining property (acid fastness), which distinguishes them from many other infectious agents. Ziehl and Neelsen in 1883 developed a special contrast method for staining MBT, based on the property of acid resistance. Unlike non-acid-fast bacteria, tuberculous mycobacteria are stained red, do not discolor when exposed to an acid solution, and are clearly visible against a blue background under microscopy. The Ziehl-Neelsen method is still one of the main methods for staining MBT during microscopy. More sensitive than the acid-fast staining method is MBT auramine staining followed by fluorescence microscopy.
The lipid fraction of the outer shell of MBT is associated with the resistance of tuberculosis pathogens to acids, alkalis and alcohols.
Variability of MBT morphology. The morphology and size of the office are not constant; it depends on the age of the cells and especially on the living conditions and composition of the nutrient medium.
Cord factor. Lipids in the surface wall of mycobacteria determine its virulence and ability to form clusters of bacteria in the culture in the form of braids (cord factor).
The cord factor was already mentioned by Koch in his initial message regarding MBT. Initially, the cord factor was associated with the virulence of MBT. The ability to form braids is observed among other mycobacteria that have low or no virulence. The cord factor, as it was later established, is associated with an unusual biological substance trehalose 6,6-dimyco-late, which is highly virulent.
L-shape. One of the important types of MBT variability is the formation of L-forms. L-forms are characterized by a reduced level of metabolism and weakened virulence. Remaining viable, they can remain in the body for a long time and induce anti-tuberculosis immunity.
L-forms are distinguished by pronounced functional and morphological changes. It was found that the transformation of MBT into L-forms increases with prolonged exposure to antibacterial therapy and other factors that disrupt their growth and reproduction, and the formation of the cell membrane.
It has been established that the sputum of “abacillary” patients with destructive forms of tuberculosis may contain L-forms of MBT, which, under appropriate conditions, can reverse (modify) into a rod-shaped variant, thereby causing reactivation of the tuberculosis process. Consequently, abacillation of the cavities of such patients does not yet mean their sterilization with respect to MBT.
MBT by its nature is insensitive to many antibiotics. This property is primarily due to the fact that the highly hydrophobic cell surface serves as a kind of physical barrier to therapeutic agents and antibiotics. The main reason for resistance is encoded in the structure of the genome of the tuberculosis bacillus.
At the same time, MBT can develop resistance (resistance) to anti-tuberculosis drugs. In recent years, simultaneous drug resistance of MBT to several drugs has significantly reduced the effectiveness of tuberculosis treatment.
As a result, modern healthcare deals not just with the dangerous pathogen of tuberculosis, but with a whole set of its strains that are resistant to various drugs. In practice, to organize effective treatment of tuberculosis, it is important not only to detect MBT, but also to simultaneously determine their resistance, and quickly enough - within two to three days - in order to prescribe effective chemotherapy in a timely manner.
At the end of the 80s. In the last century, a method has emerged that significantly reduces the time of such analysis. New diagnostics are based on selective amplification of nucleic acids (DNA or RNA) in vitro using polymerase chain reaction (PCR).
The PCR method has great potential and underlies precise DNA diagnostics, which allows one to identify any MBT strain and determine the root cause of a particular drug resistance.
Laboratory studies have shown that the emergence of resistance in M. tuberculosis is associated with nucleotide substitutions (mutations) in genes encoding various enzymes that directly interact with drugs.
The resistance of some MBT strains to isoniazid is associated with mutations in the katG gene, leading to the replacement of some amino acids in the enzymes catalase and peroxidase.
MBT insensitivity to streptomycin is associated with a missense mutation in the rpsL gene, encoding the S12 mitochondrial protein, or with nucleotide substitutions in the rrs gene, encoding 16S RNA.
Source of infection. The main source of MBT is a person with tuberculosis who spreads MBT (bacillus shedding) .
The focus of tuberculosis infection becomes dangerous in cases where patients suffer from an open form of tuberculosis, i.e. secrete mycobacterium tuberculosis. Of particular importance when infected with tuberculosis is direct, long-term and close contact of a healthy person with the bacilli shedding agent. Infection can most often occur in a family, place of residence, or group where there is a patient with tuberculosis who secretes mycobacteria. The danger of dispersal of the infectious principle is eliminated if the bacilli-releasing agent is promptly identified and isolated.
