Hello dear readers of my blog!
In the last article I told you about chlamydia in general. In this article I will tell you about the most common manifestation of chlamydial infection in men and women - chlamydial urethritis.
You can read in detail about what urethritis is and what they are like in my article “Urethritis. What you definitely need to know!” and watch a video about it.
Often when talking about chlamydial urethritis, they use the name urogenital chlamydia or chlamydial infection of the lower genitourinary tract.
In adults, chlamydia infection occurs in almost 100% of cases through sexual contact, and with any form of sexual contact (vaginal, oral, anal).
The incubation period (the time elapsed from the moment of infection until the appearance of the first clinical signs of the disease) for chlamydial urethritis is on average 2-3 weeks.
With chlamydial urethritis, its latent course is possible - carriage or an asymptomatic form, when infection has occurred, chlamydia is present in the urethra, but the person does not have any signs of the disease, he does not feel anything, although at the same time, as you might guess, he is sexually contagious. It is believed that more than 70% of women have an asymptomatic course of the disease.
Therefore, my advice to you! If one of your partners is diagnosed with chlamydial urethritis, you should not immediately blame the other for the cause of the infection. We still need to figure it out, what if you had a hidden form and you are the source of infection for your other half!
If we talk about the classic course of chlamydial urethritis, then at the end of the incubation period, a person may experience the following symptoms with varying degrees of severity.
Chlamydial urethritis in men:
- mucopurulent or mucous, light discharge from the urethra;
- itching, burning, pain when urinating (dysuria);
- discomfort, itching, burning in the urethral area;
- pain during sexual intercourse (dysparreuria);
- increased urination and frequent urge to urinate;
- pain in the perineum with irradiation (“with return”) to the rectum.
Once again I want to draw your attention! Each person’s symptoms may be different; in no case should you make a diagnosis yourself, since similar symptoms may occur with another disease!
Therefore, you definitely need to go to the doctor and get examined!
Moreover, you need to be examined not only for chlamydia, but for all possible infections, since I repeat once again, the signs for different urethritis are the same, and you yourself cannot distinguish chlamydia from, for example, gonorrhea or mycoplasmosis!
Also, very often chlamydial infection is combined with pathogens of other sexually transmitted infections.
Without treatment, chlamydia can persist in the urethra of men and women indefinitely and lead to various complications affecting the pelvic organs (prostatitis, epididymitis), rectum (proctitis), pharynx (pharyngitis), and conjunctiva of the eyes (chlamydial conjunctivitis).
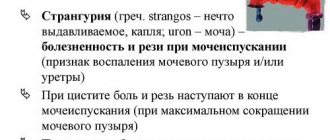
Urethritis: symptoms
As mentioned above, the signs of urethritis are most often blurred, which usually negatively affects the speed of detection of the disease and the adoption of appropriate measures.
The main signs of urethritis are considered to be:
- pain and burning during urination; pain during sexual intercourse;
- sometimes difficulty urinating with an imperative (futile) urge to urinate;
- discharge from the urethra, often copious. The discharge may be mucus or pus of various colors, sometimes found in the urine in strings. The main and most striking symptom and manifestation of urethritis in men caused by Trichomonas (trichomoniasis as such) is foamy discharge from the urethra. Otherwise, the manifestations of trichomoniasis coincide with the described symptoms of inflammation of the urethra of another etiology, as well as other problems with the genitourinary system;
- in some cases, there is also slight swelling of the tissues of the penis (head and foreskin);
- pain in the lower abdomen.
In extremely rare cases, with severely weakened immunity, symptoms of general intoxication of the body (fever, fever, etc.) may be added to the described manifestations. Moreover, this disease has the peculiarity of quickly passing into a chronic stage, in which the unpleasant manifestations of the disease disappear and reappear only during an exacerbation. As for the trichomoniasis type of disease, its symptoms most often make themselves felt 10–15 days after infection with Trichomonas, in accordance with the incubation period of this disease.
Due to the vague symptoms of the disease, which rarely causes a man much concern, its treatment usually begins late. When the first signs of the disease appear, you should seek advice from a specialist, because the sooner you start treating urethritis in men (and trichomoniasis), the easier it will be to get rid of the inflammation and its causative agents.
Initial appointment
An initial appointment with a specialist involves a thorough interview and examination of the patient (preliminary medical history), as well as the appointment of tests, which in the case of trichomoniasis (trichomoniasis) urethritis are of particular importance, as they allow one to accurately determine the causative agent of the disease.
