Amblyopia is a progressive decrease in visual acuity, the degree of which does not correspond to the condition of the eye itself. The eye could see, since the retina and the optic nerve, through which the signal is transmitted to the brain centers responsible for vision, are not damaged, but its vision decreases. This happens because the brain disconnects this eye from the process of vision. A person with amblyopia sees everything with only one eye, despite the fact that the visual analyzer of the second eye is fine. Loss of binocular vision leads to impaired orientation in space: it is difficult for a person with amblyopia to estimate the distance to objects, their depth and volume. The load on the second (seeing) eye increases, which can lead to headaches, pain in the eyes, etc.
Amblyopia cannot be corrected using optical aids (glasses and lenses).
Etiology
The main reasons for the development of such pathology as “lazy eye”, especially in children under 10 years of age, include:
- Strabismus.
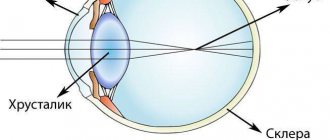
- An increased level of ametropia is changes in the lens of the eye that affect the refraction of rays. For this reason, the back focus of the image, which is perceived by the organ of vision, does not fall on the retina as it should.
- Cataract.
- Drooping eyelid. Due to the covered palpebral fissure, the required amount of light rays does not penetrate into it, which is required to clearly distinguish objects.
All of the above reasons can be either congenital or acquired. But, several specific conditions have been identified that can play the role of a predisposing factor to the onset of the disease Amblyopia or lazy eye syndrome in infants:
- Premature birth.
- Low birth weight newborn.
- Cerebral palsy.
- Mental retardation.
- Heredity.
- Bad habits of a woman during pregnancy.
While the child is still very young, it is very difficult to identify any visual disorders. Most often, amblyopia is diagnosed in children starting at 3 years of age.
Causes
Genetic aspects. If one parent has a history of amblyopia, the child is more likely to develop it. A number of inherited diseases are accompanied by amblyopia • Benche's syndrome (*141350, В): asymmetric facial hyperplasia, strabismus • 156190, В, reciprocal balanced translocation (8; 11) (q24.3; p15.1); mental retardation, short stature, amblyopia • Kaufman syndrome • Ophthalmoplegia with ptosis and miosis (*258400, r).
Risk factors. Amblyopia most often occurs in families with asymmetrical refractive errors, severe uncorrected refractive errors and strabismus.
ICD 10 online
Version 4 (revised 2020)
The International Classification of Diseases is the main classification of diseases by letter codes, which is periodically (once every 10 years) revised under the leadership of WHO. The ICD is a normative document that ensures the unity of methodological approaches and the international comparability of materials.
ICD 10 is used to convert verbal diagnoses of diseases and other health problems into alphanumeric codes that make data easy to store, retrieve, and analyze.
Classification and pathogenesis
Considering the time of onset of the disease, the disease is divided into:
- Primary (congenital).
- Secondary.
Considering the causes of the disease, several types of secondary amblyopia are considered:
- Strabismatic (dysbinocular).
- Obscuration (deprivation).
- Refractive.
- Anisometropic.
- Hysterical.
- Mixed.
Amblyopia, the causes of which can be very different, has one mechanism for the development of the pathological process, associated with processes of deprivation of shaped vision or incorrect binocular connections, causing a functional decrease in central vision.
Dysbinocular amblyopia based on a specific dysfunction of binocular vision. The disease begins against the background of prolonged suppression of the organ of vision. The lazy eye of a strabismic nature has 2 variants of its course: with central fixation, in which the fixing areas are located in the center of the retina. Or with a non-central one - when any part of the retina acts as the fixing area. The tisbinocular type of disease with a non-central fixation point is found in 70-75% of patients. The further treatment course will depend on the exact form of strabismic amblyopia.
Deprivation amblyopia occurs due to congenital or early-life opacities of the optical media of the eye. The disease is determined mainly in those people in whom blindness progresses, even after getting rid of the main cause of the disease, as well as in the absence of structural changes in the posterior part of the eyeball.
