Treatment of nystagmus should begin only after excluding its traumatic cause of development. The fact is that instability of the position of the eyeball is a characteristic clinical sign of brain injury (bruise or concussion). Therefore, if symptoms appear after the baby falls, you need to urgently call an ambulance team. Congenital nystagmus in children is provoked by intrauterine factors that have a negative impact on the development of the fetal neural tube. Those. prerequisites are laid in the early stages of pregnancy. However, violent labor and prolonged hypoxia during childbirth can also provoke a similar condition.
What it is - nystagmus in children, what causes its symptoms and how treatment can be carried out is described in the proposed material.
Horizontal nystagmus in children under one year old
“Doctor, what should we do - our baby’s eyes are “running”?! With this question, you need to urgently contact a specialist, because “shifty” eyes are a sign of a rather dangerous disease called nystagmus.
During nystagmus, the eyes make rapid movements, similar to the oscillations of a pendulum.
Horizontal nystagmus in children should not be confused with a nervous tic: yes, the process, like a tic, is uncontrollable, but a tic is an involuntary contraction of a single muscle, and with nystagmus the entire eyeball constantly twitches.
So, a baby at the age of one month begins to focus his gaze on the objects and people that surround him. During this period, you need to be extremely attentive to the development of vision in the baby, so as not to miss the onset of nystagmus. The baby is unable to understand or explain what is wrong with him, but in fact, due to nystagmus, his perception of the image is distorted. With nystagmus, children under one year old often feel dizzy and visual acuity begins to decrease, since the picture in front of the affected eye twitches and it is impossible to either fix or focus the gaze.
Determination of visual acuity in children
Visometry in children, especially young children, is a rather labor-intensive task. For example, in newborns, the presence of vision is assessed using behavioral methods. At an older age (2-5 months), the child’s sensitivity to bright light is determined. Even later, they show a ball of bright red color and 4 cm in diameter. I hang it against the background of the window on a thread and mark the distance at which the baby fixes his gaze on it and begins to follow or reach with his hand. At the age of six months, the diameter of the balls can be reduced. To roughly assess visual acuity, you can also show white balls of different sizes on a dark background. At the age of over three years, special children's tables are used with objects (optotypes), which are presented in the form of animals, toys, cars (tables by Aleinikova and Orlova).
Causes of congenital horizontal and vertical nystagmus of the eyeball in a child
Nystagmus of the eyeball in a child, as a rule, is congenital, but can also develop as a result of injuries, infectious diseases, or acquired lesions of the central nervous system.
In both cases, nystagmus manifests itself very early - before the age of six months.
The causes of horizontal nystagmus in children older than six months are directly related to nerve abnormalities or diseases of the nervous system as a whole. For example, the cause of constant eye twitching can be diseases of the vestibular apparatus, which is located in the inner ear and is responsible for our balance and orientation in space.
Less commonly, the causes of vertical nystagmus are temporary, and when the irritant factor disappears, the twitching of the eyeball also goes away. For example, when the body spins in one place for a long time or when water gets into the ear while swimming, sometimes as a reaction to certain medications.
A child with nystagmus's eyes may move in a variety of ways. Firstly, the very nature of these “twitches” can vary from oscillations to jerking movements and even rotations.
Previously, it was believed that if horizontal nystagmus is constant, it is almost impossible to treat a child for it. Nowadays, there is a way to rid the baby of these oscillatory eye movements.
Modern treatment methods and surgical innovations make it possible to “block” congenital horizontal nystagmus and significantly improve visual acuity.
Symptoms of small-swing and rotatory horizontal nystagmus
Parents need to remember that small-scale horizontal nystagmus is involuntary movements that the baby is not able to control. This problem cannot go away with a wave of a magic wand - treatment is necessary!
Therefore, you should contact a specialist urgently if the following symptoms appear:
- You notice that the baby holds his head unnaturally, tilting it to the side. This condition is called ocular torticollis, and its nature lies in the fact that the child finds a head position that helps to almost not feel the oscillatory movements of the eyes. The child tilts his head unconsciously, driven by the desire to increase visual acuity.
