What is eye fungus
Fungal diseases of the eyes are caused by fungi of the genus Candida, which, when they come into contact with the mucous membranes of the organ of vision and weaken the protective functions of the body, begin to actively parasitize them, which leads to the development of the disease.
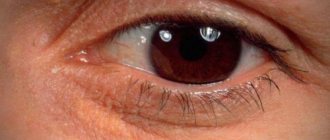
Fungus on the eyelids, photo
The first symptoms of the disease begin to appear a few days after the infection enters. Initially, redness of the eyelids and eyeball appears. There is itching and a feeling of the presence of a foreign object in the infected organ.
Penetration of fungi into the eyes is possible both from the outside through contact with carriers of pathogen spores, in the case of damage and trauma to the organs of vision, and from internal affected organs through the bloodstream. The disease is more common in children due to incompletely formed body defenses.
At the initial stage, the disease is often confused with conjunctivitis and incorrect treatment is carried out, which contributes to the occurrence of complications.
Methods for treating fungus on eyelashes
Need advice from a beauty expert?
Get advice from a beauty expert online. Ask your question right now.
ask a free question
If signs of the disease appear, you should visit an ophthalmologist. Self-treatment is not recommended, and it is undesirable to use traditional methods without a doctor’s prescription. Incorrect therapy will aggravate the situation, worsen the condition and cause complications.
At the appointment, the doctor will definitely examine the area affected by the fungus and collect tests to identify the type of mycosis pathogen. The specialist will review the medical history to identify possible chronic diseases and existing ophthalmological ailments. He will find out whether the patient is taking medications. Correctly prescribed treatment will depend on the information.
If the skin of the eyelids is damaged, the patient needs to consult a dermatologist or mycologist. To determine the diagnosis, a scraping of the affected skin will be required. After the tests, therapy is prescribed, including taking pills, applying ointments and creams, and drops. In advanced cases, injections are prescribed. Treatment is carried out on an outpatient basis, only severe cases require medical supervision and inpatient treatment.
Ointments, creams
An ointment for treating manifestations of fungus on the eyelids consists of components that provide an antifungal effect. Usually prescribed ointments and creams:
- Clotrimazole;
- Fluconozole;
- Terbizil;
- Fundizol.
The products are gentle, you can treat the skin around the eyes several times a day.
Using a cotton swab, apply to the eyelid from the inside. It is better to use the medicine at night.
Drugs
To enhance the therapeutic effect, drugs are prescribed:
- Okomistin drops are effective in combating infectious eye diseases and various types of fungal infections. Drops are used up to five times a day, the course duration is about 7-10 days. Dezmistin drops have a similar effect;
- Miramistin is available in the form of ointment, cream, spray. To combat eyelash fungus, it is more effective to use a solution. The eyes are washed with liquid 4 times a day. The solution is instilled into the eye using a pipette, 1 drop per day. The duration of treatment is determined by the doctor. The product quickly eliminates unpleasant symptoms;
- Tablets with an antifungal effect are prescribed orally for a comprehensive fight against the pathogen. Doctors prescribe Fluconazole, Imidazole, Lamisil, Diflucan, Terbizil.
Injections
Types of eye mycosis
Fungal infections of the eyes vary depending on the type of localization of the fungus on the eyeball or on the eyelids. In nature, there are several varieties of fungal infection pathogens that affect the visual area.
Actinomycosis
Actinomycosis is caused by a separate type of fungus with a radiant mycelial structure. Due to the non-standard structure of the cells of the pathogen and its intermediate position between fungal and bacterial microflora, therapeutic therapy for this type of disease is difficult.
This type of fungus is very common in the environment, but cases of infection are not common. Spores of this type of fungus live on parts of plants. The incubation period for the development of the disease is several years.
Symptoms of actinomycosis are characterized by the formation of purulent granulomas on the affected parts of the body. When such growths are opened, the purulent contents fall on nearby areas and cause infection. The occurrence of severe inflammatory processes on the mucous membranes, the formation of abscesses and fistulas on the eyelids are typical.
