Renal nephroscintigraphy is an effective type of kidney examination through the introduction of a special radioactive label into the body of an adult patient or child. This drug, in combination with a gamma camera, provides a broadcast of a complete image of the condition of the kidneys. The method is considered absolutely harmless, since the process involves a minimal radioactive load on the body, and the drug used is quickly removed from the body without additional support.
Renal nephroscintigraphy has a significant advantage over x-rays, ultrasound or tomography, since it studies not only the detailed structure of the kidneys, but also thoroughly demonstrates their individual characteristics and degree of activity. The altered tissue cells respond unnaturally to this irradiation, and therefore the camera easily records them if they are present in the organ.
Types of nephroscintigraphy
The study is highly effective in detecting kidney diseases at their initial development, during a period when tissues have not yet had time to significantly change their structure and appearance, but functionally have already begun to demonstrate negative changes in their functioning.
For the most effective examination in different cases, as well as for different tasks, they resort to one of two main research schemes.
- Statistical nephroscintigraphy of the kidneys. Recommended for obtaining accurate data regarding the physiological characteristics of the kidneys. Depending on the required tasks and complexity, the process can take from 30 minutes to 2.5-3 hours. First, a special radioactive agent penetrates into the patient’s body, and only after 30-60 minutes the main manipulations begin.
- Dynamic nephroscintigraphy of the kidneys. It involves not a sudden, but a gradual introduction of the diagnosed medical product into the body and an examination some time after this manipulation. Using this method, the doctor receives the most detailed information about the nuances of the passage of the radionuclide through the body along with urine. This guarantees a detailed study of the functioning and condition of the patient’s kidney blood vessels, the degree of their saturation with blood and the organ’s performance.
The final decision about which method to use in a particular case is made by the attending physician based on the characteristics of the patient's condition.
How to prepare for an MRI of the kidneys?
Before examining the urinary system, it is advisable to follow a special diet. This is due to the structural features of the human body: during MRI of the kidneys, intestinal loops fall into the scanning area. Increased gas formation can negatively affect the results of the diagnostic procedure.
Scanning of the urinary system in frontal, axial and sagittal projections
Preparation for the study involves removing foods and drinks that cause flatulence from the diet 2-3 days before the MRI of the kidneys:
- beans, peas and other legumes;
- cabbage;
- milk;
- black bread;
- yeast dough;
- confectionery;
- fresh vegetables and fruits;
- kvass;
- carbonated drinks.
It is advisable to avoid fatty and spicy foods, limit the amount of sweet, salty, smoked foods. 2-3 days before the test you must abstain from alcohol.
In case of kidney diseases, the attending physician may give additional recommendations related to the characteristics of the pathology before the MRI. The filtration organs are involved in the removal of harmful and toxic substances, so the condition of the urinary system largely depends on the patient’s diet. Eating unfamiliar foods or drinks may trigger an unwanted reaction.
Some clinics in St. Petersburg conduct preliminary consultations with a radiologist. The specialist will tell you how to prepare for an MRI of the kidneys and warn about possible complications.
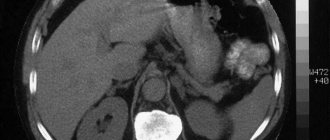
Kidney cancer on MRI
Patients should inform their doctor about any contraindications to tomography. If necessary, the procedure will be replaced by an alternative instrumental study (CT, ultrasound).
In case of increased nervousness or severe pain, premedication may be required before MRI of the kidneys. Analgesics, antispasmodics and sedatives are prescribed by a specialist; self-administration of medications is prohibited.
Preparation for an MRI of the kidneys with contrast includes additional tests to assess the functionality of the filtration organs. Serious complications of enhanced scanning include:
- systemic nephrogenic fibrosis;
- acute kidney damage;
- retention of gadolinium chelates in the body.
These pathologies develop when contrast is used in patients with end-stage renal and liver failure. A glomerular filtration rate test will help prevent side effects. Low values (less than 15 ml/min.) are a contraindication to injection of gadolinium solution.