- The baby's eyes make the same repetitive movements, or each eye makes different movements.
- The eyes move unnaturally rhythmically or, like a pendulum, swing left and right, diagonally, up and down, or rotate, converging towards the nose.
- The speed of movement in both eyes is the same or different.
- The baby has difficulty focusing his eyes on the toy.
- Increased sensitivity to light, the child begins to cry and rub his eyes in bright light.
- With horizontal rotatory nystagmus, visual acuity is reduced, the child squints and moves closer to objects to examine them.
- An older child may complain of “ripples” in the eyes, cloudiness, blurred images, and frequent dizziness.
- Sometimes hearing loss and clumsiness and clumsiness may occur due to imbalance.
Symptoms
The symptoms of the disease are quite noticeable. These are oscillatory eye movements that cannot be controlled. The eyes can move in a circular direction, vertically or horizontally. The gaze does not fixate the object in question, but rather “slips” past it. In this regard, a number of problem conditions develop:
- Visual acuity decreases;
- Strabismus develops, a feeling of double vision occurs;
- Photosensitivity appears;
- There is a feeling of dizziness, instability, nausea;
- Muscle tone decreases.
You can often notice an unnatural position of the patient’s head, which “helps” reduce the amount of vibration of the eyeball. In some cases, nystagmus manifests itself in unilateral hearing loss.
The amplitude of movements during nystagmus can vary depending not only on the position of the head or direction of gaze, but even on the degree of fatigue of the person or level of concentration.
Installation, vertical and horizontal nystagmus
Nystagmus that occurs immediately after the birth of a child is called congenital (genetic or manifested as a result of birth trauma), and that detected at any other age is called acquired, since it is associated with diseases of the nervous system. The congenital type of disorder accounts for the overwhelming majority of all cases of nystagmus.
Depending on the course of the disease, the nature of nystagmus is defined as physiological (there is a factor that causes irritation of the nervous system) or pathological (the result of various diseases or pathologies of the child’s body).
The physiological form of nystagmus is divided into the following conditions:
- Optokinetic form - the eyeball seems to “jump”. This form is also called the railway form: imagine that you are standing on the platform and a passenger or freight train is passing in front of you. When you try to look at it, your eyes make jerky movements from side to side. The same movements are made by the eye of a sick child, but not in an attempt to see fast-moving objects or changing landscapes outside the train window, but constantly.
- Installation nystagmus - jerky twitching of the eyeball is noticeable when looking away to the side. This is due to weakness of the outer eye muscles.
- Vestibular form - occurs due to infections of the inner ear (in which the vestibular apparatus is located) or as a consequence of Meniere's disease (a non-inflammatory disease in which the amount of lymph circulating in the inner ear increases).
It is also important to correctly determine the nature of the movement. They may be similar to the movements of a pendulum, at regular intervals; jerky, similar to rhythm (with slow and fast intervals); mixed (when looking forward - oscillatory movements, and to the sides - jerky).
Even the range of oscillations of the eyeball is taken into account: small - (up to 5°), medium - (from 5 to 15°), large-scale (above 15°) nystagmus.
If the eye movements performed during nystagmus are of the same type, it is called associated, and if they are different, it is called dissociated. If vertical nystagmus occurs in only one eye, it is called monocular.
As mentioned above, the main problem with horizontal installation nystagmus is a violation of visual perception in the child. If nystagmus is congenital, then visual acuity decreases from 0.3 to 0.1 diopters. Small-caliber vibrations of the eye make the ability to see slightly higher than large-caliber ones.
Based on the direction of movement of the eyeballs, the following is revealed:
- horizontal nystagmus - synchronous movement of the eyeballs horizontally (right-left);
- rotational nystagmus - the eyeballs move in a circle;
- diagonal nystagmus - the eyeballs move diagonally;
- vertical nystagmus - the eyeballs move up and down.
