What do kidneys do and why are they needed?
Normally, a person has a pair of kidneys, which are located at the posterior wall of the abdominal cavity (retroperitoneal) on either side of the spine at the level of the lumbar vertebrae. They are very small - each weighs only 0.5% of the total body weight. But their proper functioning, general health, is very important for the body.
The kidneys remove from the body the final metabolic products that are formed as a result of metabolism: excess water, carbon dioxide, salts, ammonia, and some incompletely oxidized breakdown products (urea). The activity of the kidneys helps maintain the constancy of the osmotic pressure of cells and the stability of the acid-base balance of the whole organism. In addition, the kidneys remove harmful and toxic substances that enter the portal vein from the intestines (indole, phenol, skatole, arsenic, mercury compounds, etc.), which are neutralized by the liver. The kidneys are organs that not only remove unnecessary and harmful substances from the body, but also participate in the formation of certain substances (incretory function), such as vitamin D3, biologically active substances involved in the regulation of blood pressure (renin-angiotensin), circulating blood volume ( erythropoietin), etc.
Blood enters the kidneys through the renal arteries and flows out of them through the renal veins, which empty into the inferior vena cava. The urine formed in the kidneys, due to the processes of filtration and reabsorption, flows through two ureters into the bladder, where it accumulates until the moment of urination.
The main structural and functional unit of the kidney is the nephron (glomerulus, Shumlyansky-Bowman capsule, descending tubule, loop of Henle, ascending tubule, collecting duct) with its blood vessels. The average human kidney contains about a million nephrons, each about 3 cm long, creating a huge surface area for metabolism.
Congenital kidney diseases
In recent years, parents and doctors have been concerned - the number of children with congenital and hereditary kidney diseases has increased, often complicated by the layering of infectious and inflammatory processes in the organs of the urinary system (UC) and being the most common cause of the development of such a serious complication as chronic renal failure (CRF) in childhood.
The excretory system begins to develop from the 3rd week of pregnancy. The kidneys begin to function around the ninth week of the baby's intrauterine life. Nephrons - the structural units of the kidneys develop from 20-22 weeks. They, like all organs of the genitourinary system, are very sensitive to various kinds of damaging (teratogenic) factors. The first 2-3 months of pregnancy are considered the most dangerous in terms of the development of congenital kidney diseases, and the earlier the teratogenic effect was, the more severe the developmental defects will be, possibly incompatible with life. If a harmful factor acts at 3-4 weeks of pregnancy, then the fetus may not develop kidneys (renal agenesis); if the exposure occurred at 14-15 weeks of intrauterine development, then one can expect a violation of the structure, shape and number of elements of the renal pyelocaliceal system, but at the same time, in general, the genitourinary system will be formed.
Causes of kidney disease in children
Congenital diseases of the urinary system are those diseases that exist from the birth of a child and are the result of disruption of the development processes of the embryo. In addition, this group of diseases also includes congenital disorders of the membrane transport of various substances in the renal tubules. There are congenital nephropathies (diseases of the kidney itself) and uropathy (damage to the urinary tract).
By their origin, congenital kidney diseases can be acquired in nature (developmental defects resulting from the influence of harmful factors directly on the developing embryo without damage to hereditary structures). Violations of fetal development are provoked by unhealthy environmental conditions: radiation, excessive gas pollution, etc. Unfortunately, not all expectant mothers still understand the destructive consequences of smoking, alcoholism and drug addiction on the health of the baby. The occurrence of abnormalities in the development of the kidneys and other genitourinary organs is influenced by hormonal disorders and various infectious diseases of the pelvic organs suffered by a woman at different stages of pregnancy. Doctors note a high risk of developmental disorders in the fetus in expectant mothers who have had colds in early pregnancy, accompanied by high fever (38°C and above). A pregnant woman needs to remember that it is unacceptable to use medications without consulting a doctor who is not convinced of the safety of the medicine for the unborn baby.