The occurrence and course of infection depend not only on the virulence of the pathogen, but also on the state of resistance and reactivity of the macroorganism.
Of great importance is the place of penetration of MBT into the body, where primary contact with the microbe is made (entry gate of infection). The following routes of transmission of tuberculosis are distinguished: 1) airborne; 2) nutritional (through the digestive tract); 3) contact; 4) intrauterine infection with tuberculosis.
Airborne transmission of tuberculosis Mycobacterium tuberculosis enters the air through droplets when a patient with active tuberculosis coughs, talks, or sneezes. When inhaled, these contaminated droplets enter the lungs of a healthy person. This method of infection is called airborne infection.
Depending on the strength of the cough impulses and the size of the droplets, MVTs spread in the air over different distances: when coughing - up to 2 m, when sneezing - up to 9 m. On average, sputum particles disperse over a distance of 1 m right in front of the patient.
Droplets of tuberculosis sputum that settle on the floor dry out and turn into dust particles. The tuberculous mycobacteria found in them remain viable in the dust for some time. It has been established that by the 18th day 1% of living bacteria remains in dried sputum. When there is strong air movement, sweeping the floor, or people moving, dust particles containing mycobacterium tuberculosis rise into the air, enter the lungs and cause infection.
Alimentary route of infection through the digestive tract Special experiments on animals show that the nutritional route requires a significantly larger amount of mycobacteria than aerogenic infection. If one or two mycobacteria are enough when inhaled, then hundreds of microbes are required for infection through food.
The ways of spread of tuberculous mycobacteria in the human body during alimentary infection with a tuberculosis culture are demonstratively shown by sectional materials published in connection with the trial in Lübeck. By mistake, 252 infants were given a tuberculosis culture (Kiel strain) instead of BCG during per os vaccination. As a result of infection, 68 children died from tuberculosis, 131 children fell ill and 53 remained healthy.
During the autopsy of the corpses of 20 deceased children, it was found that in most cases the process was localized in the abdominal organs.
The entry point for infection was the digestive organs.
One of the features of this route of infection in young children is the frequent involvement of mesenteric lymph nodes by tuberculosis.
It must be borne in mind that the penetration of tuberculous mycobacteria into the intestines can also occur when patients with pulmonary tuberculosis swallow their own bacillary sputum, which is confirmed by using the flotation method of gastric lavage water.
Contact transmission of tuberculosis Cases of infection through the conjunctiva of the eyes of small children and adults have been described; in this case, acute conjunctivitis and inflammation of the lacrimal sac are sometimes detected.
Infection of tuberculosis through the skin is rare. Cases of tuberculosis in milkmaids due to the penetration of MBT through damaged skin of the hands from cows with tuberculosis have been described.
Intrauterine infection with tuberculosis The possibility of infection of the fetus with tuberculosis during intrauterine life has been established in the section by cases of tuberculosis in children who died in the first days after birth. Infection occurs either when the placenta is affected by tuberculosis, or when the damaged placenta becomes infected during childbirth by a tuberculous mother. This route of infection with tuberculosis is extremely rare.
Immunity Morphological and biochemical components of a microbial cell cause various reactions in the body.
The main biochemical components of MBT are proteins, carbohydrates, and lipids. Proteins (tuberculoproteins) are the main carriers of the antigenic properties of MBT.
Tuberculin is one of the tuberculoproteins widely used in practice to detect MBT infection.
Delayed-type hypersensitivity (DSHT) Substances that make up the outer shell of the office induce a specific tissue inflammatory reaction of the macroorganism and the formation of granuloma. At the same time, delayed-type hypersensitivity (DHT), determined by the reaction to tuberculin tests, and weak antibody formation appear. Mainly, HCT is used to characterize the type IV immune response (the presence of induration that developed after 48 hours at the site of intradermal tuberculin administration) in individuals infected with MTB. However, HCT is associated with an immune response to factors that damage tissue.
Relationship between the immune response and pathogenesis Local and generalized tuberculosis damage in the body is determined by the protective reactions produced by the body's immune system against MTB. When describing this complex process, we will limit ourselves to a simple listing of the events that occur from the moment of the initial penetration of MBT into the alveoli until the results of the natural struggle between the macroorganism and the MBT. This process determines the fate of at least a third of the world's population that is infected with Mycobacterium tuberculosis.