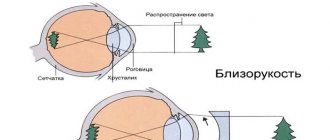
Refractive amblyopia is associated with abnormal refraction that cannot be treated. The disease is based on a prolonged projection of a blurred image of surrounding objects onto the retina.
Anisometropic amblyopia occurs when the refraction of both eyes is different, which is why there is an impressive difference in the size of the reflected bodies on the retina of the right and left eyes. This problem does not allow us to form a single visual image.
A very rare type of disease that develops against the background of some effect is considered hysterical amblyopia (blindness of a psychogenic nature). In such a situation, the degree of vision loss can be either partial or complete.
Considering the degree of vision loss, experts classify amblyopia into the following types:
- Low degree amblyopia (0.4-0.8).
- Moderate amblyopia (0.2-0.3).
- High degree amblyopia (0.05-0.1).
- Amblyopia of a very high degree (from 0.04 and below).
Amblyopia, which can only be diagnosed by a qualified ophthalmologist, can be detected in one eye (unilateral) or in both eyes at the same time (bilateral).
Thanks to all of the above classifications, it is easier for doctors to make a diagnosis, which means that treatment for amblyopia can be selected as accurately as possible.
Therapy - pleoptics
This is the term for the treatment of amblyopia. Therapy can be divided into active and passive.
In special pleoptic rooms, both simple exercises and training on special devices are performed. Amblyopia is most treatable in preschool age. At school and in adult life, the disorder is extremely difficult to correct.
To improve visual acuity at home, you can use several simple exercises related to active treatment. The main condition is the optimal correction of refractive errors using glasses. Covering the better seeing eye forces the weakened eye to act.
There are different types of occluders:
- Occluder patch - the occluder is glued to the skin of the face, ideally covering the better-seeing eye. On the inside of the face it should reach the middle of the bridge of the nose. At night, the occluder is removed and cream/lotion/oil is applied to the skin. The advantage of these occluders is perfect coverage of the eye.
- Rubber occluder - with a suction cup for glasses. With such occluders, there is a possibility that a child could peep if they are not attached correctly to the glass.
- A plastic occluder has the same principle and risks as a rubber one.
- Occlusive contact lenses are available only with a prescription from an ophthalmologist.
Peoptics helps correct vision problems that cause disturbances in the functioning of the cerebral cortex
Pleoptics methods
Active pleoptic treatment at home
Simple pleoptic active treatment can also be carried out at home when the weak eye is subjected to “workload”. Touch and touch are used for these purposes. Therapeutic methods include the following types of exercises:
- assembling sets of parts (construction set), folding colored construction blocks, mosaics, modeling from plasticine, assembling beads;
- pricking holes with a blunt needle - the child pricks out dots on a previously drawn line, the contours are gradually drawn thinner and weaker;
- drawing with a pencil through transparent paper, drawing lines with colored pencil, brushes, watercolors.
Muscle trainer - a simulator for a lazy eye
First, simple images are drawn, later complex ones depending on the abilities of a particular patient - exercises on the line: with a colored pencil on the line; filling the space between the lines with a colored pencil, gluing small details onto the line.
It is recommended to use lined paper. You should prepare in advance various forms of colored paper that will be glued to the line.
Amblyotrainer was created to improve visual function
Cutting, drawing and other activities
Along with the above options for training the affected eye, you can use other activities. These include the following classes:
- construction sets: puzzles, small Lego sets, computer games (limited time);
- coloring - filling an empty area with color, creating large and simple images, sequentially moving to smaller and more complex images;
- connecting dots - on paper, draw several dots, when connected, the child will get a specific object (fungus, flower);
- embroidery on paper or fabric with a blunt needle and colored thread (small holes should first be made on the paper);
- board games: lotto, checkers;
- books - a small child describes a picture he sees, school-age children read texts with different letter sizes.
At home, activities with bright objects of different shapes and sizes (designer parts, appliqués, beads) help stimulate the child’s visual function
Clinical picture
To understand what lazy eye is, you need to know how the disease progresses. In the case of the development of refractive disorders, the disease may occur without the manifestation of any symptoms, especially for children. Often, a similar pathology is diagnosed in young children after 3 years of age.
