Overactive bladder (OAB) is a symptom complex characterized by urgency, nocturia (frequent urination at night) with or without urinary incontinence, and frequent urination in the absence of a proven urinary tract infection or other obvious pathology of the lower urinary tract. Imperative (urgent) urinary incontinence is periodic uncontrollable leakage of urine against the background of a sudden urge to urinate. This urge is so categorical (imperative) that the person simply does not have time to get to the toilet. Almost immediately after the urge, urine production begins.
OAB is a widespread syndrome. According to the International Continence Society, 17% of European adults have symptoms. It should be noted that OAB without urinary incontinence (“dry OAB”) is observed in 7.6% of women, and OAB in combination with urgent urinary incontinence is observed in 9.3%. Currently, there is a trend towards an increase in the incidence of OAB with urinary incontinence in women from 12% under the age of 60 years to 20% at the age of 65 years and older. In general, this is more pronounced in women after 44 years of age, and in men after 64 years of age. There is no definitive data on the prevalence of OAB in Russia, but it is generally accepted that it is similar to that in European countries.
Although OAB is more often diagnosed in older adults, its symptoms also occur in other age groups. The largest number of patients was observed over the age of 40 years. In men over 60 years of age, there is a clear trend towards an increase in incidence, and in women - towards a decrease. Thus, OAB is a fairly common clinical syndrome, occurring in various age groups and leading to physical and social maladjustment.
The main cause of urgent and frequent urination is special changes in the detrusor (the muscular lining of the bladder), leading to its involuntary contractions. In patients with OAB, the nerve endings located in the bladder are in a state of chronic irritation and randomly transmit signals to the brain. This prevents the bladder from storing urine adequately and causes it to contract involuntarily during filling, resulting in urge incontinence.
The significance of the OAB problem lies in its pronounced negative impact on the quality of life of patients. OAB becomes the cause of social maladjustment and serious psychological problems, leading to abandonment of the usual way of life, for example, due to a significant impact on professional activity.
Patients require a basic examination to rule out urological and other diseases that can cause urgency and frequency of urination. Diagnosis of OAB can be successfully performed on an outpatient basis and in most cases does not require special examination methods.
As a rule, in order to exclude other diseases, patients with frequent and urgent urination are assessed for urination frequency, urine tests, ultrasound of the kidneys, bladder, prostate, and the volume of residual urine is determined.
A voiding diary is also important in identifying an overactive bladder.
Approaches to the treatment of OAB
Treatment of OAB begins with non-drug methods.
Behavioral therapy
in the treatment of OAB, it is aimed at forming a new urination pattern or restoring the previous one, in which this process again becomes controllable for the patient. When reviewing the voiding diary data together, the clinician should look for episodes with the longest time between voids and the largest volume of urine output. Together with your doctor, you can determine the minimum period of time that must be observed between urinations, for example, every 2 hours, not earlier. This regime is observed for 2 weeks, then, if this condition is successfully met, the interval between urination is extended every week by 15 minutes until a 3- or 4-hour interval is reached.
Correction of drinking regime
If you suffer from urinary incontinence and/or frequent urination, you often limit the amount of fluid you take in, thus trying to reduce involuntary urine loss. To reduce the frequency of urination at night, you should limit your fluid intake at least 4 hours before bedtime. The nature of the fluid taken is an important factor that increases the intensity of urgency and the amount of urine produced. Thus, caffeine-containing liquids (coffee, tea, Coca-Cola, etc.) not only have a weak diuretic effect, but also increase urination. The intake of such drinks should be limited to 1-2 cups per day.
Tablet drugs
, as a rule, the doctor prescribes at the beginning of treatment, but you should check with the doctor about the possible side effects of such therapy.
Use of botulinum neuroprotein
in the treatment of urological diseases, it allows you to successfully cope with the symptoms of OAB, the correction of which was previously considered ineffective and even impossible. The mechanism of action of botulinum toxin type A (BTA) is to block the release of the neurotransmitter acetylcholine, which leads to detrusor relaxation and an increase in bladder volume. BTA injections are performed intradetrusorically (intravesically). To maintain a lasting positive effect, it is important and necessary to follow the principle of continuous treatment of OAB from the moment of diagnosis.