The development cycle of tuberculosis from infection of the body with Mycobacterium tuberculosis to clinical manifestations of the disease and the spread of MTB in the environment can be divided into 5 stages.
Stages 1. Spread of infection (infection). 2. Onset of infection, proliferation and dissemination in the infected organism. 3. Development of the body's immune response. 4. Caseation (development of caseous necrosis) and accelerated reproduction of the office. 5. Secondary spread of infection (the ability to infect, infect).
Free consultation with a urologist
Tuberculosis of the genitourinary system develops in 15-20% of people with pulmonary tuberculosis. Tuberculosis of the genitourinary system is the second most common form of extrapulmonary tuberculosis, developing as a result of hematogenous spread of infection from primary pulmonary foci. Tuberculosis of the genitourinary system is equally common among men and women. The kidney is the first organ of the genitourinary system affected by tuberculosis; other organs of the urinary system, including the bladder, are involved in the pathological process secondarily, as a result of the direct spread of infection. Thus, tuberculosis of the bladder develops as a process secondary to tuberculosis of the kidney. Asymptomatic disease and diagnostic difficulties often delay the start of treatment, which leads to the development of severe complications such as kidney destruction, microcystitis, etc.
Who causes bladder tuberculosis?
Tuberculosis, including tuberculosis of the bladder, is caused by Mycobacterium tuberculosis - Koch's bacillus. This is an acid-fast bacterium that enters the human body through airborne droplets and, with reduced immunity, causes the development of tuberculosis.
Pathogenesis of bladder tuberculosis
As mentioned earlier, tuberculosis of the bladder develops against the background of tuberculosis of the kidney, and the infection spreads as follows: either by seeding the walls of the bladder with mycobacteria in the urine, or by submucosal spread of infection along the ureters from the kidney to the bladder. First of all, the triangle of the bladder is involved in the pathological process: granulomatous inflammation develops around the openings of the ureters, which ends with the formation of strictures of the part of the ureter passing through the wall of the bladder, or, conversely, the development of vesicoureteral reflux. With further spread of inflammation, the entire bladder wall quickly becomes involved in the pathological process (Fig. 1).
Fig.1. Pathological changes in the wall of the bladder in tuberculosis.
Tuberculous nodules (granulomas) form in the wall of the bladder, which can merge with each other, caseous necrosis develops, and numerous ulcers form. Ulcers can spread to the muscle layer of the bladder wall, causing damage and destruction of muscle fibers with the formation of fibrosis (scar changes). In this case, deformation of the bladder occurs, its volume decreases, resulting in the formation of contracture (sclerosis) of the bladder. Microcystitis (reduction of the bladder in size) is one of the most severe complications of bladder tuberculosis. Microcystitis is accompanied by vesicoureteral reflux (sometimes reaching the kidney), which impairs renal function. In rare cases, when the inflammatory process is severe, the ulcer spreads to all layers of the bladder, causing perforation of the wall, penetration of nearby organs and the formation of fistulas, such as a vesico-rectal fistula. If the fistula is located at the top of the bladder, it can open into the abdominal cavity, causing the development of the “acute abdomen” symptom complex.
Symptoms of bladder tuberculosis
As a rule, the symptoms of bladder tuberculosis at the onset of the disease are nonspecific. A person is worried about loss of appetite, even anorexia; weight loss, weakness and fatigue, night sweats. However, later signs of damage to the urinary system appear.
Dysuria is a problem with urination. Patients experience an increase in urination from 3-5 to 10-20 times a day. At the same time, the frequency of urination increases, both at night and during the day. Some patients experience painful urination, accompanied by burning pain in the urethra and pubic area. In severe cases, microcystitis may cause urinary incontinence.
Hematuria (blood in the urine) is an important symptom of bladder tuberculosis. It accompanies the above-described symptoms of dysuria, but in rare cases it can be the first and only symptom of bladder tuberculosis. Hematuria is manifested by the fact that when urinating, an admixture of blood appears in the last drops of urine. If blood in the urine is observed throughout urination, this indicates severe tuberculous damage to the renal parenchyma.
Pain in the lumbar region and back appears when pyelonephritis develops. Pain may also appear when the patient develops hydronephrosis. A small proportion of people develop attacks of renal colic if a clot of blood or pus passes through the ureter.