Pathological nystagmus is divided into:
- fixation - it is caused by various pathologies of the eye media, leading to blindness or amblyopia;
- peripheral - occurs against the background of diseases of the inner ear;
- central - develops as a result of infections, injuries, brain tumors.
The most common is congenital, fixation nystagmus, other forms are much less common.
Visual acuity test results
Visometry results are expressed in ordinary or decimal fractions. In Russia, Germany and the CIS countries, decimal fractions are used, while in other regions the result is presented as an ordinary fraction, the numerator of which indicates the distance to the optotype (20 feet or 6 meters), and the denominator indicates the distance from which the object can be determined healthy eye. A normal rate might look like this: 1.0, 6/6, 20/20.
To make it easier for the patient to understand, it can be explained that decimals are easy to convert to percentages. For example, with a visometry index of 0.8, vision is preserved by 80%. However, this statement is not entirely true, because the value of visual acuity does not change directly, but rather logarithmically. That is, a decrease in visual acuity from 0.9 to 0.8 is less noticeable for the patient than the same decrease, but with an initial vision of 0.2.
According to WHO, visually impaired patients include people whose visual acuity is less than 0.3 (20/60, 6/18) but higher than 0.1 (20/200, 6/60). Also included in this category are patients with a narrowing of the visual field of less than 20 degrees in the better seeing eye or with the best correction.
The diagnosis of blindness is made when the indicators decrease to less than 0.05 (6/120, 20/400) or in the case of a narrowing of the visual field to 10 degrees or more. This condition in most countries is defined as practical blindness, that is, a person is deprived of the ability to perform most professional activities, and is also limited in movement and is not always able to take care of himself. In the European Union and the United States, this diagnosis is made when visual acuity decreases to less than 0.1 (6/60, 20/200) or when the visual field narrows to less than 20 degrees, which cannot be corrected medically.
When conducting isometry using tables, special attention should be paid to compliance with standards (distance to objects, illumination, time parameters). Most oculists are inclined to believe that illumination of 700 lux is quite sufficient. To make it easier to comply with standard conditions, you can use a Roth apparatus, which is a special lighting case with mirrors. Visometry to study distance vision is carried out from 5 meters or 6 meters. This distance is optimal, since there is no strain on accommodation, that is, the study can be performed at any age, even with senile weakening of accommodation (presbyopia).
To assess near vision, the distance is reduced to 33 cm. When selecting glasses for optical correction, this value may vary slightly depending on the expected distance between the eye and the object.
To measure visual acuity, the patient is seated in a chair at the required distance from the table. To perform visometry, one eye should be closed and then the opposite eye to assess monocular visual acuity. Next, a binocular assessment is possible, which is most often higher than the previous indicator. This is what is used when selecting glasses or contact lenses.
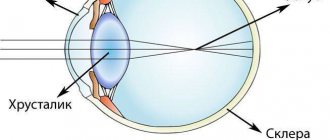
If the cause of decreased visual acuity is abnormal refraction, then an optical correction is selected that maximizes vision. If the patient already wears glasses or contact lenses, then in the process of visometry it is possible to assess their consistency.
Additionally, you can perform a pin-hole test, which is performed for differential diagnosis. If the presence of a diaphragm increases the clarity of the image, then we can say that the cause of decreased vision is a refractive error. Otherwise, the cause of decreased visual acuity may be damage to the retina or optic nerve. However, if the indicators deviate greatly from the norm, this test becomes less informative.
Visual acuity results are usually presented in the form of the following symbols:
Visus (visual acuity) OD (right eye)/OS (left eye)=1.0/1.0 or Vis OU (both eyes)=0.6.
If the patient has difficulty determining the optotypes of the table, and it is impossible to conduct an objective examination, then approximately visual acuity is determined by showing fingers from different distances. The result is assessed by measuring the greatest distance from which the patient can distinguish two separate fingers. The recording will look like this: Visus OS = finger counting from 4 meters.