The onset of pathology formation can be suspected in the following cases:
- The discrepancy in visual acuity with farsightedness is 0.5 diopters or more.
- With developed astigmatism, this difference exceeds 1.5 diopters.
- Myopia – discrepancy of more than 2 diopters.
Lazy eye syndrome, when vision is impaired in both eyes, occurs evenly during:
- Myopia greater than 8 diopters.
- Farsightedness more than 5.
- Astigmatism more than 2.5.
Amblyopia, the symptoms of which are not felt by the sick person and are not corrected by glasses, can affect adaptation to a dark environment, color perception and the formation of strabismus.
Amblyopia - characteristics
The essence of the development of amblyopia is the inability to correctly receive images in the affected eye. The eye is not properly stimulated by the visual center in the brain, resulting in the perception of the affected eye being suppressed. A situation arises when, due to the lack of visual perception in one eye, it reaches a state of lack of connection between the eye and the brain.
Often this condition is associated with strabismus, which causes the eyes to focus at two different points rather than one. The outcome of this disease is a deterioration of binocular function and, in the vast majority of cases, the inability of binocular vision, that is, the inability to create the sensation of depth that creates a three-dimensional image.
When amblyopia develops in children, the causes may lie in strabismus or the difference between nearsightedness and farsightedness in the two eyes, or may also be the result of other pre-existing eye diseases, such as cataracts, ptosis (drooping of the upper eyelid) and refractive problems.
What is amblyopia or “lazy eye” in children?
Typically, this disorder occurs when the eyes are not interconnected when sending a single image to the brain. In the case of strabismus, one eye is pointed in a different direction than the object the person is trying to look at. The brain's natural tendency is to ignore an out-of-focus image, thus leaving the eye sending that image unused. Over time, this situation can lead to displacement of the weakened eye, resulting in amblyopia.
Symptoms and manifestations of amblyopia
How does amblyopia manifest?
The disorder manifests itself depending on the cause of its occurrence. One of the reasons is strabic amblyopia (caused by strabismus):
- in an adult, strabismus causes double vision, in contrast to this, the child’s brain is still malleable and is able to suppress double vision, which results in amblyopia;
- when reading, the child uses only the healthy eye;
- decreased reading speed;
- difficulty reading small letters.
Another cause is anisometropic amblyopia:
- there is a big difference in diopters in one and the other eye;
- the child tends to use predominantly the healthy eye, which becomes dominant, and the second one “goes dull.”
The reason may be mixed - consist of a combination of several factors described above.
The cause of amblyopia is a malfunction of the visual analyzer in the child’s brain.
The general symptoms of the pathology are as follows:
- low spatial perception;
- low spatial acuity;
- low sensitivity to contrast;
- decreased visual acuity;
- decreased perception of contours;
- diplopia;
- inability to perceive 3D.
How can you determine if a child has amblyopia? There is a screening test that can detect eye disorders fairly easily, even in very young children. The test should be carried out at a time when the child is rested and in good spirits. But keep in mind that this screening test does not replace a professional examination by a doctor! It consists of the following:
- Glue the large letter “E” onto thick paper and cut it out, give it to the child;
- attach to the wall in a well-lit place (preferably at the child’s eye level) 2 lines of the letter “E” written in different directions;
- cover the child's eye with a scarf or occluder and sit him at a distance of 5 m from the wall;
- make sure that the baby is not peeping;
- point to individual letters attached to the wall;
- the child rotates the cut out letter “E” in the direction you indicated;
- if the baby turns the letter correctly, you can start examining the other eye;
- If you find that your child's vision is much worse in one eye than in the other, seek professional help.
CONJUNCTIVAL DISEASES (H10-H13)
H10 Conjunctivitis Excluded: keratoconjunctivitis (H16.2) H10.0 Mucopurulent conjunctivitis H10.1 Acute atopic conjunctivitis H10.2 Other acute conjunctivitis H10.3 Acute conjunctivitis, unspecified Excluded:
ophthalmia of the newborn NOS (P39.1)H10.4 Chronic conjunctivitisH10.5 BlepharoconjunctivitisH10.8 Other conjunctivitisH10.9 Conjunctivitis, unspecifiedH11 Other diseases of the conjunctivaExcluded: keratoconjunctivitis (H16.2)H11.