The second large group of congenital kidney diseases is based on hereditary pathology (as a result of mutations of genes or chromosomes).
Let's consider anatomical anomalies of the organs of the urinary system of an acquired nature.
Nephrologists have proposed the following classification of congenital nephropathies and uropathy with anatomical anomalies of the urinary system (according to M. S. Ignatova and A. V. Papayan):
- anatomical abnormalities of the kidneys:
- quantitative (agenesis - absence of an organ, aplasia - underdevelopment of an organ and its functions, additional kidneys);
- positional (dystopia - incorrect position of an organ in space, nephroptosis - prolapse of the kidneys, rotation - rotation of an organ in space);
- shape anomalies (horseshoe-shaped, S-, L-shaped kidneys);
- anomalies of the pyelocaliceal system (megacalycosis - an increase in the volume of the renal calyces, calyceal diverticulum - a congenital protrusion of the wall of the renal calyces in the shape of a bag);
- ureteral abnormalities:
- quantity anomalies (agenesis, doubling);
- positional anomalies (ectopia - a developmental anomaly in which the mouth of the ureter is located not in the bladder, but in the urethra/vagina/on the surface of the skin of the perineum, retrocaval ureter
- location of the ureter behind the inferior vena cava);
- anomalies of structure and shape (hydroureter - accumulation of fluid in the dilated ureter due to the presence of obstacles impeding the outflow of urine, diverticulum
- congenital bladder wall in the form of a bag, dilatation
- abnormal expansion of the organ lumen);
- quantity anomalies (agenesis, doubling);
- anomalies of position (exstrophy - the absence of the lower part of the anterior abdominal wall and the body of the bladder, and the defect of the abdominal wall is replaced by the posterior wall of the bladder (the area of the vesical triangle) with gaping ureteral openings on it);
- anomalies of structure and shape (diverticulum, megacystis - an excessively enlarged bladder; usually combined with hypertrophy of its walls, persistent urachus
- cleft urachus (umbilical sinus)
- intrauterine urinary duct in the navel area);
- quantity anomalies (agenesis, doubling);
- positional anomalies (urethral valve, hypospadias - absence of the final part of the male urethra with the localization of its external opening in an unusual place, epispadias
- complete or partial obstruction of the anterior wall of the urethra);
- arterial abnormalities;
- vein abnormalities;
- arteriovenous fistulas;
- abnormalities of lymphatic vessels;
- abnormal development of the penis;
- abnormalities of testicular development;
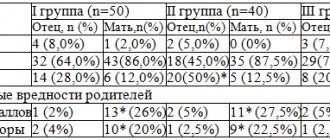
An anomaly of kidney development is any congenital defect of an organ that affects the structure, location, number, size of the kidney, developing in the embryonic period. The development of anomalies is influenced by a sufficient number of factors, namely: smoking, drinking alcohol, extragenital pathology and maternal heredity, ionizing radiation, infectious component, Rh conflict and many others.
All kidney anomalies are divided into the following subtypes: structural anomalies; location anomalies; quantity anomalies; size anomalies.
Abnormalities of kidney structure: Dysplasia is a malformation of kidney tissue, a decrease in kidney size, and impaired function. Anomalies of the cups can manifest themselves in the following form: - spongy kidney: with this pathology, many pseudocysts are observed in the dilated straight tubules of the renal nephron. It is benign and occurs more often in males; underdevelopment of the renal pyramids and an increase in the size of the proximal parts of the renal calyces. Urodynamics are not affected.
Anomalies in the location of the kidneys:
In its embryonic development, the kidney goes through several stages, and in one of them, the organ moves from the place of origin - the pelvic region - to the lumbar region. Dystopia is any change in the position of the kidney.
Quantity anomalies
1) kidney aplasia is the absence of one or two kidneys;
2) kidney doubling - happens on both the right and left sides. Duplication of the kidney can be complete - characterized by the presence of all structures of the kidney: ureter, pyelocaliceal system, and incomplete - there is no pyelocaliceal system;
3) accessory kidney.
