Myopathy of the eye, what is it?
Many people are concerned about eye myopathy, what it is and how to treat it.
This pathology has several varieties, these include oculo-pharyngeal myopathy and ocular myopathy. The first differs in that in addition to the symptoms affecting vision, those that injure the muscle tissue located in the pharynx are added. It should be noted that oculo-pharyngeal myopathy usually occurs after 40 years. Both types contribute to the development of benign myasthenia gravis.
Myopathy is characterized by a lack of effect on the spinal cord and peripheral nervous system. The main symptoms can be considered atrophy of muscle tissue and its primary degeneration, which is expressed in the form of changes in caliber, color and shape.
Phenomena such as vacuolization and muscle proliferation at the cellular level may occur. Lipomatosis (the appearance of fat and connective tissue between muscle fibers) is also noted.
No treatment for myopia
Such a visual impairment as myopia requires immediate treatment: it does not remind you of itself with unbearable pain, does not force you to forget everything to run to the pharmacy for medicine, but, nevertheless, it often surely and steadily leads to partial or complete loss of vision. We can postpone treatment indefinitely, resorting only to purchasing correction products that increase by one diopter every year. Hoping for modern laser surgery, many of those who are familiar with myopia first-hand think only about prompt resolution of the problem in the distant future, without caring about prevention and special treatment here and now.
The variety of spectacle optics and contact lenses allows you to choose the product that will make it possible to completely forget that you have vision problems. This is an aggravating factor in the development of myopia to a high degree. Only a combination of preventive measures will prevent the disease from developing rapidly, and they cannot be neglected.
How does the disease manifest itself?
In primary forms, the first signs of the disease usually appear in childhood or adolescence. A typical symptom that may indicate the disease in a child is muscle weakness. This feature is characteristic of all forms. Weakness is usually symmetrical, meaning it occurs in symmetrical muscles. In the initial stages, weakness may be insignificant, but gradually its severity increases.
As the disease progresses, the quality of life decreases: even habitual loads become difficult and difficult for the patient to perform. Difficulties appear when walking or climbing stairs. Due to muscle dystrophy, posture may be disrupted and curvature of the spine may appear, for example, lumbar lordosis, kyphosis, scoliosis, which progress over time. In this case, the patient’s head and stomach protrude forward, the shoulders drop, and wing-shaped shoulder blades are formed3.
When the proximal muscles, located closer to the center of the body, are affected, difficulties arise with rising from a chair, getting out of the bath, climbing stairs, combing hair, or shaving. A “duck” gait is observed - the patient moves, swaying to the sides. With weakness in the hands, a person has difficulties performing highly differentiated work (writing, playing musical instruments, turning, etc.). Weakness of the feet is manifested by the formation of a hollow foot, a flopping gait. In some forms, for example, Nemalin myopathy, sometimes with Pompe disease, weakness of the respiratory muscles appears, which leads to an increased risk of pulmonary infections. In addition, the oxygen supply deteriorates, which can cause damage to the brain, heart, and other organs4.
Along with muscle weakness, tendon reflexes decrease, muscle spasms or contractions occur, and joint mobility is limited—contracture3.
Treatment of 2nd degree myopia
Treatment of grade 2 myopia is impossible without regular visits to an ophthalmologist.
After diagnosis, the doctor will select an individual method of vision correction:
- Glasses. Most often, glasses are used for this, and in some cases contact lenses. It is better if the glasses are bifocal, that is, with combined lenses. The upper part is allocated for stronger lenses, which allow you to view objects located in the distance. The lower half is designed for weaker lenses that allow reading and writing.
- Laser correction. Laser correction can help, which is carried out in cases of non-progressive myopia and after the patient reaches 18 years of age. Laser correction is aimed at changing the shape of the cornea, due to which the focus is projected to the right place, namely the retina.
- Other methods. As for therapeutic methods, such as drug treatment, eye exercises, physiotherapy, they are all aimed at maintaining vision at the same level. These methods are not able to save a person from moderate myopia; they can only prevent further progression of the disease.
- Vitamins. Doctors often prescribe vitamins B and C, as well as nootropic drugs such as Panotogam and Piracetam. To relieve accommodation spasms, mydriatics are used - Mezaton and Irifrin.
- Surgical treatment. If during routine examinations it is revealed that a person’s vision decreases by 1 or more diopters per year, then this indicates a progressive form of the disease. When conservative methods are unable to stop this process, it is necessary to resort to surgical treatment. Most often, in this case, the method of scleroplasty is used, which is designed to strengthen the sclera of the eye and stop the progression of the disease.
Symptoms
The progression of the disease occurs over a fairly long period of time. Symptoms gradually increase. An abrupt course of the disease is not typical.
The overall picture looks like this:
- muscle weakness and pain;
- excessive fatigue of the patient;
- “ache” in the body;
- decreased mobility in joints (in some cases, on the contrary, increased mobility);
- decreased muscle strength.
In addition to general symptoms, there are certain signs for each specific case.
Duchenne dystrophy
This disease is the most common and most severe form of the disease, and also has the highest mortality rates. It includes the following symptoms:
- enlargement of the calf muscles due to the growth of adipose tissue;
- difficulties with lifting the patient independently;
- complete degeneration of the whole body gradually develops;
- joint deformation;
- dystrophy of the cardiac and respiratory muscles (which can lead to death).
Any inflammatory process in this form of the disease can be fatal.
Erb Roth dystrophy
This type of disease mainly develops in children. Moreover, it is possible that it develops in an infant, an older child or a teenager.
If we are talking about dystrophy in an infant, such a disorder is clearly congenital (hereditary) in nature, since a newborn can acquire this disease only by inheritance or as a result of a genetic failure.
For children from 3 to 5 years old, such a disease can also be considered congenital.
Well, for older adults (teenagers), the name juvenile (youthful) dystrophy is applicable. Moreover, youthful does not mean that a girl cannot get sick; the female sex is susceptible to this disease in the same way as the male sex.
The main symptoms characteristic of the disease are as follows:
- hip dystrophy;
- back atrophy and gradual curvature of the spine;
- formation of a “duck” gait and a “wasp” waist;
- weakening of the muscles around the mouth.
It is not worth talking about the instantaneous nature of progression, except in the very early stages, when very young children suffer.
Becker's dystrophy
This type of disease has the following symptoms:
- increased fatigue of the lower extremities;
- change in the appearance of the legs (vegetative manifestations);
- decreased energy metabolism;
- atrophy of the pelvic muscles.
Landouzy-Dejerine disease
This disease largely affects the muscles of the face and, accordingly, the symptoms are corresponding, including:
- visual impairment (myopia, farsightedness of several diopters);
- dysfunction of the eye muscle;
- uncontrolled muscle fasciculation (involuntary contraction);
- weak response of the paralabial muscles (reminiscent of the ability to move the lips, with swelling).
