CANDIDIASIS
(
candidosis
; synonym:
candidiasis, superficial blastomycosis, soormycosis, candidiasis, moniliasis, oidiomycosis
) is an infectious disease of the skin, mucous membranes and internal organs caused by yeast-like fungi (fungi of the genus Candida).
The disease was first described by B. Langenbeck in 1839, although it has been known since the time of Hippocrates under the names stomata aphtoides and aphta infantis (K. Galek). In 1848, F. Th. Berg first established the presence of yeast-like fungi in the tissues of a sick person. Berkhaut (M. Berkhaut) in 1923 identified the genus Candida among yeast-like fungi. The term Candida was adopted in 1939 by the III International Congress of Microbiologists.
Candidiasis occurs in all countries of the world, especially often in tropical and subtropical climates. The number of patients with various clinical forms of Candidiasis, especially visceral ones, has a slight upward trend.
Etiology
Rice.
1. Chlamydospores with a double-circuited shell and granular contents at the ends of the pseudomycelium (indicated by arrows). The causative agent of Candidiasis is most often Candida albicans, less often C. tropicalis, C. krusei, C. pseudotropicalis, C. stellatoidea and some other species. The genus Candida (class Fungi imperfecti) includes St. 80 species characterized by round, ovoid, less often cylindrical, and sometimes irregularly shaped cells. Young cells are from 2 to 5 microns in diameter, mature ones are slightly larger. Yeast-like fungi do not have true mycelium; they form chains (pseudomycelium) of elongated cells that touch each other with a narrow base (so-called constrictions), the length of the pseudomycelium is up to 12-16 µm. Cells reproduce by germination and multipolar budding (2-3 or more daughter buds). C. albicans and C. stellatoidea form spores with a dense, usually double cell wall—chlamydospores—at the ends of the pseudomycelium (Fig. 1).
Candida is aerobe; they are often saprophytes of the mucous membranes of the mouth, intestines, vagina, and skin. Found in soil, fruits and vegetables. For nutrition, they use proteins, peptones and amino acids from nitrogenous substances. Candida is considered an opportunistic pathogen; their pathogenicity for humans and animals largely depends on the state of the macroorganism (see below).
The most common for growing Candida (optimum temperature 30-37°) are Sabouraud's liquid medium, beer wort, and meat-extract glucose agar. For the detection of chlamydospores, the most suitable are Czapek-Doxa medium with the addition of Tween-80, potato agar with bile, corn and rice agar.
Candida remains viable in cultures (in a dried state) for several years and can withstand repeated freezing and thawing in water and soil. They compete with many microorganisms in terms of duration of existence on various products, for example. ' in sour milk, sauerkraut, fruit juices, etc. In crops and patol, the fungi die when boiled for a few minutes. 2-5% solutions of phenol and formalin, chloramine, Lysol, iodides, borates, copper and zinc sulfate, potassium permanganate and other chemicals have a destructive effect. substances; Solutions of aniline dyes (gentian violet, malachite green, methylene blue, etc.) have a fungicidal effect.
Myths and dangerous misconceptions in the treatment of candidiasis
Myth 1. Thrush is normal, everything will go away on its own. In fact, if the disease is not treated, it will become chronic and cause other health problems.
Myth 2. Thrush occurs only in sweet tooth lovers. Wrong, in fact it all depends on the immune system. Sweets are allowed, but in moderation.
Myth 3. Fermented milk products are the best prevention of thrush. Some girls even soak cotton pads in kefir and wipe problem areas. In fact, it is not worth wasting time on such folk remedies.
Myth 4. The disease can be treated with just 1 tablet. In fact, a comprehensive approach is required.
Epidemiology
The good adaptability of many species of the genus Candida to the environment ensures their widespread distribution, as well as carriage by humans and animals. For example, C. albicans can be found on the skin, mucous membranes and in the feces of up to 20% of healthy people. K. affects calves, lambs, foals, poultry, etc.; diseases and wild animals were noted. Some representatives of the genus Candida are associated with normal microflora of human skin (primarily C. albicans). As a source of infection, patients with fresh forms of lesions of the skin and mucous membranes are of greatest importance. Exogenous infection occurs through direct contact with a patient or a carrier of fungi (kiss, sexual contact, etc.) and through infected objects. Wastewater from baths, swimming pools and showers can, under unfavorable conditions, contribute to superficial foot disease. A warm and humid climate, especially the summer season, is important in the occurrence of K. Unfavorable working conditions (for example, a low level of technical equipment in confectionery and fruit-processing enterprises), violations of hygiene rules, both collective and personal, can even contribute to the occurrence of small outbreaks of superficial K. in maternity hospitals, nurseries, confectionery factories, etc. There are known cases of K. infection of newborns during the passage of the birth canal; very rare cases of congenital K. are described. Endogenous infection is associated with the activation of yeast-like fungi that are already present in the microbial associations of the body, therefore, in severe diseases (tuberculosis, pneumonia, diphtheria, malignant neoplasms, etc.) K. can occur as a concomitant disease.