Kidney size abnormalities
— Hypoplasia is a congenital decrease in the size of an organ while maintaining the excretory function.
— Horseshoe kidney – fusion of two kidneys in the form of a horseshoe.
— Biscuit-shaped kidney - fusion of two internal surfaces of the kidneys and a change in their location.
- L and S-shaped kidney - in the first case, the kidneys grow together with opposite edges and are located on one side of the spine, in the second - one kidney lies along the spinal column in its usual place, and the second is perpendicular to it.
Diagnosis of anomalies
Often, any congenital kidney anomaly is an accidental finding, since it does not have specific symptoms. The anomaly can be determined by referral to additional research methods, when at an appointment with a urologist the patient complains about the functioning of the urinary system.
Research methods used
- X-ray with contrast.
- Ultrasound with Dopplerography.
- Cystoscopy.
Treatment
Depending on the pathology, treatment varies greatly. A urologist will help you understand the causes of your complaints and solve any difficulties that arise. Types of treatment that are most often used:
- Renal cyst puncture;
- Laparotomy operations;
- Symptomatic treatment.
Inattention and negligent attitude towards one’s own health can be costly, both literally and figuratively, and timely treatment prescribed by a competent specialist will preserve health, a high quality of life, and often life itself. If you have problems with your kidneys, dispel your doubts - go to the page where you can consult a doctor by asking a question. Be healthy!
Urologist-andrologist
Klimenko Konstantin Vladimirovich
Diagnosis of kidney abnormalities
Modern diagnostic technology allows early detection of kidney development abnormalities.
Echography (ultrasound) allows you to diagnose congenital kidney malformations from the middle of the second trimester of pregnancy. Intrauterine diagnosis is possible starting from the 20th week of pregnancy and earlier. Ultrasound specialists also pay attention to the condition of the amniotic fluid, because low and polyhydramnios can be diagnostic signs of any disease, incl. and kidneys. I would like to draw your attention to the fact that if any pathology is detected in the fetus, the expectant mother should not be left alone with this problem, worry and accumulate feelings of guilt, she must contact a family psychologist. It should be added that in some cases, diagnoses made in utero are not confirmed.
When children are born with congenital kidney diseases, excretory urography and nephroscintiography are also used to make a diagnosis - research methods that make it possible to determine the anatomical and topographical features of the kidneys with the introduction of a contrast agent and renal angiography - a method that allows you to identify the presence and characteristics of the blood flow of the kidney.
Renal functions are also examined (biochemical tests of blood, urine, urine analysis according to Zimnitsky, etc.)
Advertising
Features of the treatment of kidney diseases in children with anomalies
In case of anomalies in the number of kidneys, with the exception of agenesis (underdevelopment of the organ), the outcome of which is unfavorable, symptomatic treatment, diet selection and active therapy for possible inflammatory diseases are carried out, since with kidney anomalies conditions are often created for obstructive disorders, reflux (reverse reflux of urine from the bladder into the kidney), urinary tract infections. This form of anomaly is often complicated by renal arterial hypertension, for which lifelong antihypertensive therapy is prescribed. In case of severe dysfunction of the organ, kidney transplantation is possible.
Abnormalities in the position of the kidneys (positional) are more common. Such children are registered at the dispensary, they are prescribed courses of massage and wearing bandages (according to indications) and prevention of complications such as hydronephrosis and urolithiasis (KD), and if persistent pain occurs, surgical treatment is used.
Anomalies of shape (fusion) occur in 15-20% of all honorary anomalies. There are symmetrical (horseshoe-shaped) and asymmetrical (S- and L-shaped fusions). Treatment is conservative and observation. Surgical interventions are performed in case of severe hydronephrosis (obstruction of the urethral segment), severe pain syndrome, with the development of urolithiasis, tumors.