There is also a mild form of this disease - ocular myopathy, which can cause minor complications in the eyes, causing minor deviations. So, a person may focus his vision worse, he experiences problems with closing and opening them. As a rule, an illness of such a mild degree poses no threat to the patient if treated.
Types of myopia
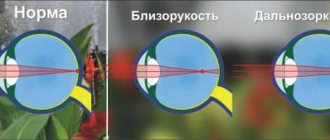
According to severity, experts distinguish three main types of myopia:
- weak - less than 3 diopters;
- average - from 3 to 6 diopters;
- high - over 6 diopters.
According to the clinical course, there are two types of myopia: non-progressive and progressive.
Non-progressive myopia is a problem that is usually solved with glasses or contact lenses. In this case, additional treatment will not be needed.
Progressive myopia is a more serious disease, the sign of which is considered to be a deterioration of vision by at least one diopter per year. It is often encountered by schoolchildren whose visual load increases significantly. In some cases, such myopia may stop progressing when the body stops growing. In other cases, vision continues to deteriorate, resulting in blindness and disability.
Progressive myopia imposes many restrictions on a person. Wrestling and boxing, long and high jumps, as well as many other sports are contraindicated for him. Lifting heavy objects is also undesirable, and this can already affect everyday life.
The higher the degree of myopia, the greater the likelihood of various complications. Disproportion of the eyeball leads to stretching of its membranes, they become thinner, while the vessels passing through them are stretched, and because of this, blood flow worsens and problems with metabolism arise. Tears may occur in thinned areas - they are caused not only by heavy lifting or increased visual stress, but also by psycho-emotional stress.
Without timely correction, vision may continue to deteriorate.
It only gets worse from there. The retina detaches, and the detachment progresses: first, part of the peripheral vision disappears, then there is a feeling of a “black curtain” through which nothing can be seen, and it increases until the person loses vision completely.
As a rule, this is not accompanied by pain, so a myopic person cannot always respond in a timely manner to a sharp deterioration in vision.
Classification
Specialists in the field of neurology have developed several classifications of myopathies. The most popular among clinicians is the etiopathogenetic principle of separation, according to which hereditary, inflammatory, metabolic, membrane, paraneoplastic and toxic myopathies are distinguished. Among hereditary myopathies, 3 types are most common: juvenile/adolescent form of Erb, pseudohypertrophic form of Duchenne and humeroscapulofacial form. Less common are scapuloperoneal, oculopharyngeal, distal and other forms. A separate group includes congenital myopathies: central core disease, nemaline and myotubular myopathy, disproportion of myofibril types.
Inflammatory myopathies are classified as infectious - arising as a result of infectious-inflammatory damage to muscle tissue during various infectious processes: bacterial (streptococcal infection), viral (enteroviruses, influenza, rubella, HIV), parasitic (trichinosis, toxoplasmosis) and idiopathic - dermatomyositis, inclusion body myositis , polymyositis, myopathies due to collagenosis.
Metabolic myopathies are divided into those associated with disorders of lipid metabolism in muscles (acetyl-CoA dehydrogenase deficiency, carnitine deficiency), glycogen metabolism (Andersen disease, Pompe disease, glycogenosis type III, McArdle disease, phosphorylase b kinase deficiency, phosphoglyceromutase deficiency), purine metabolism (MADA enzyme deficiency) and mitochondrial myopathies (reductase, ATP, cytochrome b, b1 deficiency).
Doctors distinguish several types of myotonic syndrome. Each type of disorder has its own characteristics of occurrence and requires specific therapy. In medicine they talk about the following types of pathology:
- dystrophic myotonia, characterized by concomitant damage to the endocrine and autonomic nervous systems, as well as visual impairment;
- congenital paramyotonia is a rare type of disease accompanied by paresis and paralysis;
- Thomson's myotonia, which is hereditary and manifests symptoms between the ages of 6 and 12 years;
- Becker's myotonia is the most common. Signs of the disease develop after 4 years of age;
- Schwartz-Jampel syndrome is accompanied by skeletal abnormalities and severe mental retardation.
The specific type of syndrome in a child is determined by the attending physician based on a clinical examination.
Myopathy - symptoms, treatment, causes of the disease, first signs
Myopathy is a disease that occurs as a result of disturbances in the metabolism and structure of muscle tissue, resulting in a decrease in the strength of the affected muscles, as well as a limitation of motor activity.
Myopathies belong to a group of neuromuscular diseases, which are characterized by dystrophic damage to muscle tissue with atrophy of individual fibers (myofibrils) in some places.
In addition, atrophied myofibrils are replaced by connective or adipose tissue.
This leads to the loss of the muscles’ ability to contract, which causes the appearance of muscle weakness in the clinic of the disease, as well as limitation of motor activity.
There are two main forms of the disease:
- Primary myopathies, which are often hereditary. In turn, they are divided into the following types:
- congenital myopathies that develop in infancy;
- early childhood myopathies that develop at the age of 5-10 years;
- juvenile myopathies that develop in adolescence.
- Secondary myopathies occurring against the background of other diseases.
For example, against the background of endocrine disorders (Cushing's disease, hyperaldosteronism, hyperparathyroidism, hypo- and hyperthyroidism), chronic intoxication (alcoholism, drug addiction, work in enterprises with occupational hazards), severe chronic diseases (chronic renal failure, chronic liver failure, chronic obstructive pulmonary disease, heart failure), as well as tumor processes.
Primary forms of myopathy are much more common than secondary ones. Therefore, it is extremely important when planning a pregnancy to consult a geneticist in order to identify the risk of developing this pathology in the unborn child.
Based on which part of the body muscle weakness is more pronounced, the following types of myopathy are distinguished:
- proximal - the pathological process is located in those parts of the limbs that are located as close as possible to the body (for example, in the case of the arms, these are the shoulders);
- distal - the muscles of the limbs are affected, which are at the maximum distance from the body (for example, in the case of the legs - the calf muscles);
- mixed - has symptoms of proximal and distal forms of the disease.
Primary myopathies have a poor prognosis. Especially if the first symptoms appeared in early childhood. The involvement of the heart muscle and respiratory muscles in the process is also important.
In this case, the prognosis of the disease worsens.
The most favorable outcome is observed with secondary myopathies, since in this case it is easier to achieve success in treating the underlying disease that caused the development of myopathy.
Symptoms
nervzdorov.ru
Myopathy begins with the appearance of slight muscle weakness in the limbs. Fatigue sets in faster when walking or other physical activity than before the onset of the disease.
It becomes more difficult for such people to cover long distances, so they often have to take short rest breaks in order to continue their journey with renewed vigor.
Next, muscle atrophy joins the growing weakness, resulting in deformities of the limbs. As a rule, atrophic changes are observed in the proximal (which are closer to the body) parts of the arms and legs.
Because of this, the distal limbs may appear hypertrophied. This phenomenon is called “pseudohypertrophy”. As muscle weakness progresses, it becomes difficult to jump, run, or walk up stairs.