Clinical studies have shown that a single intravesical administration of BTA is effective, reduces the severity of symptoms of urge urinary incontinence, improving quality of life. Treatment is carried out on average every 4–8 months.
When discussing the issue of botulinum therapy, it should be borne in mind that in Russia there is only one original toxin that is officially approved for use in urology and has an impeccable evidence base confirming its effectiveness, safety and tolerability.
Treatment
Conservative therapy
Lifestyle correction. The doctor gives recommendations on drinking regimen, nutrition (to normalize weight, limit caffeine), and exercises that help strengthen the pelvic floor.
Drug treatment. Pharmacotherapy aimed at eliminating the cause of the disease or regulating urination is very effective.
Neurotropic drugs harmonize the functioning of the nervous system. For example, to alleviate/eliminate the symptoms of an overactive bladder, treatment with anticholinergic drugs (M-anticholinergics) is prescribed.
The neurogenic overactive bladder that appears during menopause in women with urge urinary incontinence responds to treatment with hormone replacement therapy.
If the cause of the disease is an inflammatory process, courses of antibiotics will help.
Surgery
If a stone or tumor is detected in the bladder, surgical treatment is necessary. We perform high-tech minimally invasive operations:
- TUR of the bladder - transurethral removal of a tumor (including malignant) from its wall through the urethra without an incision in the skin;
- endoscopic contact cystolithotripsy - intravesical destruction and removal of pieces of stone through the urethra. If necessary, it is possible to simultaneously perform TUR - transurethral resection of prostate adenoma.
If the cause of unregulated urination in women (urine leakage) is different, for example, stress urinary incontinence, then our hospital performs a modern minimally invasive operation with urosling , which solves the problem. This surgical treatment option is purely for women. Urosling, like a hammock, supports a sagging urethra in the correct position, eliminating the cause of the disorder and the symptom itself.
For overactive bladder, the price for treatment depends on the individual situation of the particular patient - the treatment methods indicated for him or the need for surgical intervention. And this becomes clear after a urogynecological examination.
If you experience problems with urination, contact the Clinical Hospital on Yauza. With us you will receive comprehensive assistance - an expert examination to identify the causes of an overactive bladder in both men and women, and treatment to any extent you need.
Sign up for a consultation
Before contacting a specialist, answer the following questions
1. Do you experience frequent urination (>8 times during the day, >1 time at night)?
2. Do you have urgent (sudden) urges that are difficult to control? 3. Do you experience involuntary urinary discharge? 4. Do you use urological pads? 5. Do you have neurological or other diseases that can affect bladder function (consequences of stroke, neuropathy due to diabetes mellitus, osteochondrosis, herniated discs)? 6. Have you had brain/spinal cord or pelvic surgery? 7. Do you have inflammatory diseases of the genitourinary area that are difficult to treat with antibiotics? 8. Are there any discomfort or pain in the bladder, genitals, or perineum? If you answered yes to 2 or more questions, you should contact a specialist.
This syndrome represents urinary disorders of central and peripheral origin, such as frequent urges during the day and even at night, difficult to control, leading to urinary incontinence. This syndrome is a so-called diagnosis of exclusion, a functional disorder, since one of the diagnostic criteria is the absence of infection and other organic pathology of the urinary system.
The prevalence of “overactive bladder” has recently been increasing, which may be due to the psychogenic cause of the pathology. The disease occurs equally often among men and women of different age groups, but the peak incidence occurs in old age. The main complication of a long-term disease is the development of neurosis-like or borderline mental disorders - somatoform disorders, hypochondria, depression, anxiety-phobic neurosis, obsessive-compulsive neurosis and other pathologies that seriously disrupt the adaptation of patients in all spheres of life. It can be assumed that mental disorders are not only supporting factors, but also predisposing to this syndrome.
Currently, there are several theories that prove the neurogenic cause of this disease (various disorders in the nervous system), but they do not explain all cases of the disease. If it is impossible to determine the cause, then in medicine it is customary to use the concept “idiopathic” - which means the cause of any disease or syndrome has not been established to date.
The neurogenic theory implies any disorder in the central or peripheral nervous system, which leads to disruption of the regulation of the urination process (stroke or other pathological lesions in certain parts of the brain, damage to nerve pathways, multiple sclerosis). Increased excitability of muscle and epithelial tissue is also noted, but as already mentioned, these reasons cannot explain all cases. Predisposing factors include age (the risk of pathology increases with age), smoking, obesity, poor diet, hormonal changes, and mental stress.