In the case when vision is so reduced that the listed methods are not suitable for determining its acuity, light perception is studied. This requires a point source of light, which is directed alternately into the eye being examined at different angles. In this way, the sensitive different segments of the retina are assessed. If the eye is able to correctly distinguish the movement of a light beam, that is, visual acuity corresponds to light perception with correct light projection, then in the protocol the entry has the following form: visus = 1/∞ plc (proectio lucis certa). This indicates preserved function of the optic nerve and retina and is an important prognostic criterion for the effectiveness of treatment of various diseases, such as cataracts. If the patient made a mistake in determining the direction of movement of the beam, then the protocol records: visus = 1/∞ pli (proectio lucis incerta), that is, there is light perception, but the light projection is incorrect. In the case of a complete lack of light perception, the inability to distinguish light from darkness, blindness is diagnosed and visus = 0 is recorded.
Causes of congenital vertical nystagmus in a child
The causes of nystagmus may be associated with a variety of disorders in the central nervous system. Infant nystagmus is congenital, and if after one month, from the moment the baby is born, the gaze still does not focus, then the problem is most likely associated with acute infections suffered during fetal development or with injury during childbirth.
The causes of acquired nystagmus are the result of inherited anomalies (Leber's disease - complete or partial death of the optic nerve) or a violation of the refractive power of the eye (myopia, astigmatism, cataracts, retinal diseases). Another genetic disease that causes vertical nystagmus is albinism. It is clearly manifested externally, since the hair, skin and iris of an albino child’s eye are practically devoid of coloring pigment. Because of this, the retina of the eye, unprotected from light rays, and the optic nerve itself suffer greatly, causing nystagmus.
In children aged from three months to one and a half years, a nodule spasm occurs (involuntary contractions, head nods), against the background of which nystagmus may develop. The cause of nystagmus in a child is usually a disease or tumor of the brain.
Acquired nystagmus is also associated with diseases of the inner ear, which can be caused by injuries, sometimes tumors, and Meniere's disease. All these reasons lead to severe irritation of the vestibular apparatus. In this case, nystagmus is manifested by deviation of the eyes away from the affected ear. For a baby, not only head injuries are dangerous (affecting the centers in the cerebral cortex that are responsible for “steering” the eyes), but also acute infectious diseases that affect the brain, in particular encephalitis or meningitis.
The causes of congenital nystagmus should be excluded at the stage of pregnancy planning, take special medications, and follow the doctor’s recommendations.
Diagnosis of nystagmus
Uncontrolled, constant movements of the eyeballs are visible to the naked eye, so parents themselves can identify the primary symptoms of the disease. But only a certified specialist can determine the cause of the disease after a thorough examination.
Also, to diagnose nystagmus, a child must undergo an examination by a neurologist.
A traditional examination by an ophthalmologist includes an assessment of visual acuity (tests using tables), but to correctly identify the cause of nystagmus and its type, an accurate diagnosis is needed:
- Electrophysiological studies (visual evoked potentials).
- Electroencephalography (EEG).
- Electroretinography is a safe examination of the retina in which a special lens with an electrode is placed in the child’s eye (after instilling a local anesthetic), and a second electrode is attached to the back of the head. You need to look at the light stimuli without blinking at the monitor, and the program already records the received impulses in the form of a graph.
- Optical coherence tomography of the ear - needed for detailed images. retina, studying its structures, detecting pathologies.
- Magnetic resonance imaging is a painless test that provides high-resolution images of the brain, eye sockets, and inner ear.
- Echo-EG is an echoencephalography procedure, a painless ultrasound examination of brain structures within fifteen minutes. The child will be asked to lie down, and small sensors will be installed on the scalp, after lubricating it with gel.
- CT - Computed tomography is needed to diagnose brain diseases such as tumors or head injuries. Unlike MRI, CT is based on x-rays, so there are certain requirements and limitations. For children of preschool age, this procedure is carried out in medicated sleep, since they cannot lie still for a long time.