The characteristic appearance of a patient with myopathy gradually develops: wing-shaped shoulder blades, drooping shoulders, a protruding abdomen and increased lumbar lordosis, due to which the so-called “wasp” waist is formed. In addition, a “duck” gait is observed (movement is accompanied by swaying to the sides).
In addition, myopathies may be accompanied by damage to the facial muscles. You can suspect the involvement of facial muscles in the pathological process when a person cannot stretch out his lips, puff out his cheeks, frown or smile.
Damage to the orbicularis oris muscle is accompanied by the development of dysarthria due to difficulty pronouncing vowel sounds.
Dysarthria itself refers to a speech disorder, which is expressed in difficulty pronouncing certain words, individual sounds, syllables, or in their distorted pronunciation.
Damage to the respiratory muscles is accompanied by impaired ventilation of the lungs, which leads to congestive pneumonia. This form of pneumonia is one of the most severe, difficult to treat and quickly leads to the development of respiratory failure.
There is also evidence of the possibility of damage to the heart muscle. In this case, cardiomyopathy develops, which leads to the development of heart failure.
Medicines
smartmoney.today
The goal of treatment is to reduce muscle tissue atrophy. Anabolic hormones (retabolil, nerobol) provide significant assistance in this regard. Their action is expressed in stimulating the growth of muscle cells, which is necessary to maintain muscle mass.
Due to this, there is an increase in strength, performance and endurance. However, there is a downside to taking these drugs. With long-term use, accompanying effects may occur in the form of baldness, increased hair growth on the face and body.
In addition, there is such a concept as masculinization, which refers to the appearance of secondary male sexual characteristics in women.
In this case, the physique changes to a male type, the voice becomes rougher, the menstrual cycle is disrupted, the elasticity of the skin changes, and acne appears.
Anticholinesterase drugs include drugs such as prozerin and neuromidin. Preference is given to neuromidin, since its spectrum of action is much wider than proserin. Also, with long-term use of proserin, various unpleasant side effects are observed, so in most cases the drug is prescribed in short courses.
In turn, neuromidin has a good stimulating effect on neuromuscular transmission and also increases muscle contractile activity. In addition, neuromidin has sedative and analgesic (relieves pain) effects.
Vitamin preparations include vitamins E, B and C, as well as nicotinic acid.
Folk remedies
medaboutme.ru
Since in most cases the cause of myopathy is a hereditary pathology, it is impossible to alleviate your condition without medications, but by independently following certain measures you can improve your general condition.
For example, nutrition plays a big role, so it is important to follow some recommendations. Firstly, you should add more fresh vegetables and fruits, dairy products, eggs, honey, nuts, and cereals (especially oatmeal and buckwheat) to your diet. Secondly, it is important to give up coffee, alcohol, potatoes, cabbage, and spicy foods.
In order to prevent accelerated muscle atrophy, it is necessary to constantly perform therapeutic exercises. But you should also remember that the condition of the muscles in myopathy is far from the condition of the muscles of a healthy person. Accordingly, the load should be minimal so as not to cause overvoltage. Swimming pool exercises are perfect for this purpose.
Also, do not forget about the importance of breathing exercises. A common occurrence in myopathy is damage to the respiratory muscles, resulting in impaired ventilation of the lungs, which subsequently leads to an inflammatory process (the development of pneumonia). Breathing exercises are aimed at improving gas exchange in the lungs.
It is not recommended to develop a list of exercises on your own; it is better to contact a specialist for an individual selection of the necessary exercises. After training at a medical institution, you can continue gymnastics at home.
The information is for reference only and is not a guide to action. Do not self-medicate. At the first symptoms of the disease, consult a doctor.
Source: //yellmed.ru/bolezni/miopatiya
Horner's syndrome - what is it?
Horner's syndrome is a pathological condition associated with damage to the cervical region of the SNS (sympathetic nervous system) and is manifested by the appearance of:
- ptosis (pathological drooping of the upper eyelid);
- miosis (constriction of the pupil);
- anhidrosis (lack of sweating on the affected side).
Other names are also used to define the pathology - Claude Bernard-Horner syndrome, oculosympathetic syndrome, Horner's triad.
Horner's syndrome can be either congenital or acquired. The incidence of Bernard-Horner syndrome is approximately 1.42 cases per 100,000 births.
Prevention
There is evidence that children who spend more time outdoors have a lower risk of developing myopia. Natural sunlight is also beneficial. It saturates with vitamin D, which affects sleep, mood, energy and has a positive effect on a person’s general condition.
You can’t stay in the sun for a long time, it negatively affects your vision. If you have to spend a long time in a sunny place, wear sunglasses or a wide-brimmed hat.
We recommend reading: Prevention of myopia
Prevention should begin by limiting the daily use of computers, phones and other devices that emit blue light and cause eye strain. While working with them, increase the lighting to make it easier for your eyes to see small details. Every 45 minutes, take 10-minute breaks, during which you perform eye exercises.
Inflammation is the root cause of many diseases, including those that negatively affect eye health. Many pathologies cannot be prevented, but the risk of their occurrence can be reduced. For example, quit smoking and take large doses of alcohol.
Concomitant pathologies
In addition, ocular myopathy often occurs with concomitant diseases, such as:
- glycogenosis;
- myoglobinuria;
- amyloidosis (primary);
- polymyositis.
In most cases, the course of the pathological process of dysfunction of the eye muscles is not indicated by any symptoms at all, but only until vision begins to rapidly deteriorate. The approach to such patients must be individual. A biopsy may help to detect this disease earlier.
Myopathy can be malignant, in which case its consequences and complications will be much more serious. The catalyst for the progression of the disease are bad habits, such as alcoholism and smoking.
Myopathy in children - causes of the disease
There is an assumption that myopathy in children is provoked by a surplus of creatine phosphokinase. This leads to dysfunction of muscle fibers in relation to their retention of a substance called “keratin”. This is why myopathy begins - a weakening of muscle tone, up to the complete necrosis of muscle fibers.
There is a theory, the meaning of which is that individual structured muscle units have unique “membranes” that release a much-needed element. In a word, everything happens because metabolic metabolism is disrupted.
Description
Myopathy is a disease that occurs as a result of disturbances in the metabolism and structure of muscle tissue, resulting in a decrease in the strength of the affected muscles, as well as a limitation of motor activity.
Myopathies belong to a group of neuromuscular diseases, which are characterized by dystrophic damage to muscle tissue with atrophy of individual fibers (myofibrils) in some places. In addition, atrophied myofibrils are replaced by connective or adipose tissue. This leads to the loss of the muscles’ ability to contract, which causes the appearance of muscle weakness in the clinic of the disease, as well as limitation of motor activity.
There are two main forms of the disease:
- Primary myopathies, which are often hereditary. In turn, they are divided into the following types:
- congenital myopathies that develop in infancy;
- early childhood myopathies that develop at the age of 5-10 years;
- juvenile myopathies that develop in adolescence.