Symptoms of “overactive bladder” are mainly associated with disturbances in the urination process and are represented by the following options:
- pollakiuria (frequent urge to urinate)
- nocturia (night urination, which requires a special interruption of sleep to go to the toilet, which is not normally typical for a healthy body)
-enuresis (severe urge to urinate, which is accompanied by urinary incontinence)
All these symptoms are characterized by suddenness, because most often they occur when the bladder is not full.
If you suspect overactive bladder syndrome, you should seek help from a urologist, who may additionally prescribe a consultation with a neurologist and a gynecologist.
A large number of different methods are used for diagnosis, because functional diseases are difficult to diagnose precisely because to establish them it is necessary to exclude other causes. To identify characteristic complaints, the doctor can use specially designed questionnaires. The examination in most cases is of no diagnostic value, but should be carried out in all patients. Laboratory diagnostics includes studies such as general and bacteriological urine tests, general and biochemical blood tests. It is important to properly conduct a neurological examination, which can identify the neurogenic cause of the disease and refer the patient to a neurologist.
Since many diseases of the urinary system can be accompanied by similar symptoms, it is necessary to conduct a thorough examination to identify them. One of these methods is cystoscopy - insertion of a cystoscope into the cavity of the bladder, which allows you to directly see and evaluate the condition of the mucous membrane of the bladder. Indirect visualization methods - ultrasound, CT, MRI - are of indirect importance. Urodynamic studies make it possible to identify characteristic symptoms and judge the mechanisms of developed disorders. The absence of any disorders in the urinary system gives grounds to make a diagnosis of “Overactive Bladder”.
For treatment, non-drug means such as behavioral therapy (so-called psychotherapy) and maintaining the correct “water” regime are used.
Among the medications, you can use anticholinesterase drugs (blockers of the effects of the parasympathetic nervous system), beta-adrenergic receptor agonists (activate the effects of the sympathetic nervous system) - both groups of drugs allow you to relax the muscle - the detrusor of the bladder (the muscle that promotes urination). The drug desmopressin is used only as indicated in patients with diabetes insipidus and nocturnal enuresis. Neuromodulation methods and the introduction of special blocking drugs into the detrusor (bladder muscle) are used in patients resistant to therapy with the above drugs.
What are the features of the treatment of mixed urinary incontinence?
Firstly, in this case, additional diagnostics are needed to confirm (or exclude) the mixed form. The basis of additional examination is a comprehensive urodynamic study (CUDI)
, which allows you to find out which of the two types of incontinence is more pronounced. Depending on the results of KUDI, treatment will begin with the form of incontinence that is more pronounced. Only if the patient’s stress form predominates, then the first stage is implantation of a suburethral sling. And after the operation, treatment for OAB begins.
Types of urinary incontinence
1. Urgent (imperative) urinary incontinence. This type of problem is associated with an overactive bladder (OAB), when the bladder contracts beyond the person's control. This may be felt as an irresistible urge to go to the toilet, which patients are unable to restrain, and, sometimes, an involuntary leakage of urine that follows. Often the cause of such symptoms can be various disorders of the nervous regulation of the bladder (after strokes, spinal cord or brain injuries, diseases of the nervous system). However, in most cases the true cause cannot be identified. Excessive intake of substances that irritate the bladder - coffee, tea, chocolate, cola, sour fruit juices - can contribute to the manifestations.
2. Stress incontinence or effort incontinence. It is often caused by weakened pelvic muscles, sphincter weakness, or problems with the urethra. All these reasons allow urine to leak out when intra-abdominal pressure increases (when sneezing, coughing, laughing, lifting weights, etc.). The most common factor of stress urinary incontinence in women is damage to the muscles of the pelvic diaphragm during pregnancy and childbirth; in men – prostate surgery.
How much can OAB therapy cost in Germany?
When you contact the Nordwest clinic, you receive a detailed information about how much it will cost to treat and rehabilitate an overactive bladder in Germany . We have a clear calculation system, so the total cost of therapy is constant. Your benefits when contacting us:
- fair prices;
- professional consultation and guidance from doctors with the possibility of checking the diagnosis by a second specialist; full support of the patient on all issues of recovery and prevention of the underlying disease;
- full support of the patient on all issues of recovery and prevention of the underlying disease.