Pyuria in kidney tuberculosis and bladder tuberculosis occurs in 20% of cases. A urine test reveals a large number of pus cells (white blood cells), which makes the urine cloudy.
Diagnosis of bladder tuberculosis
Diagnosis of bladder tuberculosis begins with the doctor collecting a detailed history of the disease and analyzing the symptoms of the disease. Symptoms of chronic cystitis, detection of pus cells in the urine and lack of bacterial growth on standard culture media, lack of effect from treatment of cystitis according to standard antibacterial regimens should prompt the doctor to think about the possibility that the patient has tuberculosis of the bladder.
Routine research methods include a general blood and urine test, a biochemical blood test, and a tuberculin test.
The standard in the diagnosis of tuberculosis of the genitourinary system is the cultural method for determining acid-fast bacteria. The material for diagnosis is urine, collected three times in the morning. Special culture media are used (solid nutrient media, for example, Lowenstein-Jensen medium, and bacterial growth is observed after 4 weeks). Currently, bacteriological analysis is carried out using the BACTEC 460 system (an automated system for cultivating mycobacteria in liquid nutrient media with subsequent radiometric detection of growth). In this case, the result is obtained within 2-3 days.
Polymerase chain reaction (PCR) has high sensitivity (more than 90%), specificity (more than 95%) and is fast to perform. The result can be obtained within 6 hours after taking the sample.
Luminescent and fluorescent microscopy is also used in diagnosis .
X-ray examination
An X-ray examination of the chest organs (CH) may reveal tuberculosis foci (active process or past tuberculosis). Since bladder tuberculosis is a secondary process in relation to kidney damage, radiographic examination methods reveal signs of tuberculosis in both the bladder and kidney. A survey X-ray of the retroperitoneal organs reveals calcifications of varying sizes in the kidney parenchyma and the bladder wall. In addition, enlarged mesenteric lymph nodes and calcifications in the adrenal glands can be visualized on a plain radiograph.
Intravenous pyelography and voiding cystography have high sensitivity (88-95%). These techniques allow us to determine the severity and extent of the pathological process. The earliest changes detected during these studies are: the presence of cavity structures (cavities) in the renal parenchyma, stenosis and stricture of the ureters. Late changes include cortical necrosis and cavities in the kidney, calcifications in the renal parenchyma and bladder wall, and ureteral and urethral strictures. The bladder is deformed and significantly reduced in size. These techniques also make it possible to visualize fistulas opening into the abdominal cavity and rectum, and with voiding cystography it is possible to detect vesicoureteral reflux (Fig. 2).
Fig.2. A – Intravenous urography. There is no visualization of the non-functioning right kidney in the figure. B – voiding cystography. The figure visualizes a reduced bladder size and registers vesicoureteral reflux.
Contrast-enhanced computed tomography (CT) can also visualize the above-described signs of bladder tuberculosis. In addition, even small calcifications and minor thickenings and changes in the structure of the bladder wall are clearly visible on CT.
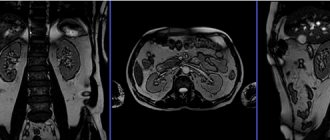
Magnetic resonance imaging (MRI) is a highly sensitive method for diagnosing the severity and extent of bladder tuberculosis and is particularly useful in visualizing the course of fistulas.
Cystoscopy allows the doctor to use a cystoscope inserted into the urethra to see the inside of the bladder. In addition, during this study, a biopsy of the bladder wall is performed, followed by bacteriological and histological analysis (Fig. 3.).
Fig.3. Histological examination of a biopsy specimen of the bladder wall.
Also, to diagnose bladder tuberculosis and assess the severity and extent of the pathological process, the following methods can be used: ultrasound of the retroperitoneal organs, angiography, vasography, scintigraphy, etc.
Treatment of bladder tuberculosis
Drug treatment of bladder tuberculosis is a long process lasting at least 4-6 months, requiring the prescription of at least 3 drugs. For drug therapy, special antibacterial drugs are used that are highly active against Mycobacterium tuberculosis. These include: rifampicin, isoniazad, pyrazinamide, ethambutol, ethionamide, prothionamide and other drugs. The treatment is very difficult to tolerate, as it often causes side effects. In case of severe impairment of renal function, the dosages of prescribed drugs are reduced to prevent the toxic effects of medications on the human body.