Routes of infection
The amount of candida fungus can also increase upon contact with a previously infected person. For example, the causes of candidiasis in this case are as follows:
- during sexual contact (usually in this case the urogenital, vaginal or oral form develops);
- during pregnancy (in this case, the infection is transmitted from mother to child, and he/she develops symptoms of candidiasis at birth);
- during dental procedures (for example, prosthetics - in this case, an adult develops candidiasis in the mouth);
- injuries to the eyes, ears, skin (infection gets into the wounds).
Pathological anatomy
Rice.
2. Microslide of affected skin with superficial candidiasis: the germination of pseudomycelium (indicated by arrows) into the thickness of the necrotic epidermis is pronounced. Gram-Weigert stain; X 280. Fig. 3. Microspecimen of abscess granuloma (in the center of the preparation) in the depths of the dermis in case of chronic granulomatous candidiasis (biopsy). Staining with PAS method and hematoxylin. Cutaneous candidiasis manifests itself in the form of subacute dermatitis in skin folds, occasionally with the formation of abscesses and ulceration. When histol, the study notes intercellular edema of the epidermis, parakeratosis, acanthosis and germination of fungal filaments into the necrotic epidermis (Fig. 2). Inflammatory infiltration predominantly from segmented leukocytes is observed mainly in the dermis. Sometimes the formation of limited abscesses with the presence of disintegrating segmented leukocytes is observed. Subsequently, granulomas are formed, consisting of lymphocytes, epithelioid and giant lashes (Fig. 3).
When K. of the mucous membranes of the oral cavity and pharynx, superficial, easily removable whitish-yellowish films are found. Microscopically, they consist of pseudo-mycelium of the fungus, desquamated epithelium and a small number of segmented leukocytes. In more severe forms of infection, the fungus penetrates between the layers of the epithelium and parasitizes the cells. Their dystrophy and swelling, perivascular inflammatory infiltrates in the dermis are observed.
Visceral K. can be isolated (gastrointestinal tract, respiratory organs, genitourinary system) and generalized with single or multiple metastases in internal organs, nervous system, muscles, bones. Candidal esophagitis is often a consequence of the spread of the process from the mucous membrane of the oral cavity and pharynx; Three types of lesions are distinguished: 1) individual whitish plaques, consisting of desquamated epithelial cells, leukocytes and fungal threads, which are embedded between the cells of stratified squamous epithelium; 2) the formation of merging dense deposits and the introduction of fungus into the submucosal layer; 3) pseudomembranous deposits developing on the ulcerated mucous membrane; threads of the fungus not only penetrate the necrotic masses, but also penetrate deep into the muscular lining of the esophagus and grow into the vessels.
Damage to the stomach and intestines is observed less frequently, which is explained by the structural features of the glandular epithelium, which produces sialomucins, and, possibly, by the bactericidal properties of gastric juice (see). Usually K. of the stomach and intestines develops against the background of previous inflammatory, ulcerative, and atrophic changes. The more pronounced these changes were, the more severe the form K takes. In the mild form, the threads of the fungus only partially grow into epithelial cells and spread along the basement membrane, the inflammatory reaction is weakly expressed, mainly in the submucosal layer. In the severe form, necrosis of the mucous membrane is detected, threads of the fungus diffusely penetrate the necrotic masses and penetrate into the thickness of the wall of the stomach and intestines; this form may be accompanied by the formation of ulcers, which are sometimes complicated by bleeding or perforation with subsequent development of peritonitis.
K. of the mucous membranes of the respiratory tract is manifested by catarrhal-desquamative and diphtheritic inflammation. Candidal pneumonia (see Pneumomycosis) develops as a result of the spread of the process to the lung tissue along the respiratory tract due to aspiration of the fungus or by hematogenous route.