Pediatric urology PEDUROLOGY.RU
Urinary disorders, manifested by frequent urination, urinary incontinence, including urgency, are common complaints in childhood. However, parents usually pay attention to these symptoms in children over 4-5 years old, considering such manifestations to be a feature of younger age. But that's not true.
Not only the problem of social maladaptation of a child with “wet panties” syndrome, but also severe infectious complications from the urinary system, as well as vesicoureteral reflux, which may accompany this condition, determine the relevance of the problem. Due to the fact that not only highly specialized specialists (urologists), but also general practitioners are involved in the process of diagnosing and treating urinary disorders, in 1997 P. Abrams and A. J. Wein introduced the term “Overactive Bladder” to facilitate diagnosis and treatment.
Bladder overactivity is a symptom complex characterized by 1) pollakiuria (frequent urination > 8 times during the day); 2) urgency (an unexpected irresistible (imperative) urge to urinate; 3) urgent urinary incontinence (an episode of involuntary loss of urine immediately following an episode of urgency); 4) enuresis (bedwetting); Pollakiuria is combined with a decrease in the effective volume of the bladder below standard values. The most important sign of pollakiuria, as a pathological symptom, is the absence of residual urine, which is established retrospectively during an instrumental examination (catheterization of the bladder or ultrasound examination after urination). Urgency is diagnosed when the patient complains of periodically appearing, irresistible desires to urinate. If a child cannot suppress the urge to urinate, urge urinary incontinence occurs. Enuresis is urinary incontinence at night. If all of the above symptoms are present, we can speak of a complete syndrome of urinary dysfunction.
AT WHAT AGE SHOULD OVERACTIVE BLADDER IN CHILDREN BE CONSIDERED A DISEASE? By the age of 4, most children develop a “mature type of urination”, characterized by: complete retention of urine day and night; · the ability to delay and interrupt, if necessary, the act of urination; · the ability to empty the bladder without a previous urge to urinate; · behavioral reactions accompanying the act of urination - the desire for privacy when the urge appears, etc. Normally, children 3-4 years old empty their bladder 5-8 times while awake; The average effective bladder volume ranges from 120 to 150 ml.
The volume of urination can be calculated using the formula: (30xage) +30 ml. Thus, we can talk about the formation of an OAB symptom complex in cases where in a child 4 years of age and older, the number of urinations and the effective volume of the bladder go beyond the normative indicators, and urination is uncontrollable to one degree or another. However, we must not forget that pathology begins at an early age, and therefore it is very important to know, even in children in the first months of life, how often the child urinates, what the portions of urine are (in infants, the study should be carried out according to international standards within 4 hours). The diagnosis of OAB is established using a comprehensive staged examination, including at the prehospital stage: -physical examination; -laboratory tests; -keeping a diary of urination and bowel movements. At the first stage of the examination, the child should be examined by a psychoneurologist, since even during the initial examination behavioral problems, hyperactivity and attention deficit syndrome, and delayed psychomotor development can be identified. During a physical examination, the lumbosacral spine is examined to identify malformations and phenomena of spinal dysmorphism: (hyperpigmentation, subcutaneous lipoma, buttock asymmetry, hypertrichosis), which is an indication for R-graphy of the lumbosacral spine or MRI, which will reveal bone markers of myelodysplasia, the presence of additional formations and will allow assessing the state of liquorodynamics. When collecting anamnesis, it is necessary to determine the presence of constipation and/or stool. It is mandatory to study perineal sensitivity and reflexes, as well as the tone of the anal sphincter. When examining the lower extremities, it is necessary to pay attention to the symmetry of the extremities and gait. An examination of the external genitalia is carried out to identify concomitant pathologies: cicatricial phimosis, epispadias, meatal stenosis, vulvitis, vaginitis. It is fundamentally important to confirm or exclude the presence of infectious complications. Clinical laboratory tests (general blood count, general urinalysis), microbiological research methods (bacteriological culture of urine to determine the sensitivity of microorganisms to antibacterial drugs) are mandatory. A method for identifying an