Surgical treatment of bladder tuberculosis
Surgical treatment is required for patients with gross disorders of the bladder structure (i.e., with a small bladder). The goals of augmentation cystoplasty (an operation aimed at increasing the size of the bladder):
- increasing bladder capacity to eliminate urinary incontinence;
- restoration of the functional activity of the bladder (i.e., the bladder should work as a low-pressure reservoir during the period of urine accumulation, and a high-pressure compressor during urination);
- elimination of vesicoureteral reflux (usually achieved by increasing the size of the bladder) to preserve kidney function.
Various types of reconstructive plastic surgery are used depending on the individual patient's indications. The following operations can be performed: sigmoidocystoplasty, ileocystoplasty, cecocystoplasty, ileocecocystoplasty, gastrocystoplasty, formation of an orthotopic bladder, etc. The essence of intestinal augmentation of the bladder is that to increase the volume of the bladder, a segment of the intestinal tube on a vascular pedicle is used, which is fixed to the wall Bladder.
Intestinal plastic surgery (augmentation) of the bladder gives excellent long-term results in patients with a bladder volume of less than 100 ml, leveling the symptoms of the disease. In addition, the pathological mechanisms of kidney damage are eliminated, allowing for the preservation of its function.
The article is for informational purposes only. For any health problems, do not self-diagnose and consult a doctor!
Author:
V.A. Shaderkina is a urologist, oncologist, scientific editor of Uroweb.ru. Chairman of the Association of Medical Journalists.
Laboratory research methods for tuberculosis
Date: 05/28/2018
Sputum examination
. Detection of MBT in sputum has important epidemiological and clinical significance.
It is better to collect sputum in the morning. The patient should first rinse his mouth so that there is less saliva in the sputum. If there is a small amount of sputum, it is collected within 24 hours.
In the absence of sputum, its appearance should be caused by irritating inhalations of an aerosol of a hypertonic solution of table salt with soda.
Bronchial lavage water obtained after administration of 10-12 ml of warm isotonic sodium chloride solution through the trachea is also examined.
The examination of sputum begins with its examination. In patients with pulmonary tuberculosis, the sputum may contain streaks or blood clots, pieces of calcified bronchial stones - broncholiths.
Microscopic examination of stained sputum smears in patients with destruction of lung tissue reveals elastic fibers. Sometimes there are so-called coral fibers, which are formed as a result of the deposition of fatty acids on elastic fibers, as well as lime-coated elastic fibers and amorphous calcareous particles.
To detect MBT in sputum, it is examined repeatedly, sending a morning portion to the laboratory for at least 3 days in a row. In some cases, MBT can be detected in sputum and in the absence of radiological changes in the lungs (in this case, ulcerative bronchial tuberculosis cannot be excluded). Sputum examination is necessary before starting anti-tuberculosis chemotherapy.
Detection of MBT in pathological material is carried out by bacterioscopic, bacteriological (cultural) and biological methods.
In addition to sputum, objects of study for the detection of MBT can also be urine, feces, cerebrospinal fluid, exudate from cavities, and biopsies of various tissues.
The main method for identifying MBT is bacterioscopic. In many developing countries, it is widely used not only for diagnosis, but also for identifying tuberculosis patients during mass population surveys.
For direct bacterioscopy, the preparation is stained using the Ziehl-Neelsen method: first with a carbolic solution of fuchsin, and then, after bleaching with a 5% solution of sulfuric acid or a 3% solution of hydrochloric acid, and then stained with a 0.25% solution of methylene blue. The stained preparations are examined microscopically in an immersion system. MBTs are colored red, and the surrounding background and non-acid-fast microorganisms are colored blue.
The information content of the bacterioscopic method for identifying MBT increases by 14-30% when using fluorescent microscopy. To color the drug, fluorochromes are used - organic dyes that fluoresce when illuminated with ultraviolet, violet or blue rays. Such dyes are auramine and rhodamine C. The drug is examined using a fluorescent microscope. MBTs glow golden yellow against a dark background.
To detect MBT in a preparation using the bacterioscopic method, it is necessary that 1 ml of sputum contains at least 100,000 microbial bodies. With a smaller number of mycobacteria, the test may give a false negative result.