MRI of the kidneys in men, as in women, is performed on an empty stomach. The exception is the contrast procedure: it is advisable to have a snack an hour before the session. When scanning the bladder, the patient drinks 0.5-1 liter of water half an hour before the session. Examination of a filled organ is more informative.
MRI of the kidneys with contrast is not done during pregnancy. A woman should notify her doctor about a possible contraindication. The lactation period is not a limitation to the use of the “coloring” drug. Nursing mothers express milk for their baby in advance. You can put your baby to your breast 6-12 hours after the session.
Before scanning, the patient removes metal jewelry, accessories, and changes into a comfortable set (pajamas).
Indications for examination
The urologist refers the patient to detailed nephroscintigraphy of the kidneys if he has the following indications:
- suspicion of the presence of tumor formations or metastases in the area of the kidneys and other urinary organs;
- the need for an additional and more accurate determination of the characteristics and nature of education (often for this purpose the method is used in conjunction with other studies);
- detection of deformations, changes in volume, location or structure of the kidneys;
- preparatory manipulations for planned surgery on this organ;
- the need to monitor the condition of the kidneys after a course of radiation or chemotherapy;
- assessment of the degree of functionality and capabilities of the kidneys and other organs of the urinary system.
INDICATIONS FOR THE STUDY
Nephroscintigraphy with EC (ethylene cysteine):
- detection of congenital anomalies and location of the kidneys
- hypertonic disease
- infectious and inflammatory diseases of the kidneys and urinary tract
- kidney injuries
- urolithiasis disease
- preoperative assessment of renal tubular function
- systemic diseases that occur with impaired renal function: diabetes mellitus, gout, vasculitis, etc.
- autoimmune kidney diseases (glomerulonephritis)
- toxic kidney damage
Angionephroscintigraphy with DTPA (diethylenetriamine pentaacetic acid):
- determination of total and separate functional mass of the kidneys
- detection of congenital anomalies and location of the kidneys
- hypertension (diagnosis of renal artery stenosis)
- infectious and inflammatory diseases of the kidneys and urinary tract
- kidney injuries
- urolithiasis disease
- preoperative assessment of glomerular kidney function
- systemic diseases that occur with impaired renal function: diabetes mellitus, gout, vasculitis, etc.
- autoimmune kidney diseases (glomerulonephritis)
- toxic kidney damage
Contraindications for diagnosis
Kidney nephroscintigraphy is not always prescribed for a child or an adult. Despite its safety and reliability, it has several contraindications.
Patients are not referred for diagnostics in the following situations:
- high severity of the patient’s condition: due to health reasons, not all people can lie freely without moving on the diagnostic table for about half an hour;
- a course of chemotherapy or radiation has just completed, the body needs rehabilitation for some time;
- a surgical operation undergone in the recent past: nephroscintigraphy of the kidneys can affect the accumulation of fluid in the just operated area of the body, which will adversely affect the rehabilitation period.
Dynamic or statistical nephroscintigraphy of the kidneys is also undesirable during pregnancy (however, it can be prescribed as an exception in particularly serious situations) and if the patient is found to have an individual intolerance to the drug injected into the body.
Laboratory of Radioisotope Diagnostics
Radionuclide diagnostics is one of the modern methods of radiation diagnostics for assessing the functional state of various organs and systems of the body using diagnostic radiopharmaceuticals labeled with radionuclides.
Currently, among the methods of radionuclide diagnostics, scintigraphy is the most widely used - a functional imaging method that involves introducing radioactive isotopes into the body and obtaining an image by determining the radiation emitted by them.
Features of radionuclide diagnostics (scintigraphy)
Imaging methods of radionuclide diagnostics are based on obtaining an image reflecting the distribution of radiopharmaceuticals introduced into the patient’s body, which specifically accumulate in various organs and tissues. Radiopharmaceuticals are specific chemical or biochemical compounds labeled with gamma-emitting radionuclides that have a short half-life. Gamma radiation emanating from the patient's body is recorded by a gamma camera detector and, after computer processing, the received information is converted into a functional image of the organ under study. The spatiotemporal pattern of distribution of the radiopharmaceutical gives an idea of the shape, size and position of the organ, as well as the presence of pathological foci in it.