When treating actinomycosis, injections of antibiotic drugs are used for a course of up to 3 months. Surgical intervention to open granulomas and then remove the contents to prevent the spread of infection is also possible.
Fungal conjunctivitis
Fungal conjunctivitis is an ocular form of fungal infection, resulting in acute or chronic inflammation of the conjunctiva. Often fungal conjunctivitis occurs together with blepharitis and keratitis.
The penetration and development of infection is facilitated by damage to the mucous membrane, the presence of chronic diseases and long-term use of antibiotic drugs that reduce the protective properties of the immune system. Favorable factors for the spread of the pathogen are a warm and humid climate and unsatisfactory sanitary conditions.
Symptoms of fungal conjunctivitis include redness of the eyeball with increased lacrimation and itching in the affected area. As the disease develops, photophobia and swelling appear, nodules with purulent contents and easily removable yellowish films appear.
To treat purulent conjunctivitis, antifungal drugs are used, both for local and systemic use for a course of up to 6 weeks.
Dacryocystitis
Dacryocystitis is an inflammatory disease of the lacrimal sac. The main cause of the disease is considered to be obstruction of the tear ducts, which results in stagnation of tear fluid, leading to the disappearance of its protective properties and, as a result, the development of fungi. The contents of the lacrimal sac gradually turn into pus.
The disease most often occurs in middle-aged women, which is associated with the anatomical structure of the female body. Factors contributing to the development of infection are chronic diseases, reduced immunity and sudden changes in temperature.
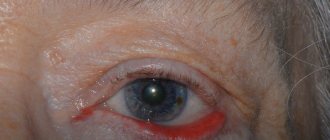
Symptoms of the acute form of dacryocystitis are expressed in severe redness of the skin and swelling in the area of the lacrimal sac, swelling of the eyelids and narrowing of the palpebral fissure. In the chronic form, the symptoms are not pronounced and are characterized by constant lacrimation.
To treat dacryocystitis, complex therapy is used using local antifungal drugs, antibiotics and physiotherapeutic procedures. In the chronic form, surgical intervention is recommended to open the tear ducts and prevent fluid stagnation.
Endophthalmitis
Endophthalmitis is an inflammatory disease of the visual organs with the accumulation of pus in the space between the iris and cornea. The inflammatory process is characterized by rapid progression, leading to the development of complications and, in the absence of treatment, loss of the eyeball.
The causes of the development of endophthalmitis can be traumatic injuries to the eyes with the entry of foreign objects and the penetration of a fungal infection against the background of a weakened immune system. The disease can also be triggered by other inflammatory processes in the body.
Symptoms are characterized by swelling of the eyelids, redness of the eyeball, discharge of pus, and pain in the infected area. Subsequently, clouding of the vitreous body and deterioration of visual acuity are characteristic.
For treatment, it is recommended to use increased doses of antibiotics by injection, including intraocular administration of drugs. If there is no effectiveness, the affected part of the vitreous is removed.
Keratitis
Keratitis is an inflammation of the cornea with clouding, which leads to decreased visual acuity. Inflammation can be caused by various microorganisms, including some types of fungus.
The causes of keratitis can be mechanical damage to the cornea, improper use of contact lenses, dry mucous membrane of the eye and weakened immunity. Development is also possible in the presence of other purulent inflammatory processes.
All forms of the disease include pain, photophobia, excessive lacrimation and foreign body sensation. In advanced forms, inflammation of all eye membranes may develop, which can lead to loss of vision.
Treatment of keratitis should take place in a hospital under the supervision of specialists for 4 weeks. To eliminate the infection, complex therapy is used.
Candidal blepharitis
Candidal blepharitis is an inflammation of the eyelids with dislocation on the ciliary edge. The disease often occurs in a chronic form with recurrent exacerbations. Fungus on the eyelid is caused by pathogenic microorganisms of the genus Candida. The infection primarily affects the hair follicles of the eyelashes.