Diagnosis of urethritis involves the use of modern methods for detecting infectious and bacterial agents in the human body and most often includes:
- Analysis of urine;
- analysis of discharge from the urethra, as well as scraping from the urethra: both of them make it possible to determine the type of causative agent of infection and inflammation. This is done either by culture or using PCR (polymerase chain reaction), which makes it possible to accurately identify the DNA of the agent (this is one of the main methods for diagnosing trichomoniasis). In the case of trichomoniasis urethritis, establishing the presence of trichomoniasis most often involves preliminary therapy designed to remove microorganisms from a latent (hidden) state. Provocative therapy involves drug intervention (medicines are injected either into the blood or directly into the urethra). At the same time, the specificity of trichomoniasis suggests that in order to identify the pathogen it is necessary to take a smear and scraping several times (usually three times over three days);
- blood test: allows you to determine the degree of development of inflammation (based on the level of leukocytes).
Test for chlamydia
To test for chlamydia in urethritis, a smear is often taken - a scraping from the urethra. Moreover, to obtain reliable results, it is recommended not to urinate for at least 3 hours before taking the test. This is very important to obtain reliable survey results.
I would like to draw your attention to the fact that nowadays, with modern diagnostic methods, there is no need to drink any beer before taking the test, although such advice can be found on the Internet!
Diagnosis usually occurs using molecular biological methods of laboratory research, for example PCR (polymerase chain reaction), when specific fragments of DNA and/or RNA of chlamydia trachomatis are detected.
Important! If a person’s test for chlamydia is positive, but there are no subjective and objective signs of an infectious-inflammatory disease and risk factors for getting this infection, additional research must be done using a different method to confirm the diagnosis!
TRICHOMONAS INFECTION: CLINICAL COURSE, DIAGNOSIS AND TREATMENT
Complications of trichomoniasis can cause infertility, pathology of pregnancy, childbirth, diseases of the newborn, infant mortality, the birth of defective offspring, etc. Only in 10.5% of patients trichomoniasis occurs as a monoinfection; in other cases it is a mixed protozoal-bacterial process. Treatment of trichomonas infection should be comprehensive and include the prescription of not only protistocidal drugs, but also nonspecific treatment methods. Success in the fight against trichomoniasis is possible only with close cooperation between venereologists, urologists and gynecologists. Trichomoniasis is a sexually-transmitted abnormality which ranks the first among worldwide diseases. Its complications include sterility, abnormal pregnancy, labor, neonatal morbidity and mortality, congenital defects, etc. As high as 10.5% has trichomoniasis as a monoinfection, while in other cases it is a mixed protozoan and bacterial process. The treatment of Trichomonas infection must be combined and include not only protistocidal agents, but also nonspecific therapies. Trichomoniasis can be successfully controlled only through joint efforts made by venereologists, urologists, and gynecologists.
E.A.Mezhevitinova - senior researcher, candidate of medical sciences, O.I. Mikhailova - doctor of the department of the Scientific Center of Obstetrics, Gynecology and Perinatology (director - Academician of the Russian Academy of Medical Sciences, Prof. V.I. Kulakov), RAMS, Moscow
Ye.A. Mezhevitinova, Candidate of Medical Sciences, Senior Researcher, OIMikhailova, Physician, Research Center of Obstetrics, Gynecolophy and Perinatology (Director Prof. VIKulakov, Academician of the Russian Academy of Medical Sciences), Academy of Medical Sciences, Moscow
T
Richomoniasis is one of the most common diseases of the genitourinary tract. Around the world, trichomoniasis affects 170 million people every year. This disease equally often affects both women and men. In girls, Trichomonas infestation is extremely rare. The causative agent of genitourinary trichomoniasis is Trichomonas vaginalis, which belongs to the protozoa, the class of flagella, the genus Trichomonas, which is a mobile single-celled organism that has adapted in the process of evolution to life in the organs of the human genitourinary system. To date, more than 50 varieties of Trichomonas are known. Only 3 types of Trichomonas parasitize humans: urogenital, oral and intestinal. Urogenital trichomonas are an independent species, morphologically and culturally different from oral and intestinal trichomonas. In women, the habitat of Trichomonas is the vagina, in men - the prostate gland and seminal vesicles. The urethra can be affected in both men and women. Infection with trichomoniasis occurs from a sick person. Women who have casual sex suffer from trichomoniasis 3.5 times more often than those who have one sexual partner. Protozoa enter the mucous membranes of the genitourinary tract through contact with a patient with trichomoniasis or a carrier of trichomonas. Trichomonas are fixed on the cells of the squamous epithelium of the mucous membrane, penetrate into the glands and lacunae. Once in the genitourinary organs, Trichomonas can cause the development of an inflammatory process.