Radionuclide diagnostic methods belong to molecular imaging methods, since they reflect pathological processes occurring at the molecular and cellular level and do not duplicate information obtained by other methods of radiation diagnostics (ultrasound, CT, MRI). Functional changes, which are much faster than anatomical ones, make nuclear medicine methods unique both in the early diagnosis of diseases and in dynamic monitoring. Radionuclide diagnostics are widely used in oncology, endocrinology, cardiology, uronephrology, and neurology.
Laboratory of Radioisotope Diagnostics of the RKB named after. G.G. Kuvatova is located on the third floor of the Diagnostic Center and is equipped with a Millennium emission computed tomograph, 2 gammas of the VNR laboratory, and a radiometer.
The laboratory uses the following radiopharmaceuticals: a solution of sodium iodine-hippurate, labeled with iodine-131, which has a half-life of 8.3 days, and technetium-99m with kits for it, the half-life of which is 6 hours.
All research methods are based on the principle of accumulation of tropic radiopharmaceuticals in the organ under study, which includes Ts-99m.
Contraindications:
- absolute - pregnancy;
- relative - breastfeeding (do not breastfeed for 24 hours).
The following studies are carried out at RDL:
Radionuclide methods for studying the kidneys include: renography, dynamic and static renal scintigraphy.
The main indications for radionuclide examination of the urinary system are:
- assessment of individual renal function;
- visualization of a “non-functioning” kidney during intravenous urography;
- demonstration and function of ectopic renal tissue;
- detection of congenital anomalies;
- assessment of renal artery patency;
- diagnosis of renovascular hypertension;
- preoperative assessment of renal function;
- detection of vesicoureteral reflux;
- as an alternative method to intravenous urography in patients sensitive to iodine;
- preparation for kidney transplantation.
Radionuclide renography : the method is based on graphical registration of the process of changes in activity in the kidneys after the introduction of nephrotropic radiopharmaceuticals by counting radiation with two detectors directed at them. The resulting renograms reflect the ability of the kidneys to clear the blood of the administered drug, as well as the time characteristics of its transport through the kidneys and collecting system.
Dynamic nephroscintigraphy is a method based on dynamic recording of radioactivity in the kidneys and blood after intravenous administration of a nephrotropic radiopharmaceutical excreted by the kidneys, and computer processing of the resulting images.
The second stage is radionuclide renography, which is a valuable method for diagnosing and determining the doctor’s treatment tactics for early functional and organic changes in the kidneys and upper urinary tract, not only on the affected side, but also in the contralateral kidney.
Scintigraphy of the thyroid gland. The examination is carried out to determine the anatomical and topographical state of the organ: location area, aberrant tissue, establishing the structure and shape of the gland, identifying structural disorders, the presence of “cold”, “warm” and “hot” foci.
Indications:
- if nodular forms of goiter are suspected;
- if an aberrant thyroid gland is suspected;
- in the differential diagnosis of tumor formations in the neck area;
- for the purpose of postoperative control.
Scintigraphy of the parathyroid glands is used to diagnose tumors of the parathyroid glands, as well as to detect ectopic tissue of the parathyroid glands. The sensitivity of the method in diagnosing this pathology is 93%, which is 1.% times higher than the capabilities of CT or NMR tomography.
Indications:
- suspicion of parathyroid adenoma;
- osteoporosis of unknown etiology;
- recurrent kidney stone formation;
- primary hyperparathyroidism;
- planning and monitoring of surgical treatment of hyperparathyroidism;
- differential diagnosis of space-occupying mediastinal formations.
Scintigraphy of the liver and spleen is based on obtaining an image of the liver and spleen by recording, using a gamma camera, radiation emanating from radiopharmaceuticals selectively accumulating in these organs.
Indications:
- assessment of “anatomical” features (determining the location, size, shape of the liver and spleen) in normal and pathological conditions;
- diffuse changes in the liver (hepatitis of various etiologies, cirrhosis of the liver);
- Liver cintigraphy with Tc-99-labeled erythrocytes is an extremely accurate method for diagnosing cavernous hemangiomas of the liver.