- Secondary myopathies occurring against the background of other diseases.
For example, against the background of endocrine disorders (Cushing's disease, hyperaldosteronism, hyperparathyroidism, hypo- and hyperthyroidism), chronic intoxication (alcoholism, drug addiction, work in enterprises with occupational hazards), severe chronic diseases (chronic renal failure, chronic liver failure, chronic obstructive pulmonary disease, heart failure), as well as tumor processes.
Primary forms of myopathy are much more common than secondary ones
Therefore, it is extremely important to consult a geneticist when planning a pregnancy in order to identify the risk of developing this pathology in the unborn child.
Based on which part of the body muscle weakness is more pronounced, the following types of myopathy are distinguished:
- proximal - the pathological process is located in those parts of the limbs that are located as close as possible to the body (for example, in the case of the arms, these are the shoulders);
- distal - the muscles of the limbs are affected, which are at the maximum distance from the body (for example, in the case of the legs - the calf muscles);
- mixed - has symptoms of proximal and distal forms of the disease.
Primary myopathies have a poor prognosis. Especially if the first symptoms appeared in early childhood. The involvement of the heart muscle and respiratory muscles in the process is also important. In this case, the prognosis of the disease worsens. The most favorable outcome is observed with secondary myopathies, since in this case it is easier to achieve success in treating the underlying disease that caused the development of myopathy.
Classification of the disease
According to the severity of the disease, myopia is usually divided into:
- Weak degree (up to 3.0 D);
- Middle steppe (up to 6.0 D);
- High degree (over 6.0 D).
Mild myopia does not cause any particular discomfort to the patient and does not require constant wearing of optical lenses. Moderate myopia requires certain treatment and constant wearing of corrective glasses. A severe form of the disease often leads to the need for surgical treatment.
In addition to the degree of myopia, the disease varies in its course. This is how it happens:
- Progressive;
- Not progressive.
With a non-progressive form of myopia, the pathology can be easily corrected and treated, manifested by decreased distance vision. In the progressive form of the disease, which is also manifested by decreased distance vision, vision decreases so rapidly that it requires an increase in optical correction by 1 D almost every 12 months. Various complications often arise against its background, which sometimes require surgical intervention. Typically, a similar form of the disease is observed with a high degree of myopia.
There are often cases when myopia is combined with astigmatism. This refractive error is caused by a change in the shape of the cornea, focusing parallel rays of light at several points simultaneously. During an ophthalmological examination, astigmatism is not always detected. Suspicions of its presence arise due to the impossibility of vision correction even with long-term selection of optical lenses. Indeed, in this case, corrective lenses should be aimed not only at increasing visual acuity, but also at eliminating astigmatism.
What is eye myopathy and how to treat it
Eye myopathy is a disease in which there is a pathological disorder of visibility that occurs due to changes in the refractive functions of the visual apparatus.
If proper measures are not taken, the disease process progresses intensively and can cause severe weakening of vision, even blindness.
At the first symptoms, it is important to consult a doctor for help
The disease can appear on one visual organ, but cases with myopathy in both eyes are often observed.
Kinds
Myopathy most often occurs due to a genetic predisposition. Pathology happens:
- ocular – accompanied by degenerative non-muscular disorders;
- oculopharyngeal - here, in addition to a decrease in visual function, there is a violation of the muscle tissue located in the throat.
Myopathy can develop at any age. But in most cases it appears after 40 years.
Reasons for education
Predisposing factors for the formation of myopathy are changes in the functioning of the accommodative muscles of the eyes, as well as the shape of their chambers.
Ophthalmic pathology develops due to dysfunction of muscle tissue, as a result of which they stop retaining keratin. After some time, their tone decreases, so muscle death is possible.
In addition, other factors can cause the appearance of ocular myopathy:
- heredity;
- severe eye strain;
- incorrect treatment of ophthalmic diseases;
- lack of vitamins and minerals in the patient’s body, this leads to changes in metabolism;
- defects in the structure of the organ of vision.
Timely diagnosed and treated myopathy of the visual organ will lead to a favorable result.
Stages, symptoms
Often, eye myopathy occurs without any noticeable symptoms, which greatly complicates the diagnosis of the pathology. The mild stage of an ophthalmological disease is classified by changes in the muscles of the eye, this provokes a decrease in visual function and causes difficulties in their mobility (closing, opening the eyes).
In some situations, myopia is noted, which is divided into 3 stages:
- weak with 3 dioptres;
- average - from 3-6 diopters;
- intense - over 6 diopters.
This pathological visual disorder has no tangible signs. Doctors studying eye myopathy only understand that the disease appears due to changes in metabolic processes occurring in the body.
No other assumptions have been made. Despite the fact that the disease is asymptomatic, its main symptom is a severe decrease in vision.
If such a condition occurs or one of your relatives has such a diagnosis, the risk of developing myopathy increases.
Concomitant diseases
Sometimes eye myopathy appears with associated pathologies:
- polymyositis - systemic inflammation of muscles (often striated muscle tissue);
- myoglobinuria - a syndrome characterized by the myoglobin pigment in urine; occurs when muscle protein breaks down;
- primary amyloidosis is a metabolic disorder accompanied by the appearance and deposition of amyloid in the muscles;
- Glycogenosis is the name given to syndromes caused by genetic defects in enzymes involved in the breakdown of glycogen.
Therapeutic measures in the fight against visual myopathy must be taken individually. Early detection of the disease is facilitated by a biopsy. The disease may have a malignant nature, then the process will worsen, and the consequences will be much more serious. Bad habits become the culprit for the progression of myopathy.
Disease prevention
There are several preventive recommendations for myopathy:
First of all, it is important to eliminate bad habits (smoking, alcohol); a certain dietary food (various cereals, salads with the addition of celery, turnips, milk, liver are shown; remove spicy, fatty, salty foods from the diet); Regular sports activities can normalize the patient’s condition; get plenty of rest and don’t strain your eyes for too long; When working at a computer, the light should be consistently illuminated (for example, darkness, as well as bright light, has an adverse effect on vision); When exposed to intense sunlight, use protective glasses to avoid burning the cornea; The distance between the book and the eyes should be at least 30 cm, and every hour you should take a break, do some exercises, and blink a little.
If myopathy is detected in time, the outcome will be favorable. To do this, it is necessary to undergo examinations by an ophthalmologist from early childhood. When establishing myopia, correctly prescribed treatment is of great importance.
Causes
The main factors influencing the development of the disease are physiological. They manifest themselves in the improper functioning of certain eye muscles and the shape of their chambers. Dysfunction occurs and they no longer retain the keratin they need. Gradually, their tone weakens, the tissues die.
The appearance of the disease is also influenced by factors such as:
- genetics;
- severe strain on the eyes;
- lack of vitamins leading to metabolic disorders;
- ineffective treatment of eye diseases;
- congenital pathologies of the visual organs.