You should not hesitate to diagnose nystagmus, because as the child grows, visual acuity decreases, and this happens especially quickly in young children.
Other methods for studying visual acuity
Objective visometry
Objective visometry techniques are used in children to clarify the cause of vision loss, if malingering and aggravation are suspected.
Optokinetic nystagmus method
To conduct research, you need to use objects with a periodic structure (chessboard, lattice, etc.). The patient is shown such an object in motion, and the doctor observes the eye movements of the subject. If the patient detects the movement of an object, his eyes involuntarily make rhythmic movements from side to side (nystagmus). Visual acuity is judged by the minimum size of the object that causes nystagmus.
Study of visual evoked potentials
This technique requires special attention from the patient. During the procedure, electrical impulses are recorded from the occipital region of the brain, which arise in response to visual stimulation. The patient is shown a chessboard on which cells of different colors change places with each other at a given frequency. Their size gradually becomes smaller. Visual acuity is determined by the minimum cell size at which, in response to a change in color, an impulse is recorded on the EEG.
Preferential gaze test
This technique of selective forced vision is based on the fact that the child prefers to look at structured objects rather than at homogeneous ones. During the examination, two different objects are placed in front of the patient, one of which has a vertical striped color, and the second is uniformly gray. If the patient distinguishes objects, then he will look at the structured one. Typically, Keeler maps are used to perform this method of objective visometry. Due to the fact that the test requires the participation of the muscles of the neck, head and eyes, a negative result may be associated not only with a disorder of the primary sensory system, but also with a violation of oculomotor function.
Treatment of congenital nystagmus in children
Until recently, getting rid of congenital nystagmus was considered difficult to achieve. But modern developments in the field of eye microsurgery have made it possible to successfully solve this problem.
Since this is still a consequence of another disease, a system for treating nystagmus in children was created that can “block” involuntary twitching of the eyeballs and increase visual acuity.
“Blocking” of nystagmus occurs through surgery. This technique has proven to be effective in 75% of cases!
But to treat congenital nystagmus, surgery alone is not enough: you need to improve visual acuity, help the child see the world without twitching or hesitation. This is where therapeutic treatment comes to the rescue, which allows you to increase the child’s visual acuity to almost normal levels. This alternative technique has already proven itself, showing sustainable results. The main thing is to diagnose the disease in time and begin modern comprehensive treatment as soon as possible, which includes surgery, therapeutic treatment and correction with glasses.
Surgical treatment of horizontal nystagmus
Why is it better to start treatment for nystagmus with surgical intervention? Yes, because surgery is the only way to “block” oscillatory eye movements.
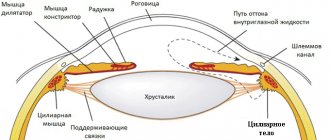
Traditional surgical interventions for the treatment of horizontal nystagmus have always involved procedures that require weakening or strengthening of the extraocular muscles to reduce the frequency of ocular oscillations. But these operations were not always successful in cases of congenital nystagmus in children.
A technique was needed that would help children specifically, and modern technologies of the 21st century contributed to its successful development. “Non-contact” technologies introduced in the last decade (high-frequency radio wave surgery) have allowed surgeons to minimize the level of trauma during surgery (preserve the integrity of blood vessels, nerve bundles, and intraocular tissues). This is a huge achievement!
Today, the latest, safest and most accurate developments are used to treat nystagmus - mathematical modeling of surgery (STRABO) and high-frequency radio wave surgery.
They help cure different types of nystagmus, reducing the frequency of oscillatory movements with a straight gaze position. Thanks to these developments, scalpels and scissors are no longer used during the operation, the rehabilitation period is reduced, and mathematical modeling provides the highest accuracy of calculations.
To reduce the frequency of eye vibrations and correct the unnatural position of the head, as well as restore the visual functions of diseased eyes, a variety of unique operations are performed using new techniques, the choice of which is determined by the type and cause of nystagmus in a particular patient.
In 75% of cases, it is possible to block nystagmus in one operation.