With anomalies of the pyelocaliceal system, renal function is not impaired. These anomalies do not require special treatment, unless they are complicated by some pathological process, usually nephrolithiasis (NPD).
Anomalies in the development of the ureters are the main element of the anomaly of the kidney itself. Treatment is only surgical.
Anomalies of bladder development are more common in boys. Agenesis (underdevelopment) of the bladder is an extremely rare disease, often combined with other defects of the urinary system. Children with this pathology are not viable.
The most important direction of modern pediatric urology is the correction of congenital anomalies of the genitourinary system, primarily congenital defects in the development of the urethra and bladder. And if a couple of decades ago these defects required long-term multi-stage treatment, today urologists are increasingly striving to operate on such children in one stage. Of these anomalies of the genitourinary system, first of all, it is worth noting such congenital diseases as hypospadias (underdevelopment of the final part of the urethra and epispadias (partial or complete splitting of the anterior wall of the urethra), as being of great importance for the full development of the child. Treatment of this pathology requires various plastic surgeries.In these surgeries, replacement tissue is taken from the smallest patient.
I would like to dwell on one of the most common complications of congenital anomalies of the urinary tract (in the ureteropelvic segment) - hydronephrosis in children, since its frequency is 3 cases per 1000 newborns. Hydronephrosis of the kidneys is an increasing expansion of the renal calyces and pelvis with atrophy of the renal parenchyma (kidney lining), caused by a chronic violation of the outflow of urine from the kidney. The development of hydronephrosis is caused by any process (both in the urinary system and outside it - stones, tumors, etc.) that causes an obstruction to the outflow of urine. As a result of increasing intrapelvic pressure, atrophy (a decrease in the mass and volume of the kidneys, accompanied by a weakening/cessation of their function) of the renal parenchyma and muscle fibers of the wall of the urinary tract occurs and kidney function decreases. However, in our country there is a well-established diagnostic system using the screening method - ultrasound (sensitivity of the method is 65-98%), incl. and in utero. Dynamic monitoring of children who were diagnosed with hydronephrosis before birth is necessary, because in 10% of these babies this diagnosis is not confirmed in the first days of life. If the disease develops at an older age, then one of its symptoms is the presence of a tumor-like formation in the baby’s abdomen, usually detected by parents when bathing the child. Early detected hydronephrosis determines the success of surgical treatment and the preservation of kidney function. Over the past 5 years, a lot of research has been carried out, and vast positive experience has been accumulated in performing ureteroplasty operations in children, optimal methods of postoperative drainage of the urinary tract, etc. have been found, which leads to good treatment results.
An equally important congenital anomaly is anomalies of the bladder. In this case, exstrophy of the bladder deserves special attention. In this case, there is an absence of the anterior wall of the bladder, as well as the corresponding part of the abdominal wall. Treatment of such an anomaly also involves performing plastic corrective surgeries that correct the congenital defect.
Advertising
Anomalies of the relationship (fusion) of the kidneys
Renal fusion is an anomaly characterized by the fusion of two kidneys into one organ, the ureters of which end in the bladder at the usual places. The most characteristic signs of this anomaly are the incorrect position of one or both kidneys in relation to each other and their fusion with each other. Fusion can occur symmetrically with the upper or lower poles (horseshoe kidney), as well as the middle parts or asymmetrically, when the lower pole of one kidney fuses with the upper pole of a vertically rotated (S-shaped kidney) or horizontally located (L-shaped kidney) other kidney. Sometimes both kidneys are completely fused and have a biscuit-like shape or are a formation that does not have a specific shape. Confused kidneys account for 14% of all renal anomalies.
The most common type is the horseshoe kidney. Fusion of the lower poles is observed in more than 90% of all cases of horseshoe kidneys. The isthmus, which connects the poles of both kidneys, consists of renal parenchyma or dense fibrous tissue. The horseshoe kidney is found in a ratio of 1:425 autopsies. A horseshoe bud often consists of symmetrical buds of equal size. In some cases, one or both kidneys can be doubled, and then the kidney becomes asymmetrical.