Clinical signs
The internal os of the cervix is a kind of boundary for the upward spread of urogenital trichomonas due to the circular compression of the cervical muscles and the sharply alkaline reaction of the endometrial secretion. These protective barriers lose their strength during menstruation, abortion and childbirth. In addition, the rhythmic movements of the uterus during sexual intercourse are predisposing factors for the absorption of urogenital trichomonas located in the cervix into its cavity. When trichomonas penetrate into the pipes, trichomonas salpingitis occurs. As a rule, there is no isolated inflammation of the ovaries; usually this lesion is observed together with damage to the tubes. Urogenital Trichomonas penetrate into the ovary through the wound surface of a burst Graafian vesicle. Tuboovarian formations may occur. Urethritis can be either primary or secondary. Most often, the anterior part of the urethra is affected, but sometimes the infection spreads to the posterior part of the urethra and total urethritis occurs; with a long course, the formation of multiple strictures is possible. Paraurethritis, cystitis and even pyelitis may occur.
| Depending on the duration of the disease and the intensity of the body's reaction to the introduction of the pathogen, the following forms of trichomoniasis are distinguished: • fresh (acute, subacute, torpid); • chronic (torpid course and duration of the disease over 2 months or not established); • Trichomonas carriage (in the presence of Trichomonas there are no objective and subjective symptoms of the disease). |
None of the clinical signs of Trichomonas infection are strictly specific. For acute trichomoniasis
the inflammatory process proceeds rapidly with copious discharge that irritates the skin and severe itching of the external genitalia.
I am concerned about burning and pain when urinating. Complaints appear soon after the start of sexual activity or casual sexual intercourse. The incubation period for trichomoniasis is on average 5-15 days. Clinical manifestations of the inflammatory process intensify after menstruation. Upon examination, inflammatory changes are revealed from moderate hyperemia of the vaginal vault and cervix to extensive erosions, petechial hemorrhages and diaper rash in the perineal area. A very characteristic, but not constant symptom is the presence of granulomatous, loose lesions of the mucous membrane of the cervix, red in color (crimson cervix). In the area of the posterior fornix, there is an accumulation of liquid grayish-yellow, foamy discharge that flows freely from the vagina, irritating the skin. Genital warts may form in the area of the vaginal vestibule. When the urethra is involved in the inflammatory process, its lips are often swollen and hyperemic; a small amount of purulent discharge can be squeezed out with a massage. When palpating the urethra, its soreness and pastiness are noted. There may be hyperemia at the mouth of the duct of the greater vestibular gland. During colposcopy, pinpoint hemorrhages are detected on the mucous membrane of the vagina and the vaginal part of the cervix (strawberry cervix symptom). Foci of inflammation when stained with Lugol's solution are iodine negative. In the subacute process,
the symptoms are minor, the discharge is not abundant.