0 Pterygium Excludes: pseudopterygium (H11.8)H11.1 Conjunctival degeneration and depositsH11.2 Conjunctival scarsH11.3 Conjunctival hemorrhageH11.4 Other conjunctival vascular diseases and cystsH11.
8 Other specified diseases of the conjunctivaH11.9 Disease of the conjunctiva, unspecifiedH13* Lesions of the conjunctiva in diseases classified elsewhereH13.0* Filarial infestation of the conjunctiva (B74.- )H13.
1* Acute conjunctivitis in diseases classified elsewhereH13.2* Conjunctivitis in diseases classified elsewhereH13.3* Ocular pemphigoid (L12.- )H13.8* Other conjunctival lesions in diseases classified elsewhere
Diagnosis
To establish a diagnosis, you need to go through several simple procedures. To begin with, the doctor examines the patient, determining the general condition of the eyeballs, reaction to light and the condition of the eyelids. Next comes a series of manipulations, like:
- Visiometry.
- Detection of color fields.
- Perimetry.
- Determination of refractive power.
If a person is diagnosed with a severe disease, it is necessary to supplement the diagnosis with an examination of the condition of the fundus, microscopic examination, as well as checking the condition of the lens and vitreous body for the degree of their transparency. If a loss of transparency is detected, then in this case an ultrasound is required.
When the cause of severe pathology lies behind strabismus, doctors determine the angle using the Hirschberg method. In addition to all this, patients may be prescribed tonometry and consultation with a neurologist.
Risk factors for developing pathology
- Strabismus - occurs most often, which is caused by prolonged suppression of the picture perceived by the squinting eye as it processes information in the brain.
- Astigmatism or farsightedness is blurred vision in both eyes, which is caused by anisometropia - the phenomenon of unequal refractive indexes. Each eye perceives a different visual wavelength. This type of disease is called refractive amblyopia , and the severity of the disease directly depends on the magnitude of the deviation of the refractive index in the affected eye.
- Cataracts, hemophthalmos, corneal opacities , serious changes in the structure of the vitreous body and other damage that prevent light from reaching the retina.
- Nystagmus is an involuntary movement of the eyeballs of a neurological nature.
- Ptosis is a pathology of the muscles of the adnexa with drooping of the upper eyelid.
Causes
- Pathological development of the eyeball in the prenatal period.
Long-term clouding of the lens and cornea.
Difference in refraction (in one the refraction is much greater than in the other). Perhaps the wrong treatment was given.
Strabismus is the most common cause.
One eye has a high degree of farsightedness or astigmatism.
Absence or incorrect fixation of the eye.
Underdevelopment of photoreceptors of retinal neurons, in particular cones, which leads to color blindness.
Risk factors include:
- Lack of newborn weight.
The existence of strabismus, ametropia.
Cerebral palsy.
Mental retardation.
Neonatal retinopathy (retinal damage associated with vascular pathology).
Prematurity.
Symptoms of amblyopia can be recognized by observing your baby.
Strabismus develops, impaired coordination of movements, decreased visual acuity, impaired orientation in unfamiliar rooms, tilting to the side towards an object with the healthy eye, difficulty perceiving three-dimensional objects, deviation of the diseased eye to the side or closing it when reading.
If these symptoms appear, you should contact an ophthalmologist who will prescribe the necessary treatment.
Methods of therapy
It is worth noting that treatment of amblyopia is completed with a positive result in younger patients. Amblyopia in adults takes much longer and is more difficult to treat than in young children. The reason for this predisposition depends on the fact that restoration of the functioning of an already formed component of the visual analyzer in adults is almost impossible. All eye dysfunctions that were not cured in childhood are almost impossible to correct in adults.
In mature people diagnosed with lazy eye syndrome, the disease inhibits the mobility of the organ so much that conservative treatment methods are inappropriate due to their low effectiveness. For example, children can also temporarily switch off the affected eye from work using a special curtain. This tactic will force the sore eye to work. For adults, this treatment is not suitable.