Varieties
With a disease such as myopathy, the muscle structures of the shoulder girdle and pelvic girdle are predominantly affected. But other muscles can also be affected, so depending on the severity of the symptoms, several forms of this disease are distinguished.
The most common form is Duchenne myopathy. This form of pathology is otherwise called pseudohypertrophic, since it is characterized by an increase in muscle mass due to the accumulation of fat, which causes the muscles to become large but weak. Duchenne myopathy is the most malignant form of pathology - it is characterized by a rapid course and severe consequences. Most patients with Duchenne atrophy become disabled and even die due to respiratory or heart failure. It must be said that Duchenne myopathy manifests itself already in the first years of life, and it mainly affects boys. In addition, the earlier it begins, the more severe the pathology.
The second form is also no less common - this is Erb's myopathy or the juvenile form of the pathology. The disease develops in men and women aged 20–30 years, and is manifested by atrophy of the muscles of the thighs and pelvic girdle. Patients develop a “duck” gait and develop atrophy of the oral muscles, which is characterized by the inability to purse their lips and whistle, which also causes problems with the pronunciation of certain sounds. Early onset of the disease leads to immobility and disability, but if the disease begins later, its course is less aggressive.
Another common form is Becker myopathy. It is considered the mildest pathology of all varieties. It begins in young people at the age of 20 and is manifested by hypertrophy of the calf muscles. There are no mental abnormalities with this form.
Becker myopathy
The next form of pathology is glenohumeral-facial. Both men and women are affected by this variant, and the disease manifests itself between the ages of 10 and 20 years. The initial symptom of the disease is weakness of the facial muscles, after which atrophy spreads to the muscles of the shoulder girdle, affecting the shoulder blades. This disease affects the muscles of the mouth and eyes, which leads to their hypertrophy. Very rarely the process reaches the pelvic girdle. The course of this type of myopathy is slow, so patients can maintain mobility and performance for a long time. The later the disease begins, the easier it is, and disability in most cases does not develop in this form.
There is also a type of disease called eye myopathy. Most often, due to damage to the eye muscles, a person develops myopia and this is the main and only symptom of this pathology. No other disorders are found in eye myopathy, so this form of the disease can be considered the mildest.
In medical practice, there are some other types of myopathies, for example, distal, filiform, mitochondrial, Oppenheim myopathy. These forms of the disease are less common and do not have pronounced manifestations, so they are often not even diagnosed.
As mentioned above, the causes of the disease lie in gene mutations, and scientists have still not been able to figure out why these mutations occur. The consensus is that myopathy develops as a result of metabolic disorders in muscle tissue.
Treatment of myopathies
As a rule, in the treatment of myopathy, palliative therapy (symptomatic treatment) is the basis, since the other option is ineffective and is currently only at the development stage.
In other words, a cure for myopathy has not yet been found.
Symptomatic therapy includes:
- taking vitamins E, B;
- anabolic steroid;
- potassium and magnesium preparations;
- anticholinesterase drugs;
- thiamine pyrophosphate;
- neostigmine;
- amino acids.
In addition to drug therapy, the following is prescribed:
- physiotherapy;
- massage;
- therapeutic exercises (therapeutic gymnastics);
- exercises in the pool.
Depending on the characteristics of the course of the disease, conservative and surgical measures are used in the treatment of myopia. Medications are prescribed for mild myopia.
To normalize focusing, glasses that fix the focus on the retina are recommended. The selection of glasses must be approached carefully, since the wrong choice can lead to unpleasant sensations - dizziness, pain in the eyes, discomfort when reading.
To normalize trophism and blood supply to intraocular tissues, restorative therapy, gymnastics for the eye muscles, and massage are recommended.
For moderate and high myopia (not myopathy), the only way to effectively get rid of the pathology is considered to be an operation to normalize the shape of the eyeball - keratotomy. The procedure involves changing the curvature of the cornea. If necessary, a lens can be implanted during the procedure.
Laser vision correction helps correct high-grade astigmatism.
Typically, laser vision correction is not performed on children under 18 years of age due to the constant growth of the body and the formation of the eye structure. Sometimes there are exceptions when minor children with high myopia undergo surgical keratotomy.
Treatment is symptomatic and ineffective. Pathogenetic treatment is being developed, many institutes in different countries are conducting research at the gene level - using both stem cells and cell cultures... but this is the medicine of the future.
Diagnostics
Photo: neurology-md.ru
The doctor may suspect the presence of myopathy even at the level of the initial examination, since such people are characterized by a corresponding appearance. Firstly, there is muscle atrophy (of the proximal limbs) and pseudohypertrophy of the distal limbs. Secondly, over time, a “duck” gait is formed. Myopathy is also characterized by drooping of the shoulders, wing-shaped lag of the shoulder blades, protrusion of the abdomen forward and increased lumbar lordosis.
Then the doctor proceeds to a neurological examination, during which a weakening of tendon reflexes and a decrease in muscle strength are detected. Unlike neuropathy, myopathy does not cause sensory impairment.
After the examination, the patient is sent to the laboratory to undergo the required list of tests. One of them is a biochemical urine test, which looks for creatinine to confirm myopathy. The presence of creatinine in the urine may indicate muscle damage, so this indicator is not without information in the diagnosis of the disease in question. Next, a biochemical blood test is performed, which evaluates the level of CPK, ALT, LDH and other enzymes.
In addition, electrophysiological research methods are used: electroneurography and electromyography. The results of electroneurography provide information about the state of the peripheral motor neuron, which is necessary if there is a suspicion of neuropathy. Electromyography is performed to directly assess the condition of muscle tissue. With myopathy, a change in muscle potentials occurs (their amplitude decreases and duration shortens).
The most informative method is a morphological study of muscle tissue. This is done using a muscle biopsy. This method, although the most informative, is rarely carried out, only in cases where previous research methods did not provide adequate information to confirm a particular diagnosis. With myopathy, the morphological picture of muscle tissue samples is as follows: randomly scattered atrophied myofibrils (contractile elements of muscle fibers), hypertrophied muscle fibers are revealed, and replacement of sections of muscle tissue with connective or fatty tissue is observed.
To assess the condition of the heart muscle, a consultation with a cardiologist is scheduled, who in turn sends the patient for an ECG and ultrasound of the heart. If pneumonia is suspected as a complication of myopathy, an X-ray of the lungs is performed.
Diagnosis and treatment
A neurologist diagnoses this disease and makes the correct diagnosis.
So, diagnostics includes:
- clinical blood test;
- biochemical blood test (to determine the level of CPK, LDH, ALT, AST);
- electroneurography;
- electromyography;
- muscle biopsy (examination of muscle tissue).
Among other things, differential diagnosis may include:
- ECG;
- Ultrasound of the heart;
- magnetic resonance imaging (MRI);
- consultation with a cardiologist and pulmonologist.
A disease such as myopathy requires careful diagnosis, since treatment of the pathology does not eliminate it and is aimed only at supporting the health of the sick person. Therefore, the earlier the diagnosis is made, the greater the likelihood of improving the patient’s quality of life.