The goal of surgery for nystagmus is to block oscillatory eye movements during direct gaze. But at the same time, it is important to maintain the entire range of movements of the eyeball in different directions.
There are many types of operations used for nystagmus. One of them is faden - operations (the oculomotor muscles are not transplanted, not shortened, but are, as it were, “sutured” with a special suture to the sclera of the eye so that it “fits”).
Separately, it is worth noting that nystagmus cannot be eliminated using conventional, traditional methods of eye surgery. The special qualifications of an ophthalmic surgeon are very important - he must be able to work with nystagmus. To do this, the doctor must undergo special training in surgery for this particular pathology.
Nowadays, in the treatment of nystagmus, a low-traumatic method of high-frequency radio wave surgery is used, which allows the eye tissues to heal quickly; after the intervention, the child can be taken out of the hospital the next day.
Such operations are completely safe for a small child and very effective. The surgical approach is at the forefront, but it is not the only treatment method. To achieve a lasting result and improve visual acuity, a complex intervention combining surgery and therapeutic treatment is necessary. Only then is it possible to restore binocular and stereoscopic, three-dimensional vision.
↑ Physiological forms of nystagmus and their disorders
Optokinetic nystagmus (OKN)
A physiological reaction to objects moving in front of the eyes. The slow phase of nystagmus is directed towards moving objects. It is most easily detected with an unrestricted field of vision, but due to the fact that such a clinical examination is difficult to provide, older children and adults are asked to look at the optokinetic drum or mite. A difficult problem is creating interest in a young child in conducting research. To suppress OKN, the subject’s gaze is transferred to a stationary object.
There are pathological forms of OKN.
- Very low vision. The results of the OKN study are used to quantify visual acuity, although a reliable technical basis for this study does not yet exist.
- A disorder of the generation of saccadic movements (saccades) - oculomotor apraxia (impairment of purposeful movements) causes an OKN disorder with deviation of the eyes towards moving objects. In this case, the fast phase of nystagmus is either absent or pathologically altered (see below).
- Intracranial injuries. The pathology of OKN sometimes manifests itself in acute vestibular and cerebellar disorders, diseases of the occipital or occipital-parietal region.
- Congenital idiopathic or sensory nystagmus.
Monocular asymmetry of OKN
Children in the first 6 months of life, especially newborns, with monocular vision have pronounced asymmetry of OKN. The nasotemporal OKN is mainly unstable, while the temporonasal OKN is almost unchanged. The asymmetry decreases after 6 months of age, remaining at high speeds of object movement. With early-onset visual impairments, especially binocular ones, the asymmetry of the OKN not only remains, but can become permanent (Fig. 27.5).
Vestibulo-oculomotor reflex (VGR) and vestibular nystagmus
Movements of the eyeball that occur in the light or in the dark in response to head rotation and are caused by irritation of the semicircular canals of the labyrinth. The physiological meaning of this reaction is to maintain a stable position of the eyes, despite the movement of the head and body. Acute VGR disorder leads to the appearance of oscillopsia with every movement and is accompanied by decreased vision due to the inability to fix a visual image during movements of the head and body. Even traveling in a car can be extremely unpleasant for such a patient.
In laboratory conditions, VGR is studied using a rotation test on a special chair or by rotating a small child on outstretched arms. In the light, the responses are a combination of optokinetic II vestibular components, and in the dark the response is only of vestibular origin. After the cessation of rotation, single residual inetagmoid oscillations may remain.
Pathological changes in VGR are observed in the following cases.
- Diseases of the cerebellum cause a large amplitude of oscillation of the eyeball in response to movements. The disappearance of the fast phase is observed in cases of saccade generation disorder (see below). In children, especially young children, VGR pathology occurs with sensory disorders or congenital idiopathic nystagmus. Prolonged residual optokinetic nystagmus is observed in blind children and in diseases of the cerebellum.