The irreversibility of the pathology develops by the age of 12, so it is better not to delay the treatment of amblyopia, which can be treated in childhood, and consult an ophthalmologist in time.
Before starting any therapeutic measures, it is necessary to exclude all pathologies that can cause loss of vision.
Using standard methods, which consist of all methods to eliminate dysfunction of the visual organs, you can try to cure amblyopia. To begin with, occlusion of the primary functional eye is prescribed. That is, the working eye is limited in receiving visual signals using an artificial limiter.
After this, the doctor performs artificial stimulation of the “lazy eye” using bright periodic light flickers, which act on the diseased eye as an external irritant. Such a procedure is aimed at restoring the normal balance of parallel and identical perception of data from vision analyzers, and also serves as an impetus for creating an even distribution of visual load on both organs of vision.
If such tactics show high effectiveness, laser vision correction is performed in the future.
Regarding the hysterical type of illness, doctors say that it disappears as unexpectedly as it appears. In addition, he responds well to treatment, with the help of sedatives and psychological support from professionals.
Amblyopia and its pronosis
The key to any recovery is not only the early detection of the disease, but also the impeccable implementation of all the ophthalmologist’s recommendations.
Important! The greatest effect of treatment occurs before the child reaches 6-7 years of age.
After this age, you can only count on partial recovery. In adults with amblyopia, the loss of vision is irreversible.
Poor treatment results are associated with ignoring recommendations for wearing glasses, the child’s reluctance or fear of visiting a doctor. As a result, time is missed when the optic nerve is not yet formed and can be easily corrected.
If the disease is left to run its course, the outcome will be complete blindness, especially in adulthood.
Amblyopia symptoms
Binocular vision impairment
The main symptom of amblyopia is blurred vision in one eye. The eye could see, but ceases to participate in the process of vision
Headache
Since with amblyopia one eye does not participate (or only slightly participates) in the visual process, the load on the second (seeing) eye increases. This can lead to headaches.
More about the symptom
Stinging in the eyes
Pain in the eyes is also a consequence of increased stress on one eye.
More about the symptom
Disorientation in space
Loss of binocular vision leads to impaired orientation in space: it is difficult for a person with amblyopia to estimate the distance to objects, their depth and volume.
Symptoms
There are different degrees of manifestation of the disease; with a mild course of the disease, symptoms may not be expressed. Experts have identified individual symptoms in childhood and adulthood.
Amblyopia in children manifests itself in the following symptoms:
- Strabismus.
- Tilt of the head when reading, or closing one eye.
- Poor coordination of movements.
Symptoms in adults are different:
- Double vision.
- Veil, vagueness.
- Sudden deterioration in vision for a long period or a couple of hours.
At the initial level of development, the patient is not aware of the existence of the disease and only accidentally notices the different optical powers of the eyes.
Forecasts
The final prediction of the outcome of the disease, which the doctor can give to the patient, depends on the following conditions:
- Indisputable compliance by the sick person with the recommendations prescribed by the attending physician.
- Diagnosed type of disease.
- Adequacy of eye fixation.
- Initial visual acuity (before illness).
- The age of the sick person at the time of treatment.
- The method of treatment chosen by the doctor.
Amblyopia of the obscuration type, which manifests itself on one side, can affect visual impairment if medical assistance was not provided during the first 3 months of the child’s life. The chances of eventually achieving visual acuity of 0.4 diopters or even higher can only be guaranteed after successful surgery during the first 2 months of life. At the same time, forecasts regarding binocular vision can hardly be called optimistic. Bilateral lesions have the same prognosis, but after the baby reaches six months of age. If treatment is started during a critical period of pathology progression, the prognosis will be disappointing.
Strabismus that remains untreated can cause sensorimotor abnormalities, the most significant of which is considered to be the eccentric type. It is this that has a negative effect on the final outcome and significantly prolongs the duration of treatment.
One of the main conditions is the patient’s undisputed compliance with all medical prescriptions. Timely diagnosis and treatment are of great importance. For example, in a patient over five years old, the likelihood of changing an already present form of strabismus into one that would allow achieving equal visual acuity in both eyes at once is very low.