The cause of the development of candidal blepharitis can be considered the active development of pathogenic microflora in the body due to weakened immunity. There is a risk of infection in people with oily or dry eyelid skin. Mature and older people are most susceptible to the disease.
Symptoms include swelling and redness of the eyelids with characteristic itching. There is rapid fatigue and increased sensitivity of the eyes with increased tear production. Subsequently, plaque forms on the eyelids and yellowish scales at the base of the eyelashes.
Treatment of candidal blepharitis is long-term and requires an integrated approach. The first goal in treatment should be the complete elimination of the infectious agent.
Scleritis
Scleritis is a slowly progressive, inflammatory disease that affects the entire thickness of the outer membrane of the eyeball. The disease is caused by damage to the eye by pathogenic fungi. In advanced cases, scleral tissue may die. The fungal form of scleritis is extremely rare.
The development of scleritis can be triggered by inflammatory processes in the body, injuries to the organs of vision and reduced immunity. The disease mainly affects people of mature age.
Manifestations of scleritis are expressed by pain, aggravated by pressure, increased lacrimation and redness of the eyeball and eyelids. Necrotic processes are characterized by the appearance of yellow spots on the shell.
To treat the disease, the use of topical medications and physical therapy is recommended.
Chorioretinitis
Chorioretinitis is an inflammation of the retina and posterior choroid. Characterized by a long incubation period. There are several types of infectious agents, including pathogenic fungi.
The causes of the disease may be infection arising from other organs, mechanical damage to the eye, complicated myopia and reduced immunity. The disease mainly affects middle-aged and older people.
The manifestation of symptoms of the disease manifests itself mainly in decreased vision, including night vision, and changes in visual functions in the form of distortion of objects and the appearance of spots during vision. There are no external changes in the organs of vision.
Anti-inflammatory and antifungal therapy is recommended for treatment. For advanced and chronic forms, physiotherapeutic treatment methods can be prescribed.
Symptoms
The type of pathogen and the localization of the pathological process determine the form and nature of the course of oculomycosis. Isolated or combined damage to several eye structures is possible.
Fungal inflammation of the conjunctiva is characterized by rather sparse clinical symptoms, minor discharge from the eyes, and a long course. Antibiotic therapy is usually ineffective. It should be noted that a protracted course of the disease can provoke deformation of the edges of the eyelids. Some features of the clinical picture of fungal conjunctivitis:
- In most cases, the conjunctiva appears swollen and hyperemic (reddened).
- Granulomatous nodules of an inflammatory nature appear on the mucous membrane of the eyelids.
- After rupture of the nodules, pus leaks out and ulcers form.
- The conjunctiva is covered with a light green coating.
- In the morning, the eyes stick together due to a dried film on the eyelids, which is formed as a result of purulent discharge.
Features of the course of fungal keratitis (inflammation of the cornea):
- The patient is bothered by painful sensitivity to light and lacrimation. There is a feeling that there is a foreign body in the eye.
- A ring-shaped infiltrate, gray-yellow in color and with unclear contours, is found in the cornea.
- If antifungal therapy is not carried out, the condition worsens significantly. There is an increase in infiltrate and the appearance of hypopyon (pus in the anterior chamber of the eyeball).
- There is an increase in swelling of the conjunctiva and deterioration of vision. Increased discharge from the eyes.
- Necrosis of the cornea (death) is possible with the development of an abscess and the spread of the pathological process to other anatomical structures.
Clinical picture of fungal scleritis (inflammation of the outer membrane of the eye):
- Redness and soreness of the inflamed sclera are almost always observed.
- If the infection does not spread to the cornea or internal structures of the eye, vision loss is usually not observed.
- Fungal keratoscleritis often develops when the sclera and cornea become inflamed.
- Nodular elevations or scleral abscess (purulent inflammation) are detected.