In the lungs, the early stage of inflammation caused by candida is characterized by exudate from segmented leukocytes mixed with fibrin. Subsequently, necrotic changes with passive fibrinous effusion in the lumen of the alveoli predominate. With hron, the form of K. of the lungs, multiple granulomas appear, consisting of lymphocytes, histiocytes and giant cells, in the cytoplasm of which phagocytosed elements of the fungal pseudomycelium are often found.
Isolated K. of the urinary tract often occurs as a result of an ascending infection; Urethritis and cystitis are observed, which sometimes lead to the development of pyelonephritis. In purulent-necrotic lesions, growths of pseudomycelium of the fungus and a phagocytic reaction are detected.
Generalized K. - single or multiple metastatic foci as a result of hematogenous spread of the fungus - can be of different localization. When the brain is damaged, extensive growth of pseudomysolium around the vessels is characteristic, which is associated with the characteristics of the chemical. composition of brain tissue favorable for fungal growth. Candidal meningitis has the character of acute limited or diffuse purulent or productive inflammation.
Rice. 4. Microscopic specimen of a metastatic kidney abscess: fungal cells (1) are surrounded by segmented leukocytes (2). Durable green finish. Rice. 5. Microscopic specimen of a metastatic liver abscess: in the center of the inflammatory infiltrate one can see an accumulation of vegetative forms of Candida (indicated by an arrow), which are surrounded by disintegrating leukocytes. Coloring according to Shabadash Fig. 6. Yeast-like fungal cells captured by macrophages and (indicated by an arrow). Azur-eosin staining.
Gistol, the picture of changes in metastatic foci of various organs and tissues does not have strictly defined specific features. In the initial stage of the candidiasis process, a necrotic-exudative inflammatory reaction is observed, often of a purulent nature, less often with a predominance of lymphocytes in the infiltrate. The intensity of fungal growth depends on the viability of the tissue: where necrosis is more pronounced, there are much more threads of fungus. When hron, the course of the process around the necrotic-exudative focus of inflammation, connective tissue grows or the formation of a granuloma is observed (see), reminiscent of that in tuberculosis (Fig. 3). The elimination of the fungus in the body occurs mainly due to the lysosomal enzymes of segmented leukocytes (Fig. 4), i.e., as a result of the so-called. extracellular phagocytosis, so the growth of the fungus in the purulent focus is usually inhibited. The presence of a large number of segmented leukocytes prevents the proliferation of the fungus; the leukocytes seem to stick around the elements of the fungus and, undergoing decay, delimit it from the surrounding tissue (Fig. 5). As electron microscopic studies show, in fungal cells the integrity of the cytoplasmic membrane is disrupted and autophagic vacuoles appear in the cytoplasm. Phagocytosis of fungi by segmented leukocytes is rare and mainly affects non-viable fungal cells; in the cytoplasm of macrophages (Fig. 6) and giant cells, the fungus can remain for a long time and be viable - the so-called. endocytobiosis. Since the fungus is capable of intracellular parasitism, the presence of its viable forms indicates that the inflammatory process is protracted.
In weakened, exhausted patients, inflammatory changes are extremely mild. This is especially noticeable if K. is accompanied by diseases of the hematopoietic organs, in particular agranulocytosis and radiation sickness.
The detection of candida on the surface of the skin, in the urethra, vagina and other mucous membranes should not always be regarded as a fungal disease. K. is characterized by the presence of vegetative forms of the fungus, the phenomena of budding, filamentation, as well as foci of tissue necrobiosis with an inflammatory reaction and phagocytosis of fungal particles.
Introduction
Over the past decades, nosocomial infections caused by pathogens with low pathogenicity potential have become increasingly important. This is due to the growing number of patients with multiple risk factors for developing diseases of this group. In most cases, infections caused by rare or opportunistic pathogens are detected in patients with immunodeficiency after organ transplantation and in cancer patients. Fungal microorganisms are the most common etiological causative agents of such infections [1].
An increase in the number of patients with fungal infections is also observed in urological practice. According to a large-scale study conducted in the USA, Richards MJ et al. From 1992 to 1998, among patients in intensive care units of surgical departments, urinary tract infections (UTIs) occurred in 95–97% of cases in the presence of an indwelling urethral catheter, while fungal pathogens were detected in 31% of patients.
Fungal UTIs are most often caused by representatives of the genus Candida, and can also be caused by Cryptococcus neoformans, Aspergillus and pathogens of endemic mycoses [2]. The source of funguria can be at any level of the urogenital tract (Table 1).