Diagnosis of the disease is based on a blood test, taking muscle fibers for a biopsy and examining them, as well as conducting a study such as an electromyogram. In some cases, the diagnosis can only be made by molecular genetic analysis.
Disease prevention
There are several preventive recommendations for myopathy:
First of all, it is important to eliminate bad habits (smoking, alcohol); a certain dietary food (various cereals, salads with the addition of celery, turnips, milk, liver are shown; remove spicy, fatty, salty foods from the diet); Regular sports activities can normalize the patient’s condition; get plenty of rest and don’t strain your eyes for too long; When working at a computer, the light should be consistently illuminated (for example, darkness, as well as bright light, has an adverse effect on vision); When exposed to intense sunlight, use protective glasses to avoid burning the cornea; The distance between the book and the eyes should be at least 30 cm, and every hour you should take a break, do some exercises, and blink a little.
If myopathy is detected in time, the outcome will be favorable. To do this, it is necessary to undergo examinations by an ophthalmologist from early childhood. When establishing myopia, correctly prescribed treatment is of great importance.
In this article we will look at what it is - eye myopathy.
This disease is a pathological visual impairment resulting from changes in the refractive functions of the visual system. If the necessary treatment is not provided, the pathological process actively progresses and can lead to severe visual impairment, and in some cases to complete blindness.
Therefore, if visual functions are impaired, it is very important to contact a medical institution, where the appropriate diagnosis and required treatment of the disease will be carried out. The disease can occur in only one eye, but myopathy of both eyes is often diagnosed.
Diagnostic measures
It is recommended not to delay your visit to the ophthalmologist, as the risk of vision loss is high.
If a patient experiences visual impairment, it is important to immediately contact a medical facility. The doctor will conduct a survey of the patient, during which he will find out how long ago the vision problems appeared and whether similar pathological symptoms are present in close relatives. When such problems have been identified in family members, diagnosis is easy. If typical manifestations of the disease were not observed, diagnostic measures are difficult.
First of all, it is necessary to exclude pathologies of the nervous system, for example, chronic poliomyelitis, amyotrophic lateral sclerosis.
The greatest difficulty in diagnosis is represented by large groups of myopathic syndromes, which are provoked by ecogenic and endogenous pathologies. There are a large number of primary diseases of muscle tissue that are not associated with damage to the nervous system. For example, myopathy of the visual organs can develop with myoglobinuria and primary amyloidosis. To make an accurate diagnosis, the patient will need to undergo the following examinations:
- electromyography;
- blood enzyme analysis;
- muscle tissue biopsy.
Toxic myopathies
Toxic myopathies can be iatrogenic. Medicines can cause: myalgia, muscle tension (stiffness), or cramps; myotonia (delayed relaxation of skeletal muscles after voluntary contraction) - painless proximal myopathy with muscle weakness; myositis or inflammatory myopathy; focal myopathy in the area of injury (injection); hypokalemic mimopathy when administered drugs that cause hypokalemia; mitochondrial myopathy due to inhibition of mitochondrial DNA; rhabdomyolysis (acute muscle necrosis with myoglobinuria and systemic complications).
Necrotizing myopathy has been described with the use of lovastatin (an inhibitor of cholesterol synthesis), cyclosporine, aminocaproic acid, procainamide, and phencyclidine. Muscle weakness and pain develop (spontaneous and upon palpation of muscles); CPK levels increase; EMG shows a picture of myopathic changes. Intramuscular administration of the antibiotics doxine botulinum, chlorpromazine, phenythion, lidocaine and diazepam can cause local muscle necrosis and fibrous myopathy. Emetine causes progressive proximal myopathy. The same ability was found in clozapine, D-penicillamine, growth hormone, interferon-alpha-2b, vincristine.
Myalgia and muscle cramps can be caused by: angiotensin-converting factor inhibitors, anticholinesterase, beta-adrenergic agonists, calcium antagonists, corticosteroid withdrawal, cytotoxic drugs, dexamethasone, diuretics, D-penicillamine, levamisole, lithium, L-tryptophan, nifedipine, pindolol, procainamide , rifampicin, salbutamol. Drug-induced myalgia without muscle weakness usually resolves quickly after discontinuation of the drug.
Eye myopathy symptoms and treatment
To treat eye myopathy, our clinic most often prescribes medications that:
- Helps improve metabolic processes in muscles. This can be achieved through:
- "Retabolil";
- "Methylandrostenolone";
- vitamins C and E.
- Activate the circulatory system, for example, “Nikoverin” or “Trominal”.
- Normalize the processes of excitability and conductivity (Galantamine, Mestinon).
These and many other drugs can only be prescribed by a specialist based on the results of the examination.
The result of treatment for eye myopathy largely depends on the attitude of the patient himself to his problem. If it is serious, then the necessary measures will be taken on time. The main thing is to believe in your cure for strabismus and see a good doctor. After all, self-medication can lead to the opposite effect, the consequences of which will be much more difficult to correct.
Since the disease can begin almost asymptomatically, you need to pay attention to the slightest ailment. Such vigilance is not suspicious manifestations of character, but self-care
In addition, treatment carried out in the early stages has more positive results than treatment started at a later date.
Take care of yourself, be vigilant and do not miss serious disorders in your body. The cost of services, including correction of strabismus, can be found in the “Prices” section.
Factors associated with the rapid development of myopia
- Hereditary predisposition;
- birth injuries;
- head injuries;
- high pressure;
- lack of vitamins and microelements;
- weakening of the muscles of the visual organ, overstrain;
- other visual defects (astigmatism, strabismus);
- causes caused by eye strain;
- lack of appropriate treatment when myopia is detected;
- incorrect selection of correction means;
- hormonal disorders and infectious diseases;
- age.
Heredity
Most often, myopia is a hereditary disease. If both parents have mild or moderate myopia, then with a high degree of probability (75-100%) the child will also have it. If both parents have high myopia, then the children will also suffer from this disease with a 100% probability. If only one of the parents is sick, the chances are significantly reduced. Only 8% of children whose parents have normal vision develop myopia. In this situation, when only one of the parents has myopia, the child may never suffer from this disease.
Injuries
Suffered eye injuries, including birth injuries to newborns, accompanied by damage to the visual zone, without a doubt, can cause visual defects, namely myopia. This item includes traumatic brain injuries that can affect the ability to see, as well as labor.
Women with a high degree of myopia may be prohibited from giving birth naturally, as there is a high risk of losing their vision completely. Women with mild or moderate myopia after natural childbirth experienced a decrease in vision to 1-1.5 diopters, which can be explained by significant overstrain of the eye muscles during pushing.