- When the head moves, vibrations of the eyeball of equal magnitude and directed in the opposite direction occur. Therefore, suppression of VGR is necessary for synchronous movements of the head and eyes. It is believed that a similar mechanism relates to tracking eye movements and its pathological forms are found in many diseases. especially with cerebellar pathology. This condition can be artificially induced by forcing the child to look at an object that rotates with his head. An example is a button stuck into a wooden spatula to catch the tongue that a child holds in his teeth. In a healthy child, when looking at the button, nystagmus does not appear, but if there is pathological suppression of VGR, nystagmus occurs.
- Acute damage to the vestibular apparatus and its central part provokes the appearance of mixed nystagmus, which has a pronounced torsion component. In peripheral disorders, the horizontal slow phase is directed towards the localization of the damage.
With pathological VGR, the patient is bothered by a feeling of rotation, dizziness, and oscillopenia. As a rule, complaints are transient. Bilateral disorders are more severe, and recovery takes a long time. Installation nystagmus
Jerky, small-sweeping nystagmus is observed in many people with extreme gaze abduction. This phenomenon is regarded as a physiological reaction that is not accompanied by neurological symptoms or disorders of eyeball movements.
Voluntary nystagmus
Approximately 5% of people are capable of voluntary reproduction of nystagmus, and this phenomenon is considered physiological. Typically, such nystagmus is characterized by a high frequency, small amplitude and has a horizontal direction (it is much more difficult to reproduce vertical and rotatory nystagmus, and the torsional form of voluntary nystagmus is unknown). In most cases, voluntary nystagmus occurs against the background of convergence and constriction of the pupil, often accompanied by facial tics and grimaces. Normally, voluntary nystagmus cannot be maintained for more than a few seconds. Among other forms of voluntary nystagmus, the most impressive is the pendulum-shaped form with two fast phases.
Therapeutic treatment of nystagmus
After surgery, a course of therapeutic treatment of nystagmus is necessary, which will help improve visual acuity and obtain clear fixation of objects with the eyes. The course of therapeutic treatment is always strictly individual and depends on the child’s personal anatomical parameters.
In the treatment of nystagmus (as well as progressive myopia, diseases of the retina or optic nerve), for example, a physiotherapeutic procedure such as electrophoresis is used. This painless method is well tolerated even by very young children, because the medicine is not injected with a syringe, but penetrates through the intact skin of the eyelid directly into the eye using current. Cotton wool moistened with a medicinal preparation is placed on closed eyelids, and a special pad is placed on top of which a small electrode is attached. The procedure lasts from ten to twenty minutes, a total of 10 or 15 sessions are needed.
Nystagmus is often combined with strabismus. To restore the primary fusion of images obtained from both eyes into a single picture in the head, the “Synoptophore” device is used. By the way, “Synoptophore” is credited with improving vision, eliminating strabismus itself, and many other effects that have nothing to do with the capabilities of this device. The device simply does not have these functions, so do not buy into promises to cure all vision problems with this device. He has a very narrow specialization - restoration of primary fusion. This is a fairly old technique; which must be used for a very long time to achieve at least an average result.
Now a more effective technology has been developed that allows you to restore vision with both eyes even in the most advanced cases - these are stroboscopic, or oscillating, “glasses”. Exercises with this device very quickly lead to positive results. Within 10-15 days, the child’s visual acuity already increases significantly.
Conservative treatment of nystagmus can also include vision correction when nystagmus is combined with farsightedness, myopia or astigmatism - using glasses or contact lenses.
As for the prevention of the disease, for congenital nystagmus there are no life-saving measures other than promptly consulting a doctor.
Eye test video
In infants, to test visual acuity, bright contrasting balls or other objects of a certain size are used, which are shown from a given distance. For older children, you can already use tables with drawings (optotypes) of animals, airplanes, etc., which were developed by Aleynikova and Orlova.
Determination of visual acuity is often carried out without optical correction, then with it. In this case, two indicators are determined: relative and absolute visual acuity. The first value is not constant and may depend on external factors (fatigue of the body, lighting in the room), so it is often completely ignored.