The torpid form of trichomoniasis, which most often occurs in men, is characterized by a paucity of objective and subjective symptoms or their complete absence. In women, the mucous membranes of the vagina and external genitalia are of normal color or slightly hyperemic, vaginal discharge is milky in color, and its amount is insignificant. Obliterated signs of the inflammatory process (often pronounced focal or diffuse hyperemia, petechiae) are revealed only during colposcopy. The transition of infection to the chronic stage occurs through the gradual subsidence of acute and subacute phenomena. However, periodic exacerbations may occur, which are most often caused by sexual intercourse, alcohol consumption, decreased body resistance, ovarian dysfunction and changes in the pH of the vaginal contents. Chronic genitourinary trichomoniasis,
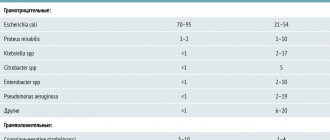
as a rule, is a mixed protozoan-bacterial process (B.A. Terekhov, A.A. Letuchikh, 1982), since Trichomonas is a reservoir for chlamydia, ureaplasma, gonococci, staphylococci and other flora. Only in 10.5% of patients trichomoniasis occurs as a monoinfection; in 89.5% of cases mixed trichomonas infections in various combinations are detected. According to our data, Trichomonas vaginalis is most often found in association with mycoplasmas (47.3%), gonococcus (29.1%), gardnerella (31.4%), ureaplasma (20.9%), chlamydia (18.2% ), mushrooms (15.7%). Under the influence of protistocidal therapy, urogenital trichomonas, as a rule, disappear. However, clinical recovery does not always occur - post-Trichomonas inflammatory processes remain. Their formation is facilitated by the fact that with the death of urogenital trichomonas, inflammation is supported by the abundant microflora that accompanies trichomoniasis. With mixed lesions, complications in patients are observed 2 times more often and are more profound. Post-trichomonas inflammatory process after treatment is diagnosed in 14.6 - 48.2% of women. Treatment of trichomoniasis with protistocidal drugs leads to the release of the flora located inside the trichomonas and the maintenance of the inflammation process. Significant disorders that develop in the body of patients with mixed urogenital infections are difficult to correct with therapeutic agents, which contributes to the occurrence of relapses and causes an extremely persistent course of the process, despite the use of etiotropic therapy. Relapses occur in 20% of cases [1]. Trichomonas carriage should be understood as the presence of Trichomonas in the human body in the absence of clinical signs of the disease. The frequency of Trichomonas carriage, according to various authors, ranges from 2 to 41%. The true number of Trichomonas carriers is unknown. Trichomonas carriage depends both on the strain of Trichomonas and on the characteristics of the host organism. In Trichomonas carriers, the natural immune response to the introduction of Trichomonas antigens, related to the antigens of their own erythrocytes, develops insufficiently. Local cellular immunity also plays a role. Trichomonas carriers, like patients with a sluggish inflammatory process, pose a serious epidemiological danger, being a source of spread of trichomoniasis. Trichomonas infection does not lead to the development of pronounced immunity. Serum or secretory antibodies (Ab) detected in patients or survivors of trichomoniasis are only signs of an existing or previous infection, but are unable to provide immunity. They are detected within a year after the illness.
Diagnostics
The diagnosis of genitourinary trichomoniasis is established on the basis of clinical signs of the disease and the detection of trichomonas in the test material. For high-quality laboratory research, proper preparation of the patient for laboratory examination is important. A necessary condition is to stop the use of external and internal trichomonocidal agents 5 - 7 days before taking the material. Material for research is taken from the vagina, urethra, rectum in women and from the urethra, rectum in men; urine centrifuge and rinsing waters are also used. The material is taken with a metal loop, a pipette with a rubber balloon, or a grooved probe is used.
| For laboratory diagnosis of trichomoniasis, the following methods are used: • microscopy of the native drug; • microscopy of a stained specimen; • cultural; • immunological. |
In native preparations
The pathogen is detected by its movement among cellular elements and microorganisms.
Trichomonas vaginalis is identified by its pear-shaped and oval shape, slightly larger than a leukocyte, characteristic jerking movements and flagella, which are especially clearly visible when examined under a phase-contrast microscope. Due to the fact that when the native drug remains at room temperature for a long time, Trichomonas lose their mobility, the study should be carried out as quickly as possible after receiving the material. The advantage of studying Trichomonas in stained preparations
is the possibility of studying them long after the material was taken.
In stained preparations, Trichomonas have an oval, round or pear-shaped shape with well-defined contours and a delicate cellular structure of the cytoplasm. The information content of this method is higher, since not only mobile forms are determined, but also stationary ones. If the results of direct examination of the pathological material are negative, Trichomonas can be detected by culturing
discharge from the urethra, vagina, prostate secretion and sperm.
The cultural method is of great value in recognizing atypical forms for the purpose of diagnosing trichomoniasis and monitoring the results of treatment. Immunological methods
have also been repeatedly proposed for the diagnosis of trichomoniasis, but they do not give satisfactory results. None of these methods guarantees complete detection of Trichomonas. Therefore, to increase the percentage of detection of trichomonas, it is necessary to resort to repeated repeated studies in all patients using all available laboratory diagnostic methods. All of the above examination methods complement each other. Their combination dramatically increases the detection of Trichomonas vaginalis.