The most common location of the fungal process is the lower urinary tract. The occurrence of a fungal infection of the kidneys and genital organs is accompanied by a significant deterioration in the patient’s condition and requires the use of a longer and more intensive course of antifungal therapy.
It is important to note that funguria is not always accompanied by clinical manifestations [2]. Therefore, determining the localization of fungal UTI, despite the modern development of diagnostic technologies, remains a very difficult task.
Diagnosis of candiduria and candidiasis of the lower urinary tract
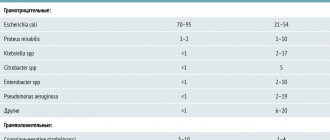
The most common causative agents of fungal UTIs are members of the genus Capdida. Currently, fungi of the genus Candida are detected in 80–94% of funguria cases [3]. The frequency of nosocomial infections caused by various species of Capdida has increased two to three times over the past 10 years [2]. The most common type of fungal UTI is Candida albicans (more than 50% of cases). Other varieties of Candida fungi are less common. Thus, C. glabrata is detected in 16–35% of cases, and C. tropicalis, C. krusei, and C. parapsilosis in 8–28% (Table 2) [2–6].
The detection of rare varieties of Candida is especially typical for inpatients with diabetes mellitus in the presence of a urethral catheter. Currently, candiduria is defined as the detection of fungal pathogens in a titer of more than 103 CFU/ml in two urine samples obtained at least 24 hours apart [2, 4, 6]. It should be noted that with fungal UTIs, candiduria is often combined with bacteriuria. In addition, there are known cases of detection of two species of Candida in urine at once [2, 3, 6]. Under normal conditions, Candida fungi can be found on the surface of the genitals and the skin of the perineum. Therefore, in most cases, candiduria is not accompanied by any symptoms and is associated with ascending colonization of the urinary tract through drainage (urethral catheters, cystostomy drains, etc.) or in women from the contaminated vulvovaginal area [2–4, 6–8]. Candiduria rarely occurs in the absence of predisposing factors or in healthy men. Thus, in patients with diabetes mellitus there is a high incidence of fungal infections of the lower urinary tract [2, 4, 6]. This is mainly due to a decrease in the phagocytic and fungicidal ability of neutrophils due to insulin deficiency [2, 6]. In women with diabetes, candiduria occurs more often than in men. This is due to the fact that women with diabetes have a more pronounced colonization of the vagina and periurethral area with Candida fungi [2, 6, 8]. Candiduria can develop in hospitalized patients already during the first two weeks of hospital treatment [2, 3, 5].
In addition to diabetes mellitus, the main predisposing factors for the development of candiduria include [2–7]:
- indwelling urinary catheters
- instrumental interventions
- anatomical and functional abnormalities of the urinary tract
- use of antibiotics, corticosteroids, immunosuppressants or cytostatics
- fungal infection of another location
- hemoblastosis with neutropenia
- elderly age
According to a number of studies, the occurrence of candiduria in most cases is preceded by antibacterial therapy [2, 4, 6, 7]. Although the occurrence of candiduria is possible with the use of any antibacterial drug, therapy with broad-spectrum drugs is associated with the highest risk of this complication, especially with a long course of treatment. Antibacterial therapy suppresses the endogenous bacterial flora in the gastrointestinal tract and leads to increased fungal colonization of epithelial surfaces, especially in the presence of a urethral catheter. That is why Candida fungi are a common cause of ascending infection in catheterized patients and patients with urinary tract obstruction [2, 5, 6].
In hospitalized patients, in 10% of cases, candiduria is the first clinical manifestation of disseminated candidiasis and candidemia [2, 4].
Most cases of renal candidiasis are caused by hematogenous dissemination of the pathogen into their parenchyma from other foci of infection, while disseminated candidiasis is an extremely severe disease, with a mortality rate of more than 50% [3, 9]. Thus, in patients with a high risk of developing candidiasis, including those with kidney damage, it is necessary to conduct a full clinical examination to identify the source of candiduria [2–4, 6, 9]. For the differential diagnosis of candidiasis of the upper and lower urinary tract, Fong IW et al. (1995) conducted a study of the effectiveness of a single instillation of amphotericin B solution into the bladder followed by urine culture. The persistence of candiduria in this case indicated candidiasis of the upper urinary tract or kidneys. Despite the high sensitivity and specificity of this method, reliable determination of renal candiduria was possible only in 44% of cases.