To increase the amount of MBT per unit volume of sputum under study, flotation and sedimentation methods are used, especially with negative results of direct bacterioscopy.
The most widely used flotation method is based on the fact that after shaking an aqueous suspension with a hydrocarbon, MBT floats to the surface along with the resulting foam. Gasoline, benzene, and xylene are used as hydrocarbons. A creamy (flotation) ring of hydrocarbon particles with mycobacteria that forms on the surface serves as a material for the preparation of drugs. When using the flotation method, the number of positive bacterioscopy results increases by 10%.
The bacteriological (cultural) method for detecting MBT involves inoculating sputum on nutrient media. Before sowing, sputum is treated to suppress the growth of nonspecific microflora. The standard nutrient medium for growing MBT is Lowenstein-Jensen solid egg medium. There are also semi-liquid and liquid nutrient media. The growth of the MBT culture occurs in 14-90 days.
To isolate an MBT culture, 20-100 microbial cells in 1 ml of sputum are sufficient. Obtaining a pure culture of mycobacteria makes it possible to determine their viability, virulence, and sensitivity to drugs.
Often, mycobacteria determined by bacterioscopy do not grow on nutrient media due to the loss of the ability to reproduce under the influence of chemotherapy. According to the bacteriological study, a quantitative assessment of bacterial excretion is carried out: scanty - up to 50 colonies on the medium and abundant - more than 50 colonies.
The biological method consists of infecting animals (guinea pigs) with infected sputum that are highly sensitive to MBT.
Before infecting animals, sputum is treated with sulfuric acid to destroy nonspecific microflora and centrifuged. The sediment (in an isotonic sodium chloride solution) is injected subcutaneously into the groin area, intraperitoneally or into the testicle. In order to reduce the guinea pig's resistance to MBT, large doses of cortisone are administered to it daily. About a month after infection, the pig's lymph nodes become enlarged and generalized tuberculosis develops.
Among the methods for detecting MBT and diagnosing tuberculosis, the biological method was until recently considered the most sensitive, since tuberculosis in guinea pigs can be caused by the introduction of sputum containing less than 5 microbial bodies per 1 ml.
The possibility of loss of virulence by Mycobacterium tuberculosis has now been proven. Such mycobacteria are viable, can grow on nutrient media, but do not cause disease in experimental animals. Therefore, to identify MBT in pathological material, it is necessary to use various methods of microbiological research.
Blood test
. There are usually small changes in the blood of patients with tuberculosis. Hypochromic anemia is determined only in patients with a widespread process and severe intoxication or with repeated pulmonary hemorrhages. ESR increases during periods of exacerbation of the tuberculosis process.
Changes in the number of leukocytes and the leukocyte formula of the blood occur mainly during acute processes and the breakdown of lung tissue. Leukocytosis, an increase in the number of band neutrophils, lymphopenia, monocytosis, and eosinopenia may be observed.
To assess the patient’s condition, his nonspecific and specific reactivity, as well as to determine the activity of the tuberculosis process and select the optimal treatment tactics, the determination of some biochemical and immunological parameters is essential.
In patients with tuberculosis who produce large amounts of sputum, with abundant purulent pleural exudate, and renal amyloidosis, hypoproteinemia may occur, unlike patients with other forms of tuberculosis.
In acute tuberculosis inflammation, the albumin-globulin ratio decreases, the content of fibrinogen and sialic acids in the plasma increases, and C-reactive protein appears.
To monitor the functional state of the liver and kidneys in the blood, the content of alanine and aspartic aminotransferases, alkaline phosphatase, bilirubin, the level of residual nitrogen, urea, creatinine is determined, coagulation tests are performed with blood serum - thymol, sublimate. In order to exclude diabetes mellitus, which is often combined with tuberculosis, the glucose content in the blood is determined.
To confirm the tuberculosis etiology of the disease, an enzyme immunoassay method is used, based on the antigen-antibody reaction. If immunodeficiency is suspected, the content of immunoglobulins in the blood serum is determined. To diagnose immunodeficiency and monitor its course, the number of B and T lymphocytes is determined.