The horseshoe kidney is formed as a result of the fusion of two nephrogenic blastemas during the embryonic period. Usually the horseshoe kidney is dystopic. In most cases, the isthmus is located at the level of the IV or V lumbar vertebra. The longitudinal axes of each half of the kidney form an angle, open upward. The pelvis faces anteriorly or medially. In some cases, they may be laterally facing and distant from each other. The cups are located atypically depending on the degree of rotation of the kidney, often have! spherical shape. Their necks can be dilated even without being visible! obstructions to the outflow of urine. The isthmus of the kidney is usually located in front of the large vessels (aorta, inferior vena cava, common iliac vessels) and the solar plexus, which are pressed against the spinal column by the isthmus. In 6-10% of cases, the isthmus of the horseshoe kidney is located between the aorta and the inferior vena cava and, extremely rarely, between the spinal column and the vessels. The isthmus seems to bring the kidneys together. Therefore, each half of a horseshoe kidney lies closer to the spinal column than normal kidneys. There are often two prominent grooves on the anterior surface of the isthmus that separate the isthmus from the underlying renal parenchyma. The ureters pass through these grooves or depressions. Sometimes these grooves are absent and the isthmus passes into the main parenchyma of the kidney without any boundaries. Rarely there is a median groove dividing the isthmus into two parts. The size of the isthmus can be very different. Its thickness most often ranges from 1.5-3 cm, width - 2-3 cm. The length of the isthmus is 4-8 cm.
Histological examination reveals renal tissue in the isthmus with varying degrees of dysplasia, with more or less fibrous tissue. More often, the isthmus consists of the normal parenchyma of one of the kidneys. In such cases, it is well supplied with blood. In the thickness of the isthmus there may be one or several lower cups. When one of the halves of a horseshoe kidney is doubled, the pelvis of the lower half of the doubled kidney can pass through at the level of the isthmus. The shape of each half of the horseshoe bud is significantly modified. In most cases, the kidneys retain embryonic lobulation. In rare cases, their surface is smooth. Both halves of the horseshoe bud can be elongated, spherical or disc-shaped. The hilum of the kidney is located on its anterior surface. Sometimes the renal hilum is separated by a parenchymal cord. In such cases, the cups of each kidney unite and become two separate sinuses. The pelvis lies directly on the kidney in the area of its hilum.
Sometimes the pelvis (or two pelvises) is located intrarenally, and the ureter perforates the parenchyma in an anterior direction. Observations are described when the pelvis was completely absent. In such cases, the cups are connected separately to the ureter. In addition, the isthmus of a horseshoe kidney may have not only one or two accessory ureters, but also its own pelvis. Such extreme forms of the extrarenal pelvis of the horseshoe kidney have also been described, when the kidney has neither a sinus nor a hilum. The cups then extend straight away from the renal surface. Each cup begins from a depression in the parenchyma or is superimposed on the papilla, which protrudes above the surface of the kidney.* N. L. Kush and co-authors (1978) during surgery found adhesions in children in the isthmus of the horseshoe kidney, which, in their opinion, are the result of mild injury to the isthmus of the kidney. Spikes can be single or multiple. They often involve the pelvis and the initial sections of the ureters. As a result of these changes, the outflow of urine from the horseshoe kidney is disrupted. The ureter usually extends from the pelvis higher than normal. It runs forward and downward, crosses the isthmus, or may lie directly on the anteromedial surfaces of both halves of the horseshoe kidney. Variants of the location of the ureter behind the isthmus on one or both sides are described.
The literature contains observations when the right pelvis was intraisthmic, and its ureter, emerging from the isthmus, was located between the inferior vena cava and the aorta. In some cases, the horseshoe kidney had a single ureter that emerged from its isthmus. During the operation, this feature must be taken into account. The surgeon must verify the existence of a second ureter on the opposite side before heminephrectomy.