Patients with multiple risk factors for candiduria may develop clinical symptoms of UTI. In this case, candiduria is regarded as a manifestation of urinary tract candidiasis [3]. Lower urinary tract candidiasis is the most common type of fungal UTI. Immunosuppression and neutropenia are among the main risk factors for the development of lower urinary tract candidiasis [6, 9, 10]. A special role in protecting the body from candida infection is played by the cellular immune system, which takes an active part in limiting the spread and destruction of Candida spp. cells. Impaired immune system function can contribute to the development of severe forms of candidiasis [10].
Infection with fungi of the genus Candida in candidiasis of the lower urinary tract most often occurs through the ascending route in catheterized patients and patients with impaired urodynamics, especially in the presence of diabetes mellitus [2–4, 6].
Clinical manifestations caused by Candida infection depend on its location. In patients with candidal urethritis, the symptoms of the disease do not differ from those with a bacterial infection. Patients with candidal cystitis may have frequent or difficult urination, urinary urgency, hematuria, and pyuria. The cystoscopic picture of candidal cystitis can correspond to both focal and widespread lesions in the form of soft, whitish areas raised above the surface against the background of inflammatory changes in the mucous membrane [2, 6]. Thus, in most cases, when candiduria is detected, a comprehensive diagnosis is necessary, aimed at excluding urinary tract candidiasis [2, 3].
The main methods for diagnosing urinary tract candidiasis include [3]:
- microscopy and urine culture
- computed tomography or ultrasound examination of the kidneys (if indicated)
- cystoscopy (if indicated)
- determination of the type of pathogen and its sensitivity to antimycotics is indicated in case of recurrent course and/or resistance to standard antimycotic therapy
- mycological examination (repeated cultures of blood and other biosubstrates) and serological diagnostics (determination of specific antibodies, antigen in blood serum) are indicated in cases of high risk of developing acute disseminated candidiasis (presence of risk factors, clinical signs)
Treatment of candiduria and candidiasis of the lower urinary tract
The prescription of antifungal drugs when candiduria is detected is not indicated in all cases. Thus, with asymptomatic candiduria in catheterized patients there is no need for treatment with antimycotics. Antifungal therapy is mandatory in patients with asymptomatic candiduria who are at risk of developing disseminated candidiasis: after kidney transplantation and surgical interventions on the abdominal organs, in those who have suffered widespread deep burns or severe injuries, before and after urological operations, in the presence of concomitant neutropenia, in low birth weight newborns [2–7, 9]. In addition, persistent asymptomatic candiduria in neutropenic patients in the absence of fever requires further evaluation and exclusion of clinically asymptomatic hematogenous renal candidiasis [2–4, 6, 7, 9].
According to a study conducted by Sobel JD et al. (2000), in the treatment of asymptomatic candiduria in patients without risk factors for disseminated candidiasis, fluconazole therapy quickly led to a positive result, however, with continued drainage of the urinary tract, relapses occurred quite often and selection of resistant strains of Candida spp was observed. Moreover, long-term microbiological results in treated and untreated patients were comparable. According to the results of studies, cessation of antibacterial therapy and replacement of drainage led to the disappearance of asymptomatic candiduria in 20%, and with removal of the catheter - in 40% of cases [2, 3, 6, 7].
C. albicans and most other Candida species are known to have good sensitivity to fluconazole. C. krusei is often resistant to this drug, and in relation to C. glabrata, a dose-dependent effect may be determined when using it. C. glabrata and C. krusei are also characterized by reduced sensitivity to amphotericin B (Table 3) [2–4, 6–8].
Intravesical administration of amphotericin B solution has long been the standard of care for candiduria. However, the results of studies by Gubbins PO et al. (1999) showed that intravesical administration of amphotericin B and oral therapy with fluconazole are equally effective in relieving candiduria. Urine sterilization with intravesical administration of amphotericin B develops faster, but the effect of systemic fluconazole therapy lasts longer, in addition, oral therapy is more convenient and economically acceptable. According to Jacobs LG et al. (1996), in elderly patients, the rate of all-cause mortality after treatment for candiduria was higher among patients treated with bladder instillations of amphotericin B than among those treated with oral fluconazole therapy (41% vs. 22%). respectively). Thus, local therapy was associated with lower survival rates. Intravesical administration of amphotericin B solution (50–200 g/ml) is indicated only in rare cases or as a diagnostic, localization test.