With active tuberculosis, all immunological reactions are positive, and their severity depends on the phase of the tuberculosis process. In patients with a favorable course of tuberculosis, the reaction of blast transformation of lymphocytes is most pronounced, and in patients with a progressive course, the reaction of inhibition of leukocyte migration in the presence of tuberculin PPD is most pronounced.
During an outbreak of the process, the number of T-rosette-forming lymphocytes decreases and the number of B-rosette-forming lymphocytes increases, while the content of G- and A-immunoglobulins decreases.
Immunological tests are used for the differential diagnosis of tuberculosis. For example, in cancer and sarcoidosis, in contrast to tuberculosis, there is a suppression of the activity of T-lymphocytes in the blast transformation reaction with phytohemagglutinin (PHA); most patients have negative reactions of blast transformation of lymphocytes and migration of leukocytes with PPD.
Urine examination
. In patients with pulmonary tuberculosis, urine analysis is usually
does not provide significant diagnostic information, but sometimes serious complications of the underlying disease are revealed. In case of kidney tuberculosis, protein, leukocytes, often erythrocytes, as well as MBT are found in the urine. When pulmonary tuberculosis is complicated by amyloidosis, persistent proteinuria and microhematuria are observed.
The excretion of 17-ketosteroids and 17-hydroxycorticosteroids in daily urine is used to assess the functional state of the adrenal cortex.
Prepared by:
Kulmaganbetova Zh.Sh - doctor bacteriologist of the Kyzylorda Regional Anti-TB Dispensary
Kidney tuberculosis - clinical symptoms, features of diagnosis and treatment of the disease
Although modern medicine has made significant progress compared to past times, diseases also do not stand still. Due to polluted ecology, climate change, active human activity, which often lacks proper rest, the immune system is significantly weakened, which creates one of the main favorable conditions for any disease. Many diseases have become stronger, more active, or even mutated. In addition, they spread quickly, which is why almost everyone who does not take good care of their health is at risk of becoming their victim. One of the rather serious diseases is kidney tuberculosis, which is the most popular type of tuberculosis after the pulmonary form.
Symptoms The difficulty in determining the presence of kidney tuberculosis in a person lies in the absence of specific, pronounced symptoms. At the initial stage, kidney tuberculosis has symptoms similar to those of other diseases, for example, malaise. Poor health can be characterized by general weakness in the body, low-grade fever (37 - 37.5 ° C), but almost half of the sick may not show any symptoms at all. Any unpleasant sensation occurs as the disease develops in the body and at a certain stage the pathological process manifests itself in the form of lower back pain. So, gradually, behind the lumbar pain, disturbances in the urinary system begin to occur, or more precisely, dysuria and gross hematuria may be observed. In addition, not many people experience lumbar pain at the beginning; a larger percentage is susceptible to it at a more progressive stage. The pain is dull and aching in nature, but it can suddenly develop into renal colic. Jumps in blood pressure and sudden weight loss are even less common with kidney tuberculosis.
Tuberculosis of the kidneys and urinary tract is characterized by a long incubation period, which can take an average of 2 to 3 years. During this period, again, the presence of the disease in the body may go unnoticed. Timely prevention will allow you to detect the disease as early as possible, which will allow you to begin an active course of treatment and reduce the likelihood of severe consequences.
Signs. The main symptom of the disease is a disturbance in the functioning of the kidneys, as well as discomfort. In addition, malfunctions in the urinary system, which are characterized by pain when going to the toilet, as well as the detection of blood in the urine help determine the presence of a problem. The neglect of the disease leads to the formation of multiple foci, as well as the capture of new surfaces by microbacteria, including the urinary tract.
Causes. Kidney tuberculosis is contagious. The disease is caused by a microbacterium, which is also known as Koch's bacillus. This is the same microbacterium that causes the pulmonary form of the disease. How is renal tuberculosis transmitted? There are several ways for infection to enter the kidney specifically. The main route is hematogenous, that is, through the blood. The bacterium reaches the kidney through the blood vessels and begins to create many small foci. If the person’s body has good immunity, then the lesions may not grow much, but over time they will shrink and disappear on their own. Another route of infection is airborne, when the bacterium is transmitted from an infected person to a healthy person through the common environment. However, this most often causes the pulmonary form of the disease. With the pulmonary form of tuberculosis and incomplete proper treatment, the microbacterium can move throughout the body through the blood and, thus, capture new territories.