Most variants of the horseshoe kidney are characterized by a certain position of the ureters. Initially, they are directed inward and anteriorly, spreading over the isthmus or lower poles of the kidneys, then they descend posteriorly and outward, describe a characteristic curve and are located much closer to the spinal column than the ureters of normal kidneys.
Duplication of the pelvis and ureters of fused kidneys occurs with almost the same frequency as duplication of the pelvis of correctly located kidneys. Duplicate ureters can merge into one before emptying into the bladder or open with separate openings. In rare cases, ectopia of one of the openings of the ureters of a horseshoe kidney occurs. The anatomical features of the ureter (its high location relative to the pelvis and bending above the isthmus) predispose to functional obstruction and impaired urodynamics. E. M. Shimkus, S. E. Shimkus (1978) note that urodynamic disturbances in horseshoe kidneys begin to develop from the upper part of the ureter and pelvis. In this section, the ureter expands when it contracts. Its contractions are usually shallow and infrequent. Impaired urinary passage and the development of hydronephrosis can be facilitated by congenital narrowing of the pelvic region of one or both ureters of a horseshoe kidney, and insufficiently expressed fatty perirenal tissue.
In almost 60% of cases, a horseshoe kidney is combined with congenital defects of other organs. Each of the kidneys, fused by the same poles, has its own blood supply. There are many variations in such cases. More often there are 2-3 arteries, and sometimes 4 or 5. We observed a case where the left side of the fused kidneys had 5 arteries, the right - 6, and all of them originated from the aorta. The common iliac, inferior mesenteric, hypogastric arteries, and aorta are often involved in the vascularization of the horseshoe kidney. The more pronounced the dystopia of fused kidneys, the lower the level of discharge of the feeding vessels. Multiple vessels involved in the blood supply to fused kidneys form a plexus on the anterior surface of the kidney, fix the kidney and, in some cases, are an additional cause of impaired urine outflow from the pelvis. Feeding vessels that flow into the parenchyma of the horseshoe kidney in addition to the renal sinus are described. The vessels enter the renal tissue from the periphery of the organ, mainly in the region of the lower poles of the kidney. Before penetrating deep into the kidney, they form grooves on its surface. O. A. Wichert (1981), noting the high frequency of nephrogenic hypertension in fused kidneys, believes that it can be not only a consequence of associated pyelonephritis, but also a manifestation of the anomaly itself. Arterial nephrogenic hypertension can develop as a result of venous hypertension due to impaired venous outflow. Abnormal blood supply plays a certain role in the genesis of arterial hypertension.
Gobden et al (1978) described cases of the development of renovascular hypertension as a result of stenosis of one of the numerous arteries of the horseshoe kidney. In the origin of arterial hypertension with multiple arteries of fused kidneys, ischemia at the border of the segments, which is detected in the corresponding areas during angiographic studies of horseshoe-shaped kidneys (in the nephrogram phase), as well as the presence of areas of dysplasia of the renal tissue transformed into a scar, and limited areas of parenchyma wrinkling may play a role. (V.S. Karpenko, A.S. Pereverzev, 1977; M. Robertson et al., 1967).
Often a healthy horseshoe kidney does not manifest itself clinically, but it is much more likely than a normal kidney to be affected by various diseases. According to I.I. Akhundov, V.V. Bryushkov (1966), various diseases occur in 86% of cases with a horseshoe kidney. Nephrolithiasis occupies a significant place among diseases of the abnormal kidney (52.4%).
Due to the characteristics of the blood supply, innervation and pressure of the isthmus on the nerve plexuses, even with a healthy horseshoe kidney, a characteristic pain symptom complex may occur. An abnormal kidney is often accompanied by pain in the navel area during straightening of the body or bending backwards. This symptom complex is called symptom I. Rov-sing. The pain is usually dull and may be intermittent or constant. Compression of the aorta is rarely observed, but if it occurs, it is accompanied by symptoms of coarctation of the aorta.