In the case of diagnosis of lower urinary tract candidiasis, the use of drugs such as fluconazole, amphotericin B or flucytosine is currently recommended [2, 4, 6–9]. The most preferred of these is fluconazole. This antimycotic, unlike other representatives of the azole group, is soluble in water and 80% is excreted unchanged in the urine, creating an effective concentration in it, and also has a wide spectrum of action and is effective against the most common pathogens of candidiasis (C. albicans, C. parapsilosis, C. tropicalis, etc.). The drug is characterized by high bioavailability when taken orally (> 90%) and a long half-life (about 30 hours). The use of fluconazole is possible in patients with impaired renal function, but in such cases an appropriate dose adjustment of the drug is necessary. The course of antifungal therapy in the treatment of candiduria and urinary tract candidiasis should last 7–14 days, with fluconazole prescribed at a dose of 3 mg/kg/day (200 mg/day) [2–9]. It should be noted that at present, the generic drug fluconazole from Dr. Reddy's Laboratories Ltd. has been introduced into practical healthcare in Russia and is being successfully used. – Mikoflucan, characterized by a favorable ratio of cost and effectiveness with the required quality.
In the absence of effect from the use of fluconazole in the treatment of candidiasis of the lower urinary tract, the use of amphotericin B is justified. However, despite the high activity of this drug against most representatives of the genus Candida, its concentration in the urine is low. In addition, the concentration of this drug in urine decreases with impaired renal function. Therefore, the use of amphotericin B is indicated only for severe infections caused by fluconazole-resistant pathogens, such as C. krusei, in patients without renal failure. Amphotericin B at a dose of 0.3 to 1.0 mg/kg/day is used for 1–7 days as an intravenous infusion [2–6, 7, 9]. Liposomal forms of amphotericin B are used for severe infections caused by pathogens resistant to fluconazole, and the presence of contraindications to the use of conventional amphotericin B (renal failure, infusion reactions, etc.) [2, 3, 6].
For candidiasis of the lower urinary tract, oral flucytosine at a dose of 25 mg/kg 4 times a day is also effective, especially if the candidiasis is caused by Candida species other than C. albicans. However, its administration may lead to the development of resistance in pathogenic Candida strains. In addition, the use of this drug is contraindicated in patients with reduced renal function [6, 7, 9].
Rare fungal urinary tract infections
Detection of cryptococci, aspergillus, and pathogens of endemic mycoses in urine is extremely rare. The presence of these infections determines an unfavorable prognosis of the disease and is accompanied by high mortality.
Cryptococcal and aspergillus urinary tract infections can occur not only in patients with acquired immunodeficiency syndrome (AIDS), but also in other immune disorders [11]. In this case, conditions arise for hematogenous dissemination of the pathogen from the primary lesions to other organs and tissues, including the urinary tract, kidneys and genitals.
In systemic cryptococcosis, cryptococcuria can be an early sign of meningitis and accompany the advanced form of this disease (30–40%). The appearance of cryptococci in the urine may not be accompanied by manifestations of systemic damage. However, in this case, it is necessary to conduct a comprehensive clinical examination aimed at searching for signs of a systemic and meningeal infectious process. Cryptococcuria can occur either in an erased form or with more characteristic clinical symptoms of pyelonephritis or prostatitis. Moreover, with cryptococcal prostatitis, the symptoms of the disease are observed mainly during the formation of an abscess. Cryptococcal UTI of uncertain localization or with a blurred clinical picture may be a manifestation of a disseminated form of the disease. According to autopsy data, in 26–57% of cases, disseminated cryptococcal infection was associated with kidney damage [2].
Treatment of symptomatic or asymptomatic cryptococcuria requires a systematic approach and the use of antifungal drugs in the form of intravenous amphotericin B at a dose of 0.7 mg/kg/day or fluconazole at a dose of 5–10 mg/kg/day, and the duration of therapy should be 3–6 months . For patients with HIV infection with urinary tract lesions, fluconazole is prescribed at a dose of 200–400 mg/day. In this case, lifelong antifungal therapy is recommended for all HIV-infected patients [2].