There are a number of other causes of kidney tuberculosis, which do not provide a 100% guarantee of the occurrence of the disease, but in some cases they can cause the following problem: prolonged fasting; severe hypothermia; work injuries; constant exposure to air contaminated with chemicals; prolonged colds; serious skin diseases. In general, the listed factors can also be characterized as causes that cause a strong decrease in immunity, as well as active malfunctions in the body. They create favorable conditions for activities that have entered the body of the Koch bacillus.
Factors of increased development of the disease and low probability of complete recovery include: concomitant diseases in the same area; further weakening of the immune system. It is worth noting that with strong immunity, the percentage of infection is much lower. A strong body is able to cope with an infection on its own, which is why a person may not even know that he had a similar disease.
Forms. Experts classify forms of kidney tuberculosis according to several criteria. In the first case, the disease is characterized by stages, or rather
- Stage I infiltrative – the initial stage in which the structure of the kidney is not yet subject to changes;
- Stage II - initial destruction - inflammation and necrosis of the renal papillae are observed, and a so-called cavity or cavern is formed;
- Stage III limited destruction – multiple cavities appear;
- Stage IV: total destruction - transformation of the kidney into a whole system of caverns or the formation of one continuous cavity, the walls of which are the remaining renal tissue.
The second division occurs according to the clinical forms of the disease, of which two are distinguished: acute form (miliary) - a uniform eruption of so-called tubercles occurs, the active process of the disease; chronic form - occurs when a microbacterium is already present in the body, which functioned on another organ, but jumped out of the primary focus, ending up in the kidney.
The form or stage of the disease can only be determined with a full examination and special tests. By clarifying the form, it is easier to choose the most effective treatment course.
Diagnostics. To make a diagnosis, especially given the certain secrecy of the disease in the initial stages, laboratory and hardware-instrumental research is used. To begin with, when a suspicion of such a disease arises, it is necessary to conduct a tuberculin test. Laboratory research methods include: complete urine analysis; bacterial culture; ELISA; PCR diagnostics; There are also a number of more complex procedures for diagnosing renal tuberculosis: ultrasound; CT scan; Magnetic resonance imaging; X-ray; morphological studies; radionuclide research. Most often, there is no need to undergo absolutely all tests, because the results of a maximum of 2-3 can confirm kidney tuberculosis. Diagnosis at the initial latent stage of the disease may require more than 3 types of research.
Treatment. When kidney tuberculosis is diagnosed, the patient is placed in an anti-tuberculosis dispensary where treatment is carried out. Depending on the condition of the body, its resistance to the disease and the effectiveness of treatment, the length of stay in the dispensary may vary.
Treatment involves the following:
- taking anti-tuberculosis drugs (isoniazid, rifampicin, streptomycin, prothionamide, kanamycin and others);
- nephrostomia (installation of a catheter or drainage to drain urine from the kidney);
- surgical intervention;
- strengthening the body and the recovery process.
Complications. The main complication of the disease is the destruction of the organ through the formation of multiple cavities filled with dead cells. A similar case is called tuberculous pyonephrosis. In this case, only thin tissue walls of the resulting cavities remain from the healthy areas of the kidney. In addition, the consequence may be atrophy, which consists in the death of tissues and their transformation into tissue that does not perform any functions necessary for the body, but is simply connective between the remaining parts of the organ. In some cases, a disease such as amyloidosis may develop. It causes the deposition of insoluble protein (amyloid) in the kidney tissue. It functions in this way, and under its influence the functions of the organ are impaired. The most serious consequence that can occur after kidney tuberculosis is chronic renal failure. It consists in the final disruption of renal functions, as well as in the death of its cells.
Prevention. The main measures for the prevention of kidney tuberculosis in children and adults are timely vaccination, correct diagnosis and treatment of the pulmonary form, as well as the elimination of possible relapses by following the recommendations of a specialist. At least once a year, conduct a complete examination of the body and take tests to identify microbacteria, since symptoms may not appear in the early stages. You just need to monitor your health, detect and treat other diseases in time, strengthen your immunity and lead a healthy lifestyle. You should not constantly overexert yourself, but give your body proper rest.
Phthisiatrician
anti-tuberculosis department
clinic No. 1
Bolotnik Tatyana Vasilievna