Treatment
Treatment of genitourinary trichomoniasis is one of the urgent and serious challenges facing doctors all over the world, which is due to the high incidence of this infection, the lack of a guaranteed etiological cure for trichomoniasis and the significant proportion of post-trichomoniasis complications.
| When treating trichomoniasis, the following principles must be observed: • both sexual partners should be treated simultaneously; • sexual activity and drinking alcohol during the treatment period are not recommended; • factors that reduce the body's resistance (concomitant diseases, hypovitaminosis) are eliminated, if possible; • it is necessary to use trichomonocidal drugs against the background of general and local hygiene procedures; • patients with all forms of the disease are subject to treatment (including Trichomonas carriers and patients with inflammatory processes in whom Trichomonas are not detected, but these pathogens are detected in a sexual partner). |
The main principle of treatment of genitourinary trichomoniasis is an individual approach to the patient, based on a thorough analysis of the anamnesis and a comprehensive clinical and laboratory examination. One of the most effective general drugs for trichomoniasis is metronidazole. Metronidazole
acts not only on protozoa, but also on anaerobic flora.
In addition, metronidazole can induce the production of interferon. The minimum inhibitory concentration of metronidazole under aerobic conditions is 1-10 mcg/ml, under anaerobic conditions it is 0.1-7.0 mcg/ml. The majority (76%) of Trichomonas vaginalis strains die at a concentration of metronidazole in the medium of 3.0 - 5.0 μg/ml. The most acceptable method of introducing metronidazole into the body to achieve its maximum concentration in the blood serum is oral. For the treatment of genitourinary trichomoniasis, a wide variety of methods have been proposed, differing in the use of both single and course doses, intervals between doses and duration of treatment. However, etiological cure is not guaranteed when using existing regimens. Relapse rates range from 2.2 to 44.1. There are several methods of treatment with metronidazole: - 0.5 g 3 times a day for 5 days; course dose 7.5 g - single oral dose 2 g. Currently, in addition to metronidazole, a number of other nitroimidazole derivatives are used. Tinidazole.
Prescribed 0.5 g every 15 minutes for an hour;
course dose 2 g or 0.5 g 2 times a day every day for a week. Ornidazole.
An antimicrobial agent for the treatment of infections caused by trichomonas, amoebas, lamblia, anaerobic bacteria, prescribed once 1.5 g or 0.5 g 2 times a day for 5 days;
for a course of treatment 5 g. Tenonitrazole.
Capsules of 0.25 g, 8 pieces per package.
It has an antitrichomocidal and antimycotic effect; 1 capsule is prescribed 2 times a day for 4 days. Nimorazole
is prescribed 0.5 g 2 times a day for 6 days or a single dose of 2 g per day (4 tablets).
In the torpid and chronic process, due to impaired vascularization with the subsequent development of scar tissue in the affected organs, the morphological structure of the vaginal mucosa is disrupted, and protistocidal drugs penetrate into the lesions in a lower concentration, which is insufficient to suppress the parasite, which in turn leads to drug resistance of Trichomonas to the prescribed doses. In the treatment of sluggish, chronic, recurrent, complicated genitourinary trichomoniasis, the following treatment regimens are recommended: • metronidazole 0.5 g 4 times a day for 5 days, a course dose of 10 g or a daily dose of 1 - 1.5 g for 10 days , course dose 10 -15 g (for excess body weight - more than 90 kg - the daily dose increases to 2 g), or 100 ml of metronidazole solution (containing 0.5 g of the drug), administered intravenously for 20 minutes 3 times a day for 5-7 days; • Tinidazole is prescribed 2 g per day once for 2 days, course dose is 4 g. Treatment of a chronic process should be comprehensive and include nonspecific treatment methods aimed at increasing the patient's body's defenses. For this purpose, for chronic and torpid forms of trichomoniasis, nonspecific immunotherapy (pyrogen drugs, biogenic stimulants, vitreous, aloe, FIBS), vitamin therapy, and proteolytic enzymes are recommended. Proteolytic enzymes are highly active biological preparations that have necrolytic, fibrinolytic, mucolytic and anti-inflammatory effects. They enhance the effect of antibacterial drugs and reduce the resistance of microflora to them. Proteolytic enzymes enhance the trichomonas activity of metronidazole by 2-10 times. They help accelerate proliferative processes in tissues, activate cellular reactions, and enhance the phagocytic activity of leukocytes. Proteolytic enzymes
can be of animal (trypsin, chymotrypsin) and plant (terrilitin) origin.