For fungi Aspergillus spp. hematogenous spread of the infectious process is especially typical in patients with diabetes mellitus and leukemia, with possible damage to the renal parenchyma and renal pelvis, as well as the urethra and bladder [11]. Necrosis of the renal papillae in aspergillus pyelonephritis, as well as involvement of the prostate in the infectious process, can lead to the formation of a “fungus ball” - aspergilloma. In this case, surgical treatment aimed at removing abscesses and aspergillomas, in combination with systemic antifungal therapy, is indicated [11]. In this situation, amphotericin B is most preferable at a dose of 1.0–1.5 mg/kg/day; in addition, liposomal forms of amphotericin B can be used at a dose of 3–5 mg/kg/day, increasing the dose to 6 mg/kg/ days The duration of the course of therapy has not been definitively determined and depends on the time of disappearance of signs of infection with Aspergillus spp. [8, 9, 11].
Conclusion
The most common causative agents of fungal infections of the lower urinary tract are fungi of the genus Candida. When candiduria is detected, a comprehensive diagnosis is necessary, aimed at excluding urinary tract candidiasis. When candidal infection of the lower urinary tract is confirmed, fluconazole continues to be the most effective and safe drug in the treatment of this category of patients. However, the presence of some Candida species resistant to fluconazole determines the need to improve the regimens for its rational use.
Pathogenesis
As a rule, K. develops only when the body’s defenses are weakened. Pathogenetic factors of this kind are diverse: hypofunction of the parathyroid and thyroid glands, disorders of carbohydrate metabolism, depletion of plasma potassium with its normal content in erythrocytes, dysproteinemia, impaired protein-forming function of the liver, hypoadrenalism, dysmenorrhea, hypovitaminosis, maceration and minor skin injuries, chronic debilitating diseases.
Dysbacteriosis (see), which develops as a result of the use of antibiotics, corticosteroid hormones, cytostatics and immunosuppressants, is very important in the pathogenesis of K., with an increase in fungal microflora and an increase in its pathogenic properties. The immune state of the body and the degree of its specific sensitization, as well as the severity of fungal infection, are essential.
Models of focal and widespread, acute and chronic forms of K. of various localization have been developed in laboratory animals. Detection of fungi in small whitish nodules localized in the lungs, kidneys and spleen of those killed by K. or killed on the 5th day. mice (rabbits on the 10th day), is used to determine the degree of pathogenicity of the studied crops. Extracts obtained from cells of freshly isolated fungi, which were the most pathogenic for animals, have pronounced immunogenic properties. Polysaccharide preparations obtained by treating yeast cells with pepsin, betanaphthol and ethanol proved to be the most suitable for serol, K. diagnosis, immunodiffusion reaction in gel, complement fixation reaction, indirect hemagglutination and agglutination reaction of latex particles. During the process of infection and immunization with live and killed vaccines, agglutinins, precipitins, and complement-fixing antibodies are formed. The processes of phagocytosis also intensify, and allergic restructuring of the body occurs.
Risk factors
Factors contributing to infection:
- uncontrolled use of antibiotics (in this case, treatment of intestinal candidiasis is especially often required), weakened immune system;
- failure to comply with personal hygiene rules;
- inflammatory and infectious processes (especially caused by bacterial infection);
- allergic reaction, wearing contact lenses (increases the risk of ocular candidiasis);
- severe stress, psychological and physical fatigue;
- sudden climate change;
- poor nutrition, diabetes and various diseases of the endocrine system;
- leaving the limbs in water for a long time (this can cause fungus on the nails).
These factors can become a trigger for the development of thrush. And before you think about how to cure candidiasis, you first need to eliminate the influence of such negative factors.
Classification
Due to the wide variety of manifestations of K., many classifications have been proposed. However, according to the wedge, K.’s manifestations can be divided into four main groups.
A. Superficial Candidiasis:
1. Candidiasis of the mucous membranes: a) yeast stomatitis (thrush); b) yeast glossitis; c) candidal tonsillitis; d) vulvovaginal candidiasis; e) candidal balanitis and balanoposthitis.
2. Skin candidiasis: a) candidiasis; b) candidal cheilitis; c) Candidiasis of large skin folds (Intertriginous candidiasis, intertriginous yeast mycosis); d) interdigital candidal erosion of the hands; e) Candidiasis of small skin folds; f) other manifestations of smooth skin candidiasis. 3. Candidiasis of the nail folds and nails.
B. Chronic generalized (granulomatous) Candidiasis.
B. Visceral Candidiasis.
1. Candidiasis of the respiratory tract. 2. Candidiasis of the digestive tract. 3. Candidiasis of the urinary system.
D. Secondary (allergic) forms of candidiasis.
Complications
Medicines for candidiasis must be taken as early as possible, otherwise the disease may become advanced and become chronic. It is dangerous due to numerous complications.