Treatment of eye myopathy
If a patient is diagnosed with severe, moderate and mild eye myopathy, treatment involves prescribing medications to the patient that normalize metabolic processes in muscle fibers. In most cases, they resort to the following medications: Methylandrostenolone, Retabolil, as well as vitamins E and C. Therapy is not complete without pharmacological agents that improve blood circulation in tissues. In this case, drugs such as Nikoverin and Trominal can be used. In addition, pharmacological agents are used that help stabilize the processes of excitability and conductivity. For this purpose, Mestinon and Galantamine are prescribed.
It is important to know that the correct choice of medicine and the duration of its use can only be determined by a specialist who takes into account the severity of the disease, the presence of concomitant pathologies, as well as the characteristics of the body of a particular patient.
What is retinal myopathy is important to find out in advance. In the absence of timely treatment, myopia develops, which requires separate treatment.
It can actively progress and be complicated by retinal pathologies (tear, degeneration, detachment), vitreous hemorrhages, scleral staphyloma, and blindness. There are several ways to treat this pathology:
- correction with contact lenses or glasses;
- drug treatment;
- surgical intervention;
- laser correction;
- traditional methods.
Treatment
When a diagnosis of “eye myopathy” is made at any degree, therapy is carried out using medications. They normalize metabolic processes in muscle tissue.
More often they resort to the use of vitamins E and C, the drugs Retabolil, Methylandrostenolone. In combination with them, medications are prescribed to normalize blood circulation in the tissues. For this, Trominal and Nikoverin are used.
To stabilize excitability and conductivity, a substance such as Mestinon or Galantamine is used. It is worth remembering that only a doctor who has received the full diagnostic result of this case can select a drug and determine the course of treatment. It also takes into account what concomitant pathologies there are and the characteristics of the body of a particular patient.
If myopathy is not treated, myopia will soon appear. And with her, the treatment will be different. It develops rapidly, and pathologies of the retina appear in the form of detachment, rupture, and dystrophy. There are eye hemorrhages and blindness.
In addition to the above-mentioned drugs, other methods are also used. They are prescribed to each patient individually: corrective glasses and lenses, pharmaceuticals, surgery, laser treatment and traditional methods.
Features of each form of the disease
All forms of the disease differ in the localization of the pathological process, type of inheritance, and age of onset of manifestations. Also, not all forms of the disease occur with the same frequency and are equally well studied.
Duchchen's muscular dystrophy
The most studied form of pathology is Duchchen muscular dystrophy. This form has a malignant course and an unfavorable prognosis. As a rule, at 14–15 years old, patients are already completely immobilized. A child cannot walk independently at the age of 8–10 years.
The pathological process begins with the legs and waist of the lower extremities. The spread is upward. After the lower extremities, the muscles of the back, arms, and shoulder girdle are involved. At the thermal stage of development, the muscles of the pharynx, face, and respiratory muscles are affected.
The first signs include gait disturbance and pseudohypertrophy - visual enlargement and thickening of muscles
The calf muscles are the first to be affected, but pseudohypertrophy may also occur in other areas:
- buttocks;
- deltoid muscles;
- press;
- language.
The heart muscle suffers quite often, and disorders develop in the early stages of the pathological process. Sick children often suffer from mental retardation. In different cases, the degree of manifestation of oligophrenia is different, it is assumed that this depends on hereditary characteristics.
Becker muscular dystrophy
Similar in clinical manifestations to Duchenne muscular dystrophy, this form of the disease is characterized by a benign course. When inheriting, the so-called grandfather effect is often observed. This is the name for cases when a patient passes on a pathological gene to his grandson through his daughter. This option is possible due to the fact that patients remain able to work longer and their fertility does not suffer, as among patients with Duchenne muscular dystrophy.
The first manifestations of the disease begin at 10–15 years of age. Often, until the age of 30, the patient is still able to walk—sometimes longer. At the same time, the patients’ intelligence does not suffer, that is, mental retardation is not observed. Also, cardiomyopathy develops only in rare cases.
Rare forms of the disease
The rarest forms of the disease, characterized by a milder course, include:
We recommend you read:What is myasthenia gravis
- Dreyfus-Cogan muscular dystrophy;
- Mabry form;
- Rottauf-Mortier-Beyer muscular dystrophy.
The first form of the disease differs from the others in that patients with it do not develop muscle pseudohypertrophy. Also, a person’s mental abilities are preserved, and cardiomyopathy begins to develop after 30–40 years.
The Mabry form does not have markers characteristic of X-chromosomal pathologies, although it is transmitted along this chromosome. Pseudohypertrophy of the muscles is strongly expressed.
The Rottauf-Mortier-Beyer form is characterized by impaired flexion abilities in many joints. This process begins with the distal parts of the legs, then the neck is affected, and gradually the process moves to the entire spine. The patient develops a permanent pathological position of the head due to impaired neck flexion.
Patients develop paresis, but they are expressed moderately: the shoulder girdle is most often affected
The disease progresses very slowly, so many patients retain full working capacity almost throughout their lives. The most likely cause of death is cardiomyopathy. Death occurs most often at the age of 40–50 years.
Juvenile Erb's myopathy
The first symptoms of the disease appear quite late, but there are known cases of Erb's pseudo-Duchchen muscular dystrophy. In this case, the first symptoms develop before the age of 10 years. The course of the disease is more severe than in those patients in whom the first manifestations were discovered later. Intellectual abilities in patients are usually preserved. The pathological process usually begins with the pelvic girdle, then affects the shoulder girdle. In some cases, they suffer at the same time.
Facioscapulohumeral shape
Landouzy-Dejerine muscular dystrophy is more common in women. This form is characterized by a relatively simple course, but it can be aggravated by excessive physical activity, including irrational physical therapy.
Most often, patients live long - up to 60 years and even longer. The pathological process spreads from the facial muscles to the shoulder girdle, and then to the proximal parts of the arms. After this, it is sometimes possible for the pathology to spread to the lower extremities. Often the muscles are affected asymmetrically.
Ophthalmic myopathy
Ophthalmic myopathy (or progressive dystrophy of the external eye muscles).
The first description of an isolated lesion of the external eye muscles in the presence of severe bilateral ptosis and external ophthalmoplegia was made by Graefe in 1868.
Among the large number of subsequent reports describing this clinical picture (more than 100 observations), cases where this picture was one of the symptoms of various cerebral pathologies, in particular basal syphilitic meningitis, should be left aside.
The question of the pathogenesis of this phenomenon, what process underlies it, has been interpreted differently. Most authors made this disease dependent on the pathological process in the nuclei of the oculomotor nerves, drawing an analogy with spinal Aran-Duchenne amyotrophy.
The assumption that the basis of the pathological process is a chronic degenerative process in the nuclei of the oculomotor nerves, expressed by Möbius, was recognized in the studies of Wilbrand and Zenger.