Skeletal scintigraphy is an extremely sensitive method for detecting skeletal bone pathology. The sensitivity of the method is based on its ability to detect functional changes.
Indications for skeletal scintigraphy are:
- search for bone metastases in tumors of various locations;
- assessment of the extent of the primary bone tumor and search for its metastases;
- clarification of the degree of regression of the tumor process after radiation, hormonal and drug therapy;
- suspicion of osteomyelitis, arthritis;
- detection of radiographically poorly detectable fractures
- assessment of bone tissue recovery after fractures;
- suspicion of aseptic necrosis of the femoral head;
- assessment of the condition of joint prostheses;
- disturbance of mineral metabolism;
- diseases of the parathyroid glands.
Osteoscintigraphy makes it possible to use it as a screening method in cancer patients.
Advantages of skeletal bone scintigraphy compared to other imaging methods:
- high sensitivity (metastases are detected 3-12 months earlier than radiography)
- visualization of the entire skeleton;
- does not require preparation;
- does not present significant difficulties in conducting the research itself;
- the study is minimally invasive (IV injection of radiopharmaceuticals) and painless;
- the method is quite safe, the radiation exposure is 2 times less than with x-ray studies of comparable volume;
- no prior preparation required.
The dose of the intravenously administered drug is small and allows diagnosis without significant harm to health.
Lung perfusion scintigraphy is the main screening procedure for pulmonary thromboembolism (PE). The absence of accumulation of radiopharmaceuticals in any area of the lungs indicates a violation of blood flow in this region. A negative radionuclide test result completely excludes the diagnosis of pulmonary embolism.
Perfusion scintigraphy of the left ventricular myocardium currently occupies a priority position in the diagnosis of coronary ischemia compared to other methods of cardiac examination, which is primarily due to its high sensitivity, specificity and information content. The non-invasive method of administration of most labeled compounds is also of great importance. Drugs in this group provide a unique opportunity for quantitative and qualitative assessment of myocardial tissue perfusion.
General goals of myocardial perfusion scintigraphy:
- determining the presence, location, extent and severity of myocardial ischemia or scar damage;
- determination of the functional significance of the lesion of the main coronary bed identified by angiography;
- differential diagnosis of reversible and irreversible myocardial damage, i.e. assessment of its viability;
- differential diagnosis of angina and cardialgia;
- monitoring and evaluation of treatment effectiveness.
The Radioisotope Diagnostics Laboratory is open from 8:30 a.m. to 4:00 p.m. Make an appointment for an examination by calling 279-03-85 or at the diagnostic center on the 3rd floor in room 324.
Head of the Laboratory of Radioisotope Diagnostics Rozalia Anvarovna Akchurina, doctor - radiologist of the highest category.
Preparation for the diagnostic procedure
Renal nephroscintigraphy does not require special preparation and requires a special diet.
In some cases (based on the characteristics of the examination), the patient must first drink additional clean water or, on the contrary, completely empty the bladder. The attending physician or specialist performing statistical or dynamic nephroscintigraphy of the kidneys will warn about all these actions, if necessary.
Before lying on the doctor's couch, you must remove any metal objects, as well as jewelry and clothing with metal inserts.
The essence of diagnosis, goals and advantages
The kidneys act as the main cleansing system of the body. With their help, blood is filtered, which is cleansed of various toxins and other harmful substances. Conventional research methods, such as blood and urine tests, can reveal various disorders in the functioning of the organ and determine the cause of these disorders.
Well, radioisotope renography makes it possible to see exactly how the filtration process occurs, display the work of the glomeruli at the current moment in time, and also monitor the work of the organs individually.
The main purpose of renography is precisely to display the work of internal organs, analyze and monitor their condition. Based on the data from this study, an accurate diagnosis cannot be made, but it is definitely possible to see various disturbances in the functioning of internal organs, as well as monitor the effectiveness of therapy.
The main advantage of kidney renography is the simplicity of the procedure, which requires virtually no additional preparation and the absence of high doses of radiation. Renography is prescribed to all patients who have obvious kidney problems.