Diagnostics
When the first signs of mycosis of the organs of vision appear, you must immediately contact a specialist and undergo a comprehensive examination to clarify the diagnosis. Before prescribing tests, the specialist conducts an external examination of the patient to identify external symptoms of the disease. Anamnesis is also collected to take into account possible precipitating factors for the development of the disease. When examining a patient for a fungal eye infection, a specialist will check visual acuity and examine the eye itself using a slit lamp. If dacryocystitis is suspected, the lacrimal canals are examined for patency.
To clarify the diagnosis, an analysis of samples of biomaterial obtained by scraping the epidermis from the affected area is prescribed. Eye secretions are also examined. During the study, microscopy of the obtained biomaterial is carried out to determine the causative agent of infection, and cultural inoculation on a nutrient medium is carried out to determine the resistance of the pathogen to various drugs.
You should consult an ophthalmologist, and in case of large affected areas on the skin, a dermatologist can provide assistance.
You should not engage in self-medication and self-diagnosis, due to the fact that without the necessary qualifications, an error in prescribing therapy may occur, leading to serious complications.
Treatment of fungal blepharitis
Once diagnosed, fungal blepharitis requires immediate treatment. The choice of therapeutic regimen depends on the causative agent of the disease. Depending on the type of blepharitis, your doctor may prescribe the following treatment options:
- antifungal drugs;
- treating the skin of the eyelids with antiseptic agents;
- antibacterial drugs (indicated, for example, for actinomycosis);
- immunomodulatory therapy.
In some cases, surgery may be required to open abscesses. In each specific case, the treatment regimen and selection of medications are determined by the doctor. You should not self-medicate and rely on traditional medicine, as this can lead to the development of complications - spread of the disease to other tissues, deformation of the eyelids, and decreased vision.
How to treat eye fungus
The basis of therapy is the use of topical antifungal drugs, and in the case of severe or chronic infection, antibiotic drugs are prescribed.
Pharmacy drugs
| Type of drug | Name | Mode of application |
| Drops for fungus in the eyes | Okomistin, Dezmistin | Place 2 drops in each eye 6 times a day |
| Antifungal ointments | Nystatin, Levorin, Clotrimazole | Lubricate the area around the eyes and place on the lower part of the eyelids at night. |
| Fungal infection tablets | Fluconazole, Lamisil, Diflucan | Prescribed to eliminate fungal infections in the body |
Folk remedies
In the initial stages of the disease, traditional medicine can be used in addition to the main therapy.
Rinse with herbal infusion. To prepare the infusion, take a dry mixture of chamomile, calendula, St. John's wort, yarrow, oak bark and linden blossom. A strong herbal infusion is made. Eyes should be washed with this infusion up to 10 times a day.
For lotions, you can use strong brewed black tea. It is advisable to change the tea leaves every few hours. Lotions should be applied to the affected area every hour.
Diet
For fungal diseases of the eyes, the same diet is used as for fungal diseases of other organs. The basic principles of the diet are to eat foods that do not contain yeast and large amounts of carbohydrates. It is recommended to cook boiled, stewed and baked food. It is useful to use a large amount of vegetables and unsweetened fruits, lean fish and meats and fermented milk products in the diet.
Folk remedies to speed up treatment
At the initial stage of development of eye fungus, you can try to stop its spread using traditional methods. The following unconventional means can cope with this task:
- Spilled tea. Freshly brewed tea is not suitable for treatment, since it does not have time to form substances useful for this procedure. The drunken drink is used for compresses and lotions. They can be done several times a day. A folk remedy will not help to completely cure a fungus. But with its help it will be possible to reduce the severity of the symptoms of the disease,
- A decoction of calamus and yarrow. To use this product, you need to mix the plant material in equal quantities. After 2 tbsp. l. The resulting mass needs to be poured with 500 ml of boiling water. After cooling, the resulting decoction can be used to wash the eyes,
- Fresh cucumbers. Another proven and safe method of treating eye fungus. To prepare this remedy, you need to peel and chop a fresh vegetable. Afterwards, pour 500 ml of boiling water. It is recommended to add 0.5 tsp to the same mixture. soda The infusion should stand for 1 hour. Afterwards, you need to moisten a clean swab and apply it to the sore eye for 15 minutes.