However, along with this neurogenic understanding of the process, evidence has emerged about its myopathic nature. Fuchs was the first to express such an opinion in 1890. He observed 5 sick women with severe bilateral ptosis and atrophy of the upper eyelids. In one case there were indications of a familial nature of the disease. During the operation performed to correct ptosis, a piece of muscle was removed, upon histological examination of which some muscle fibers turned out to be atrophic, and an overgrowth of connective tissue was found. He did not find any pronounced hypertrophy of the fibers, but some were increased in diameter up to 65; an increase in the number of nuclear formations was noted. Fuchs concluded that in this case there was primary muscular atrophy of the levator palpebrae superioris muscle. He stipulates that the microscopic picture does not, however, give the right to confidently reject the idea of the neurogenic nature of the process.
Soon after Fuchs's report, the work of Silex appears, who observed 2 sick women with increasing paralysis of the muscle that lifts the upper eyelid. In one case, in a piece of muscle removed during cosmetic surgery, he discovered a microscopic examination of a picture characteristic of progressive muscular dystrophy. The diameter of the muscle fibers varied, ranging from 5 to 110 x; between them there was a proliferation of connective and adipose tissue; in some fibers the formation of vacuoles was noted. The author believes that in his observation, as in Fuchs’ cases, there is a picture of progressive muscular dystrophy localized in one muscle.
Although most reports express the opinion of primary nuclear degeneration, there are a number of observations that give reason to assume the myopathic nature of the process. Thus, weakness and atrophy of muscles innervated by nerves other than the oculomotor (weakness of the orbicularis oculi muscle and masticatory muscles) have been repeatedly noted.
In a number of other cases, ptosis and ophthalmoplegia were part of a more complex clinical picture characteristic of progressive muscular dystrophy. An interesting observation was made by M.P. Nikitin, who described a peculiar picture of the illness of a brother and sister (the parents were related by blood). It was manifested by bilateral ptosis and external ophthalmoplegia; at the same time, there was a mild pathology of the muscles innervated by the V, VII, IX, X and XII nerves. In addition, there was diffuse atrophy of the muscles of the limbs and trunk, characteristic of progressive muscular dystrophy.
Later M.N. Nikitin cited 2 more similar observations. One patient, along with ptosis and limited upward movement of the eyeballs, had diffuse atrophy of the muscles of the left shoulder girdle, as well as wasting of the muscles of the left leg with a noticeable decrease in tendon reflexes. The second patient had complaints of weakness, difficulty walking, mild bilateral ptosis and almost complete external ophthalmoplegia. No atrophy was noted in this patient, but there was a sharp increase in the volume of the calf muscles (pseudohypertrophy).
Thus, in the last 2 observations there was a rudimentary manifestation of developing myopagia with unusual involvement of the oculomotor muscles in the process. The myopathy was expressed much less sharply and typically than in the previously described brother and sister, but, nevertheless, the presence of this particular pathology must be recognized.
Govers described a patient who developed bilateral ptosis and external ophthalmoplegia within 3 years, and later the orbicularis oculi and facial muscles weakened and atrophied; then atrophy spread to the muscles of the arms and moved to the muscles of the pelvic girdle. Govers believes that in this case there was a progressive muscular dystrophy, approaching in its manifestations the Landouzy-Dejerine type.
A similar report belongs to Desogus: ptosis and weakness of the oculomotor muscles developed at the age of 22 years, after 9 years weakness of the facial muscles and atrophy of the muscles of the shoulder girdle and upper extremities appeared. The author believes that in this case we are talking about myopathy with an unusual onset in the form of paralysis of the extraocular muscles.
In 1936, Martin cited 3 similar observations, and in 1941, Thiebaud described a patient who developed ptosis at the age of 8, weakness of the muscles of the shoulder girdle 4 years later, and weakness of the muscles of the pelvic girdle at the age of 16. In general, the picture of the disease resembled the Erbov form of myopathy. Similar observations were given earlier by Oppenheim.
Detailed data from a microscopic examination of a piece of muscle excised during surgery was provided in 1933 by Vollaro. The orbicularis oculi muscle is thinned, individual muscle fibers vary significantly in volume; some of them are significantly reduced, their transverse striations are blurred, and some have numerous nuclei. The skin and subcutaneous tissue of the eyelids are atrophic. An interesting suggestion is made by the author, who believes that the whole process is a manifestation of trophic pathology, the result of a pathology of the sympathetic nervous system. The changes he described are very close to those observed in muscular dystrophy.
Sunaga examined the extrinsic ocular muscles in 2 cases of progressive muscular dystrophy and found histological changes consistent with myopathy. He also reports that after extirpation of the ciliary ganglia in dogs in the external muscles of the eye, he identified a picture very similar to that observed with muscular dystrophy. These data are similar to the famous Kure study, which will be presented below.
The most conclusive is the data of Kilog and Nevin on 5 patients with severe progressive dystrophy of the external muscles of the eye. In all cases, there was pronounced ptosis of the upper eyelids with external ophthalmoplegia, atrophy of the facial muscles, masticatory muscles, occipital muscles, and arm muscles; in some patients, the muscles of the lower extremities and sternocleidomastial muscles were also affected. Microscopic examination of pieces of muscle removed during operations to correct ptosis showed the presence of changes characteristic of muscle dystrophy. The diameter of individual muscle fibers varied from 7 to 92; there was an increase in the number of muscle nuclei, locally located inside the fiber, as well as the formation of vacuoles and a noticeable decrease in cross-striations. No noticeable pathology was found in the nerve fibers.
The above observations by Kilog and Nevin confirm the myopathic nature of the pathology of the external ocular muscles and the orbicularis oculi muscle. The presence in some cases of weakness and atrophy of individual muscles of the face, neck, masticatory muscles, as well as muscles of the limbs confirms the diagnosis of muscular dystrophy.
Thus, the described pathology is an integral part of a more complex myopathic syndrome. Often, ptosis of the upper eyelid and external ophthalmoplegia are only the first manifestation of muscular dystrophy; sometimes they are clinically its only manifestation. In such cases, we can talk about a special variant of progressive muscular dystrophy, as suggested by Walton and Natrass. The described variant of muscle pathology is close to the scapulohumeral-facial form of Landouzy-Dejerine.
Of course, this option also includes reservations about the legality of identifying individual forms of myopathy, which were given at the beginning of this chapter.
The distal form is not recognized by everyone as a separate variant of myodystrophy. In essence, its clinical picture differs little from the juvenile form of myopathy. But muscle atrophy begins not from the proximal limbs, but from the distal ones. Further, the atrophic process affects other parts of the body’s muscles.
We did not have a single observation where we could confidently make this diagnosis. Generally speaking, in the initial form the disease presents significant difficulties in differentiating it from Charcot-Marie neural muscular atrophy, sometimes from atypical forms of myotonic dystrophy or from atypical forms of polyneuritis. This is especially difficult in the absence of pseudohypertrophy and retraction phenomena characteristic of myopathy.
On the other hand, the absence of a degeneration reaction, fibrillations, and sensitivity disorders speaks against the neural form of amyotrophy. We must agree with the opinion of S.N. Davidenkov that the distal form of myodystrophy can be included in the usual youthful form as its random variant.