Without progressive therapeutic correction of strabismus, the fight against amblyopia itself becomes difficult. In such a situation, there is no guarantee that there will be no relapses of the disease in the future, which is why doctors prescribe periodic studies at different times after completion of therapy.
Amblyopia. Causes, symptoms, treatments
Amblyopia is predominantly a childhood disease, affecting an average of 2% of the population.
One of the eyes does not participate in the visual function. Hence the common name - “lazy” (“dumb”) eye. There is no pathology of the visual organs with amblyopia. The disease manifests itself as a limitation of the ability of adaptation and sensitivity of one eye. It is very rare that both eyes do not function.
How is the disease classified?
Amblyopia can be congenital or acquired. The second type of disease has several varieties. Among them:
- Strabismic or dysbinocular. Manifests itself as suppression of the visual image of one eye (suppression). In 70% of cases, amblyopia of this type is detected with incorrect fixation. In this case, the retina is fixed in any area, with the exception of the central region. This case is considered separately and is called correct (central) fixation.
- Obscuration or deprivation. A characteristic feature is clouding of the optical environment of the visual organs. Suspicion of the occurrence of this type of disease falls if eliminating the causes of amblyopia does not help restore vision and no defects are visible in the fundus area.
- Refractive. A fuzzy image is projected onto the retina when you look at an object. Because of this, the refraction of light rays becomes unnatural.
- Anisometropic. The creation of a complete picture from images received from both eyes is disrupted. This manifestation is characteristic of different refraction of light rays in both eyes. The result of this is the display of the visible object through each retina in different sizes.
- Hysterical amblyopia or psychogenic blindness. This is a rare type of disease that occurs against the background of a state of strong excitement.
Any of these types of disease manifests itself as a limitation of visual activity, which manifests itself to varying degrees (weak - 0.4-0.8; medium - 0.2-0.3; high - 0.05-0.1; very high (below 0.05).
Amblyopia code according to ICD-10
H53.0 Amblyopia due to anopsia. Amblyopia caused by anisometropia, visual deprivation, strabismus.
Why does amblyopia occur?
Each type of amblyopia has its own list of causes. Let's consider them separately.
Causes of functional amblyopia
The functional type of disorder can occur for the following reasons:
- Limitation of visual activity.
- Cataract of congenital or acquired type.
- Low position of the eyelid, as a result of which the palpebral fissure is completely closed (blepharoptosis).
- Cloudiness of the cornea.
- Hemorrhage in the anterior chamber of the eye (hyphema).
- Blood in the vitreous body (hemophthalmos).
- Uncontrolled opening and closing of the eye (occlusion).
- Strabismus in one eye.
- Changing the refraction of light rays.
Functional disorders include anisometropic, deprivation and refractive amblyopia. Based on the causes of their occurrence, treatment is prescribed.
Causes of organic amblyopia
The following factors lead to organic amblyopia:
- There is no color vision. Only black and white colors differ.
- Part of the eye shell is missing.
- Multiple sclerosis.
- Retinal defect in premature infants.
- Degenerative image focusing disorder.
- Underdevelopment of the optic nerve.
- Thinning of the cornea.
- Clouding of the eye within the optical media.
- Scarring of the central part of the retina.
- Inflammation of the optic nerve.
- Oscillatory eye movements with a high frequency of an involuntary nature.
- Congenital brain tumor.
Like functional disorders, amblyopia caused by a disease of the visual organs is treated by eliminating the cause.
Causes of hysterical amblyopia
Hysterical amblyopia is a characteristic manifestation of psychological deviation. It is caused by a lack of mental comfort and an exaggeration of the significance of existing diseases. Doctors working with the psyche are involved in her treatment.
Causes of refractive amblyopia
Refractive amblyopia is the result of untimely treatment of certain diseases of the visual organs. These include farsightedness, nearsightedness, and a defect in the shape of the cornea or lens. If such manifestations are not corrected for a long time, for which glasses or contact lenses are prescribed, they can lead to amblyopia.