Folk remedies must be combined with drug treatment. They are used until the patient achieves recovery.
Preventive measures
The basis of preventive measures for fungal infections of the organs of vision is to maintain the body’s immunity at a sufficient level; for this it is necessary to adhere to a healthy lifestyle and proper diet. It is necessary to ensure personal hygiene and do not touch your eyes with dirty hands. When wearing contact lenses, follow all instructions for use.
If preventive measures are correctly followed and a timely medical examination is carried out by a specialist when the first signs of the disease appear, eye mycosis will not pose a serious danger to the patient’s health.
Causes of diseases
With normal functioning of the immune system, a person is completely protected from oculomycosis, but in addition to weakened immunity, other reasons can lead to the development of a fungal disease. Among them:
- failure to comply with personal hygiene rules;
- recent infectious diseases;
- long-term use of antibiotics;
- hormonal disorders;
- improper wearing of contact lenses;
- surgical interventions or injections into the eye;
- various injuries to the organ of vision;
- HIV and AIDS;
- inflammation of the maxillary sinuses;
- frequent visits to rooms with high humidity;
- work in dusty production areas.
Important!
A common cause of infection is the penetration of a fungal pathogen into the blood with its subsequent passage to other parts of the human body. This method of infection is considered if the patient has already been diagnosed with one of the forms of mycosis.
Etiology of the disease
Eczema is often provoked by the following external and internal factors:
- diseases of the gastrointestinal tract;
- infection with worms;
- metabolic disorders and pathologies;
- hyper- and vitamin deficiency, etc.
In the initial stage, the disease is acute. Without proper treatment, it becomes chronic with periods of remission and relapse. This pathology is characterized by increased tear production and the appearance of deep cracks in the corners of the eyes. Scaly or dry inflammation of the dermis of the eyelids usually develops in adult patients. Often it is the localization of general eczema.
Over time, the inflammatory process subsides. On the weeping dermis, keratinization appears and it begins to peel off. Then the skin returns to normal.
With long-term, chronic illness, the eyelids may thicken and turn out. Complete or partial loss of eyelashes is also observed.
Eyelid eczema can lead to complete or partial loss of eyelashes.
Eczema is not an infectious pathology. Therefore, despite its danger, it is not contagious.
Causes of eczema on the eyelid and around the eyes
It is not surprising that women experience symptoms of eyelid inflammation more often than men. After all, they use cosmetics. It often contains allergic agents and synthetic substances. They cause skin sensitization - its hypersensitivity to the action of irritants. This condition of the dermis triggers allergic reactions.
Eczema is also provoked by:
- dust;
- insect secretions;
- plant pollen;
- pet hair and excretions;
- use of certain medications;
- weak immunity;
- disorders in metabolism and hormonal secretion.
Inflammation on the eyelids of a child or adult appears with increased production of histamine and decreased functionality of the body's systems and organs.
Symptoms of the disease
Signs of developing eczema around the eyes:
- Reddened dermis of the forehead and eyelids.
- Severe itching and peeling of the skin.
- Swelling of the eyelids, painful sensations when touching them.
Cosmetics can trigger eczema.
As the disease progresses, a rash appears on the skin. After the blisters, papules and pustules burst, eczema becomes a weeping form. It is very dangerous, as it may indicate a bacterial infection of the wounds.
Signs of pathology during its prolonged course:
- Increased production of tear secretion.
- Burning and stinging in the eyes.
- The dermis on the eyelids becomes dry and may crack.
- With weeping eczema, the ulcers become covered with serous crusts.
When the disease becomes chronic, the eyelids thicken and turn out. These processes are accompanied by eyelash loss. The wounds and ulcers begin to suppurate and can become infected (seborrheic dermatitis).
Women often make this mistake: instead of seeing a doctor, they mask the inflammation with cosmetics. This worsens the condition of the dermis. It becomes additionally irritated, and erosions and cracks appear in the inflamed areas.