overactive bladder at the first stage of the examination is keeping a diary of urination and defecation, since The pelvic organs are innervated by the same nerve structures, and these disorders are often combined. According to the terminology of the International Society for Urinary Continence in Children, a “urination and defecation diary” involves recording the number of urinations, the time of onset of the urge, the volume of urine excreted per urination, symptoms of incontinence and urgency, urine production at night, taking into account the volume of fluid taken and recording acts of defecation . Urination diary Frequency of urination: ─ increased (> 7/day) ─ decreased (< 3/day) Volume of urine excreted: ─ portions Volume of fluid taken ─ N = 25-30 ml/kg/day (for diabetes 75-100 ml/kg day) ─ distribution over time Cases of urinary incontinence: ─ frequency ─ intensity Urgency: yes/no Constipation/stooling: yes/no The study should be carried out within 14 days, or at least within 4-5 days, determining the time and volume of urination. In infants, a 4-hour test is performed with ultrasound monitoring of bladder filling and mandatory recording of the volume of residual urine after each urination. Urine portions can also be determined by weighing diapers. The absence of changes in urine tests in the presence of pollakiuria should alert the doctor, and changes in the nature of urination are indications for further examination and treatment. Data on the nature of urination, assessed by the rhythm of urination, are analyzed using a table for assessing urinary urgency syndrome proposed by E.L. Vishnevsky in 1997, in which the main symptoms of urination disorders are assessed by a certain number of points, depending on the severity of the disorders. Urinary Urgency Assessment Chart.
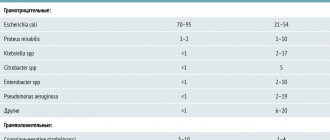
| sign | state | points |
| Urinary urgency | No Not every day Every day 1-2 times Every day several times | 01 2 3 |
| Urgent incontinence | No Not every day Every day 1-2 times Every day several times | 0 1 2 3 |
| Involuntary urination during night sleep (enuresis) | No Not every day Several times a month Several times a week Every night 1 time Every night several times | 0 1 5 10 15 20 |
| Diuresis from 18 to 6 hours (in relation to daily) | Up to 40% 41-50% 51-60% 61-70% More than 71% | 0 1 2 3 4 |
| leukocyturia | No In urine analysis according to Nechiporenko In general urine analysis | 0 1 2 |
| Sign | Number of urinations per day | points |
| Urination rhythm | 5-8 9-10 11-12 13-14 15-16 17-18 19-20 20 or more | 0 1 2 3 4 5 6 7 |
Depending on the severity of urination disorders, 3 groups are distinguished: Group 1 - mild degree of urination disorders, total score 2-10. Group 2 - average degree of disorder, total score 11-20. Group 3 - severe urinary disorders, total score 21-30. Considering the high incidence and infectious complications and the development of vesicoureteral reflux with an overactive bladder, the damaging effect on the renal parenchyma and, as a consequence, the development of renal failure, a multidisciplinary approach to treatment tactics is necessary. Since the nature of OAB is polyetiological, treatment should be comprehensive, not symptomatic and aimed at restoring the act of urination as a whole.
Treatment of childhood enuresis.
The main methods of treatment are urotherapy, pharmacotherapy and isotherapy. The starting method in the treatment of OAB is urotherapy – a system of cognitive methods. Urotherapy means the elimination of behavioral disorders in a child, cognitive correlation, urination training in combination with the principle of biofeedback. The next stage of pathogenetically based treatment of OAB is pharmacotherapy (use, in particular, oxybutynin). But in children under 5 years of age, M-anticholinergics are not approved for use (and it is at this age that urinary disorders begin), and, in addition, 17-30% of children have intolerance to oxybutynin. Therefore, physiotherapy is of great importance in the treatment of OAB, both in the form of monotherapy (in children under 5 years of age) and in combination with pharmacotherapy. It is recommended to use thermal procedures (in particular ozokerite applications), sinusoidally simulated currents, as well as the use of modern types of energy (interference currents and laser therapy).
If you would like more information, please contact us or consult your doctor for specific diagnostic and treatment recommendations.
For many questions, an online consultation with a urologist is possible - https://pedurology.ru/index.php/on-line1
What is overactive bladder (OAB)?
This is a condition characterized by a strong, irresistible sudden urge to urinate, which may be accompanied by involuntary leakage of urine. Typically, these urges are accompanied by frequent daytime and nighttime urination.
What causes OAB?