There are commercially available preparations that include both enzymes. The use of these drugs significantly increases the effectiveness of complex therapy, helps reduce relapses of the disease, prevents and reduces the frequency of peritubar adhesions. Crystalline trypsin is prescribed 10 mg once a day intramuscularly for 5 days. Then or simultaneously, etiotropic therapy is carried out. Terrylitin is administered rectally or vaginally at a dose of 600 - 1000 units 2 - 3 times a day for 5 - 10 days. Then etiotropic treatment is carried out. Administration of terrilitin is continued throughout the course of treatment. Wobenzym is a film-coated tablet, resistant to the action of gastric juice, containing bromelain (45 mg), papain (60 mg), pancreatin (100 mg), chymotrypsin (1 mg), trypsin (24 mg), amylase ( 10 mg), lipase (10 mg), rutin (50 mg). In the treatment of Trichomonas infection, Solko-Trichovak can be used. Solko-Trichovak
is a lyophilisate of inactivated microorganisms of specially selected strains of Lactobacillus acidophilus.
One bottle (single dose) contains 7. 109 inactivated lactobacilli, 5 mg repolymerized gelatin, 0.2 mg phenol as preservative. The main indications for use are vaginal trichomoniasis and bacterial vaginosis. The vaccine is used simultaneously with chemotherapy, since the development of AT lasts 2 - 3 weeks. The vaccine can be used as monotherapy for torpid trichomoniasis and in cases of resistance to chemotherapy. ATs induced by vaccination with Solco-Trichovac are capable of directly affecting not only Trichomonas vaginalis, but also anaerobic flora (staphylococci, streptococci B and D, enterobacteria, etc.). The main vaccination - 3 injections of 0.5 ml intramuscularly with an interval of 2 weeks - provides one-year protection. A year later, repeated vaccination is carried out - once 0.5 ml. Vaccination with Solko-Trichovak leads to the stabilization of normal vaginal microflora. After 3 injections of the drug, the normal vaginal flora is stabilized, immunity is increased, as a result of which Trichomonas and other pathogenic pathogens are forced out and disappear. In outpatient treatment, protistocidal drugs and immunotherapy are prescribed simultaneously. Local treatment of trichomoniasis
is prescribed in the presence of contraindications to the use of metronidazole, as well as in patients with a torpid recurrent course of the disease.
When prescribing local therapy, it is necessary to take into account the stage of the inflammatory process. In acute cases, douching, baths with infusion of chamomile flowers and sage herbs are used. For local treatment of colpitis, Klion is used, which is used in the form of vaginal tablets 1 time per day for 10 days. The drug contains 0.5 g of metronidazole and 0.15 g of miconazole nitrate, therefore it is especially effective for mixed candidiasis-trichomoniasis infection. Drug for local treatment terzhinan. This drug contains ternidazole (200 mg), neomycin sulfate (100 mg), nystatin (100,000 units), prednisolone (3 mg), clove and geranium oils as excipients. Ternidazole is effective against trichomonas and aerobic infections, nystatin has an antifungal effect, neomycin sulfate has an antibacterial effect on gram-positive and gram-negative bacteria, prednisolone has an anti-inflammatory effect. Therefore, this drug may be useful in the treatment of mixed infections. Chronic inflammatory process in 89.5% of cases occurs as a mixed infection. Disorders that develop in the body of patients with mixed urogenital infections and are difficult to correct with therapeutic agents contribute to the recurrence of the disease, causing an extremely persistent course of the process despite the use of fairly effective etiotropic drugs. Nitroimidazole derivatives affect Trichomonas, causing their death, and do not affect the accompanying vaginal flora, which contributes to the development of the post-Trichomonas inflammatory process. In case of mixed infection, it is recommended to prescribe protisticidal agents on an outpatient basis simultaneously with drugs that act on the accompanying flora. Treatment of trichomonas infection during pregnancy
In the first trimester of pregnancy during the period of organogenesis and placentation, treatment with protistocidal drugs is not indicated, since as a result of the pathogenic effect of metronidazole in the embryo and fetus, those organs and systems that are in the process of differentiation at this time may be affected primarily . They recommend daily lubrication of the urethra and vagina with a 4% aqueous solution of methylene blue or brilliant green or a solution of potassium permanganate (1:10,000). In the second trimester of pregnancy, it is permissible to use vaginal suppositories with metronidazole (1 suppository at night for 8-10 days), since during this period redox reactions of the fetus develop, associated with the inactivation of drugs. It is also possible to use terzhinan. Treatment with metronidazole tablets can only be prescribed in the third trimester of pregnancy. However, when prescribing it, it is necessary to take into account the decrease in detoxification and excretory function of the kidneys, characteristic of pregnancy, and the slowdown in metabolism and excretion of chemical compounds from the body. Metronidazole during pregnancy is prescribed in a lower dosage than outside it (0.25 g 2 times a day for 8 days; course dose 3 - 4 g).