Compression of the inferior vena cava by the isthmus of the horseshoe kidney can lead to venous hypertension of the lower half of the body, subsequent dilatation and venous stagnation in this area. This in turn can cause swelling of the lower extremities and even ascites. Sometimes there is a feeling of numbness in the lower extremities.
Prevention of diseases of the urinary system
Congenital malformations of the urinary system occur in 6% of pathological studies of children under 1 year of age. Medical genetic counseling, prenatal diagnostics, preventive methods aimed at improving the health of the expectant mother herself make it possible in 50-70% of cases to prevent the birth of children with severe congenital and hereditary diseases, and in some forms - to carry out successful preventive treatment, and then in your home The long-awaited healthy baby will appear!
Remember that your baby's health is in your hands! Attentive parents themselves may suspect something is wrong. Here are a few symptoms to look out for to help identify kidney or urinary tract disease early and prevent serious complications from developing:
- Monitor the number of times you urinate and the volume of urine produced. During the first 1-3 days of life, a newborn baby urinates 3-5 times a day - this is a physiological transition state of the urinary system. From 4 days to 6 months, the frequency of urination reaches 20-25 times a day, after 6 months and up to 1 year - 10-14 times. By the age of 5, the number of urinations is reduced by 2 times. Frequent urination and the urge to urinate (without urination itself) is a reason to urgently consult a doctor. If the child urinates little and rarely or does not urinate at all (the volume of urine in the first 3 days of life is about 50-100 ml, up to 6 months - on average 180-190 ml, 6 months - up to 2 years - 230-300 ml, 3-4 years - about 400-500, from 5 to 7 - 500-700 ml, over 7 - 800-1000 ml), he has nocturia (the predominance of the amount of urine excreted at night over the daytime volume; normally the daytime is 2/ 3 total amount of urine per day), polyuria (increase in the volume of daily urine by more than 2 times), daytime or nighttime urinary incontinence (this applies to children over 3-4 years old) - contact a specialist!
- Pay attention to the color of the urine and its clarity. While the child is small, this is not difficult. Normally, the color of urine is light yellow; in the morning the urine is the richest. Cloudy urine, blood in the urine, etc. may be symptoms of serious illnesses.
- Examination of the external genitalia is of no small importance. In newborn boys, you need to pay attention to the location of the urethra. If the baby suddenly develops redness and swelling of the scrotum on one or both sides, during swaddling or when touching the scrotum, the child cries and becomes restless, do not hesitate and do not self-medicate, but urgently contact a pediatrician or pediatric urologist. In girls, you need to pay attention to the outer labia. There should be no swelling, redness, etc., there should be no discharge (physiological discharge from the genital tract is light, mucous is observed in girls during the newborn period, in infancy, they are caused by the presence of placental and maternal hormones in the girl’s body, in the future discharge will appear only at puberty). With adult children the situation is more complicated, but a child who grows up in an atmosphere of trust and care will definitely complain if something is wrong.
- Pay attention to unexpected weight gain in your baby or to pronounced and long-lasting “traces” from the elastic of panties or socks - this could be swelling.
- Pay attention to your child's complaints. Pain in the lower back, side, above the pubis, during urination, and in young children also abdominal pain, especially intense and recurring, should cause serious concern among parents.
- If a child becomes lethargic, pale, refuses to eat, his temperature rises to high levels (38-40°C), and at the same time, there are no visible manifestations of a cold, and antipyretic drugs give only a short-term effect - take a general urine test of your child. baby.
Svetlana Kirilina, PhD, pediatric nephrologist
Congenital defects of the kidneys, urinary tract and genital organs
Etiology. The development of defects is not associated with the action of certain exogenous agents. Many of them are hereditary or familial. Occurs in chromosomal syndromes. These defects are diverse and occur during the 4-8th week of cymatogenesis.