The exact cause of OAB is not completely clear. However, factors leading to the development of OAB include: taking certain medications, neurological diseases (Parkinson's disease, multiple sclerosis, stroke). Some diseases are accompanied by similar symptoms: bladder cancer, urinary tract infections, BPH. These conditions must be excluded when making a diagnosis of OAB.
Observations have shown that some people are predisposed to the development of OAB: those suffering from depression, anxiety, and attention deficit disorder.
Symptoms and clinical course of overactive bladder in women
I.V. Kuzmin, N.O. Krotov FSBEI HE “First St. Petersburg State Medical University named after. acad. I.P. Pavlova" of the Ministry of Health of the Russian Federation (St. Petersburg)
Introduction. According to the ICS Standards Committee, the term “overactive bladder” (OAB), or “overactive bladder syndrome,” refers to a symptom complex manifested by urinary urgency with or without urge urinary incontinence and usually accompanied by urinary frequency and nocturia.
The incidence of OAB is high and reaches 10–15% among all adults. Over the past decades, a significant number of studies have been conducted on various aspects of the pathogenesis, clinical course and treatment of OAB.
The purpose of this study was to study the characteristics of the symptoms and clinical course of OAB in women, to identify the relationship between the severity of symptoms and the age of patients and the presence of concomitant diseases.
Patients and research methods. A survey of 347 women with symptoms of OAB aged from 18 to 81 years was conducted. The average age of the patients was 53.5 ± 0.7 years. OAB was diagnosed according to the ICS Standards Committee criteria. Before inclusion in the study, all patients underwent a comprehensive urological examination to exclude any diseases other than OAB that could affect the function of the lower urinary tract. The severity of OAB symptoms was assessed using urination diaries, which patients filled out over three days.
Results. Studies have shown that in the vast majority of women, OAB can be considered an acquired disease. Only 33 (9.5%) women had been bothered by OAB symptoms since childhood. Moreover, the average age of onset of OAB symptoms was 47.1 ± 0.9 years. The peak incidence of OAB occurred in the age period from 40 to 49 years.
Clinical manifestations of OAB include increased frequency of urination and urgency with or without urge urinary incontinence. When surveying women with OAB, many noted that a strong urge to urinate, which in some patients leads to urinary incontinence, could be provoked by certain actions of the patient himself or by some external factors. Most often, patients indicated the urge to urinate when the body cooled, for example, when leaving a warm room into the cold (57%). Next in descending order of frequency of responses were the sound of running water (41%), approaching the house or any related actions, for example, taking the elevator (29%), emotional stress (18%). When analyzing data from urinary diaries, it was found that the severity of most OAB symptoms is closely related to age. A positive correlation with age was observed for the frequency of nighttime urination (r = 0.19; p = 0.001), frequency of urgency (r = 0.17; p = 0.003) and frequency of urge urinary incontinence (r = 0.21; p < 0.001). Intestinal dysfunction had a significant impact on the severity of OAB symptoms in women. This is evidenced by a statistically significant correlation between the presence of constipation and the frequency of urgency (r = 0.29; p = 0.002) and urge urinary incontinence (r = 0.18; p = 0.049). An analysis of the relationship between the frequency of the main symptoms of OAB and the most significant factors in women’s medical history was carried out. The results of this analysis did not allow us to identify reliable connections between the severity of OAB symptoms and the number of pregnancies and births, the presence of any gynecological diseases, in particular uterine fibroids, as well as surgical interventions on the pelvic organs.
A study was conducted of the relationship between the main symptoms of OAB in women. Of all the symptoms, only the frequency of imperative urges showed a significant positive correlation with the severity of the other two symptoms, while no correlation was found between the frequency of urination and the frequency of urgent urinary incontinence. Thus, an analysis of the connections between OAB symptoms in women led to the conclusion that urinary urgency is a kind of “connecting” symptom of OAB, which makes it possible to identify them as the most important clinical manifestation of OAB.
Conclusion. The severity of OAB symptoms in women is related to age and bowel function. Among the symptoms of OAB, the leading role is played by imperative urges, the severity of which determines the intensity of the other two main symptoms of OAB - pollakiuria and urge urinary incontinence.
Topics and tags
Urinary incontinence
Overactive bladder
Magazine
Urological bulletins 2021 No. 1 - Special issue
Comments
To post comments you must log in or register