Clinical examination
One of the unsolved problems in the fight against trichomoniasis is the problem of medical examination of patients. According to Order 286 of the Ministry of Health of the Russian Federation dated December 7, 1993, work on identifying patients, diagnosing, treating and preventing trichomoniasis can be carried out by doctors in dermatovenerological dispensaries, obstetric-gynecological, urological and other treatment and preventive institutions. The cure of genitourinary trichomoniasis is established using bacterioscopic and cultural research methods. The first control studies in women are carried out 7-8 days after the end of treatment. If necessary, a provocation is carried out: an injection of gonovaccine (500 million microbial cells) or pyrogenal (200 MTD) and after 24, 48 and 72 hours the discharge of the urethra, vagina, and rectum is examined. The second control examination is carried out immediately after the next menstruation. Material for research must be taken from all lesions. A patient with trichomoniasis is under medical supervision to establish cure after completion of treatment for fresh trichomoniasis for 2 months, for chronic trichomoniasis for 3 months. For patients with an unidentified source of infection, the period of follow-up observation is increased to 6 months. At the same time, monthly clinical and serological examinations are carried out to detect syphilis, since metronidazole has treponemocidal properties and can complicate its diagnosis.
Cure criteria:
• absence of trichomonas when examining discharge from the urethra, urethra, vagina, rectum; • favorable results of clinical and laboratory studies during 2-3 menstrual cycles; • absence of clinical manifestations of Trichomonas infection. Taking into account the criteria for cure, if the results of clinical and laboratory tests are favorable, patients are removed from the register.
Prevention
Preventive measures for trichomoniasis should be aimed at timely and complete identification of those infected with Trichomonas. They include: identification and treatment of patients with trichomoniasis; identification, examination and treatment of sexual partners; examination for trichomoniasis of all persons suffering from inflammatory diseases of the genitourinary organs; periodic examination for trichomoniasis of persons working in children's groups, hospitals, maternity hospitals; sanitary and hygienic measures (disposable instruments, sterilization); sanitary - educational and educational work among the population; use of barrier methods of contraception.
Literature:
1. Klimenko V.N. Trichomoniasis. - 1990. 2. Anchupane I.S. Urogenital trichomoniasis and mixed trichomonas-gonococcal infections / Abstract of thesis. Ph.D. honey. Sci. M., 1992. 3. Yatsukha M.V. Some aspects of the epidemiology of trichomoniasis. //Vestn. dermatol. and venerol. 1989. - No. 1. - P. 36-9. 4. Zemtsov M.A. Modern methods of treatment of genitourinary trichomoniasis and trichomonas-chlamydial infection in women. /Authorref. diss. Ph.D. honey. Sci. M., 1995. 5. Kurashvili N.V. Study of some biological Trichomonas and immunological changes in patients with trichomoniasis properties. /Authorref. diss. Ph.D. biol. Sci. Tbilisi, 1989. 6. Vakhnina T.E. Improving laboratory diagnostics of genitourinary trichomoniasis./Author. diss. Ph.D. biol. Sci. M., 1990. 7. Bednova V.N., Vasiliev N.M. The use of proteolytic enzymes for the treatment of trichomoniasis.//Vestn. dermatol. and venerol. - 1992. - No. 3. — P.16-20 8. Abdumalikov R.A. A comprehensive method of treating patients with genitourinary trichomoniasis. / Diss. Ph.D. honey. Sci. M., 1995. 9. Delectorsky V.V., Khabarov V.A., Skuratovich A.A. and others//5th All-Russian Congress of Dermatologists: Abstracts of reports.-Vladimir, 1983.-P.83-4 10. Badanoiu A., Toma D., Tolea L., et al. Derm.-Vener. (Buc.). 1982; 27 (1): 29-32 11. Osoba AO. Hautarzt. 1981; 32 (5): 228-32.