Congenital kidney defects. Renal agenesis - the congenital absence of one or both kidneys (arenia) - is rare, while the newborn has pronounced folding of the skin, a puffy, senile face, the ears are low, the nose is wide and flat, the frontal tubercles protrude; Congenital defects of other organs are also observed. Children are not viable.
Renal hypoplasia is a congenital decrease in their mass and volume, which can be unilateral or bilateral; with unilateral hypoplasia, vicarious hypertrophy of the second normal kidney is observed.
Renal dysplasia is hypoplasia with the simultaneous presence of embryonic tissue in the kidneys. Microscopically, foci of nephroblastoma, primitive tubules and glomeruli, cysts, islands of cartilage and smooth muscle tissue are found in the kidney tissue. Combined with aplasia, hypoplasia or atresia and ureteral stenosis. With bilateral pronounced hypoplasia and dysplasia of the kidneys, children are not viable.
Large cystic kidneys (polycystic kidneys of the adult type) - bilateral significant enlargement of the kidneys with the formation in their cortical layer of a large number of large cysts with transparent contents, between the cysts there are areas of normal renal tissue. The defect is combined with cysts of the liver and pancreas and is inherited in a dominant manner. Its pathogenesis is associated with a disruption in the connection of the rudiments of metanephrogenic tissue and the urethral tube, retention cysts are formed.
Small cystic kidneys (polycystic "infantile" type) - bilateral significant enlargement of the kidneys with the formation of numerous small cysts in the cortex and medulla, closely adjacent to each other. The buds have the appearance of a large-pored sponge. On microscopic examination, all renal tissue appears to be completely replaced by cysts lined with cuboidal epithelium. The defect is combined with liver cysts and hyperplasia of the bile ducts. Children are not viable.
Renal fusion (horseshoe kidney) and dystopia are not clinically evident.
Congenital malformations of the urinary tract. The main ones:
- duplication of the pelvis and ureter;
- agenesis, atresia, stenosis of the ureters, ectopia of their mouths;
- megaloureter refers to early fetopathies - a sharp expansion of the ureter (one or two) due to hypoplasia of muscle tissue or the nervous system;
- exstrophy of the bladder as a result of aplasia of its anterior wall, peritoneum and skin in the pubic area;
- bladder agenesis;
- atresia, urethral stenosis (more often in girls) and hypospadias - a defect in the lower wall, epispadias - a defect in the upper wall of the urethra in boys.
All defects of the urinary tract lead to impaired urine outflow and, without timely surgical treatment, which is currently successfully performed, lead to renal failure. The most severe of them (for example, agenesis, atresia of the urinary tract) lead to death from uremia soon after birth, others may not manifest themselves clinically for a long time, but gradually lead to hydronephrosis, sometimes to the formation of stones, and the occurrence of ascending chronic pyelonephritis, which threatens the development of renal failure , ending in the death of the patient (usually at 20-30 years old) from uremia.
Congenital malformations of the genital organs. They are often associated with disease of the endocrine glands (adrenal glands, pituitary gland) of the mother and fetus, with the use of hormonal drugs during pregnancy; hereditary transmission of a recessive type has been established. These include: cryptorchidism - retention of the testicles in the abdominal cavity or in the inguinal canal (in newborns should not be considered a defect, since cryptorchidism occurs in them in 30% of cases, by the age of 12-16 it is observed only in 2-3% of cases and then regarded as a vice); atresia of the cervix and vagina, duplication of the uterus; hermaphroditism - the presence of characteristics of both sexes in one person. A distinction is made between true hermaphroditism—the simultaneous presence of female and male gonads—and false hermaphroditism—the external genitalia of the sex opposite the gonads. Malformations of the genital organs are not life-threatening; in some cases, surgical treatment is possible.