Risk factors
Amblyopia most often affects children aged 6 to 8 years. Those who have strabismus or impaired visual stimulation are more susceptible to developing the disease. Risk groups also include children with the following deviations:
- Prematurity.
- Low birth weight.
- Defect of the retina of the eyes in a newborn.
- Cerebral paralysis.
- Delays in mental development.
- Heredity in terms of cataracts, strabismus, anisometropia.
If the child’s mother smoked during pregnancy, took alcohol and took medications, then the risk of amblyopia increases.
Amblyopia symptoms
The initial stages of the disease may be asymptomatic. If signs of amblyopia are present, the child may not understand this. Therefore, at a young age, parents should think about the presence of amblyopia if the baby has the above diseases. An older child may notice the following symptoms indicating illness:
- Visual acuity decreases.
- Vision correction doesn't help.
- In an unfamiliar place, he cannot find his way.
- One eye deviates to the side.
- Reading or focusing on an object is accompanied by closing one eye or tilting the head.
- His color perception is impaired.
- The eyes cannot adapt to the dark.
Hysterical amblyopia is a common manifestation in adults against the background of emotional outbursts. A sharp deterioration in vision, the duration of which varies from several hours to months, indicates its occurrence.
Sometimes amblyopia can look like this:
There are cases when the disease cannot be cured in childhood:
As we see, the user got rid of the disease as an adult using a computer program.
Diagnosis of amblyopia
When diagnosing a disease, the causes of its occurrence, the type and degree of deviation are identified. The following studies help make an accurate diagnosis:
- Visual inspection. The closure of the eyelid, deviation of the eyeball, and reaction to the light source are detected.
- Checking visual acuity. Indications are measured both with and without corrective devices.
- Testing for color perception.
- Detection of limitations and defects in the visual field (periphery).
- Testing for refraction of light rays.
- Examination of the fundus using an ophthalmoscope and a slit lamp.
- Ultrasonography.
- Establishing the angle of strabismus.
- Measuring intraocular pressure.
- Study of the retina using light stimuli.
A comprehensive study helps to make a correct diagnosis. Based on the results obtained, the doctor prescribes treatment.
Treatment of the disease
If amblyopia is detected in a child under the age of 7 years, it can be successfully treated. The disease diagnosed at the age of 12 has practically no treatment. The forecasts here are disappointing. When choosing a treatment regimen, the ophthalmologist is guided by the cause of the disease. The treatment method corresponds to the type of diplopia:
- Isoametropic. For its treatment, a complete correction is used, which changes a month after the start of treatment depending on the results obtained. If after 2 years of wearing glasses vision does not improve, then a deviation in the function of the eye adaptation is diagnosed. Glasses and lenses are replaced by active vision therapy. Prismatic glasses and computer programs are used to correct vision.
- Anisometropic. Treated with full optical correction. The strength of the lenses is gradually increased for some patients to get them used to them. In many cases, such an event is enough for vision to be fully restored. If this does not happen, active visual therapy is prescribed.
- Deprivation. Early surgical intervention is necessary with intervals between operations (if there are several) of 2 weeks. To reinforce the effect, glasses are assigned for a while.
- Dysbinocular. Complete optical correction is the first step in treatment. In addition to it, active visual therapy or eye-closing procedures (occlusion) are prescribed. If the angle of strabismus exceeds 10°, then a necessary measure in this case is surgical intervention. In total, treatment takes from 6 months to 1 year.
Here is one possible treatment regimen:
If treatment began on time and the patient followed all the doctor’s recommendations, vision can be restored completely. Otherwise, vision may deteriorate to the point of complete blindness. Amblyopia that goes untreated for a long time can lead to other diseases.
Prevention of amblyopia
Prevention of amblyopia involves timely treatment of the diseases that cause it. Children at risk should undergo periodic medical examinations starting from 1 month of life. If you want your children to be free from the possibility of amblyopia, lead a healthy lifestyle during pregnancy and do not take medications without a doctor's prescription.
Remember that amblyopia does not go away on its own with age. Most often, it is treated with the use of glasses, which can then be discarded with the permission of the doctor.
Source: https://VseProGlaza.ru/bolezni/ambliopiya/