For example, due to urogenital and vaginal candidiasis, diseases of the kidneys, urinary tract, and reproductive organs develop. There may even be infertility, cervical erosion in women, urethritis and prostatitis in men. If such a disease appears during pregnancy, a miscarriage is possible.
With ear candidiasis, sepsis may develop and hearing may deteriorate. With ocular vision, vision drops sharply. With candidiasis of the digestive organs, there is a possibility of developing anemia and peritonitis.
Clinical symptoms
Candidiasis of the mucous membranes
Yeast stomatitis
(see), or so-called. thrush occurs mainly in weakened infants and small children or in elderly people against the background of chronic diseases. Initially, on the unchanged mucous membrane of the cheeks, hard and soft palate, tongue and gums, pinpoint white deposits form, which, merging, form white films reminiscent of curdled milk. If you remove the films, you will find a bleeding mucous membrane underneath them. When a child has thrush, nipple pain may occur in a nursing woman: the skin turns red, bubbles and cracks appear on the nipple, and severe pain during feeding.
Yeast glossitis
(see) - in addition to thrush, atrophy of filiform papillae can be observed in some areas of the back of the tongue; in some patients, deep grooves of the tongue are significantly pronounced (tsvetn. Fig. 1), in which whitish deposits are visible; the entire tongue is slightly enlarged due to swelling. K. of the mucous membranes is not a serious disease, but it is a symptom indicating a general weakening of the body; Yeast glossitis is often observed in older people who wear dentures.
Candidal tonsillitis
(see) usually occurs chronically with normal body temperature and absence of pain when swallowing. Whitish plugs form on the tonsils, but there may also be plaque in the form of white films. Regional lymph nodes are not involved in the process.
Vulvovaginal candidiasis
(see) is detected by the appearance of whitish discharge, crumbly in nature. On the mucous membrane of the vagina, the edges are usually hyperemic, whitish or gray plaques and superficial erosions are found. Patients note itching and burning in the external genital area. K. is often combined with Trichomonas colpitis.
Candidiasis balanitis and balanoposthitis
(see Balanitis, balanoposthitis) - white plaques form on the head of the penis, on the inner layer of the foreskin and less often on the outer layer, under which surface erosions are found; rashes are accompanied by burning and pain.
Skin candidiasis
Candida infection
may occur as an independent disease or be a manifestation, for example, of thrush.
Yeast infection is characterized by a predominance of maceration and detachment of the upper sections of the stratum corneum in the form of a border around cracks in the corners of the mouth and significant infiltration at their base (see Zaeda). Rice.
1. Candidal cheilitis (grayish scales on the swollen red border of the lips) and glossitis (whitish coating, deep furrows on the tongue). Candidal cheilitis
(see) is characterized by redness of the red border of the lips, dryness, a feeling of tightness and burning.
The grayish scales seem to be glued to the red border of the lips, and their free edge is slightly raised (color fig. 1); To diagnose candidal cheilitis, repeated detection of fungal elements is necessary. Rice.
2. Candidiasis of large skin folds - damage to the folds of the anus and intergluteal fold with a characteristic border of macerated epidermis. Intertriginous K.
(large folds) occurs quite often. The axillary fossae, folds of skin under the mammary glands, especially in obese women, intergluteal and inguinal-femoral folds may be affected (color. Fig. 2). With this localization, large lesions with clear boundaries are formed, often with erosion and weeping. The periphery of the lesions is surrounded by a border of whitish macerated epidermis. Around the main focus, especially under the mammary glands, small lesions of the same nature (so-called daughter elements) are often found.
Interdigital candidiasis erosion
brushes occurs very often, sometimes as a manifestation of an occupational disease (occupational K.). Usually the process develops in the third interdigital fold, less often in others. The stratum corneum in the fold is swollen, macerated, and has a pearlescent tint. In the center of the lesion, an eroded red surface is found, moist and shiny due to moderate weeping. The process does not extend beyond the lateral surfaces of the main phalanges. Erosion occurs quite persistently and, without eliminating pathogenetic factors, is prone to relapse. Patients note itching and burning.
Candidiasis of small skin folds
(behind the ears, in the navel area, interdigital folds of the feet) is common. The process is characterized by the same wedge signs as when localized in large folds, and can be either the primary manifestation of K. or develop along with signs of another disease.
Other manifestations of smooth skin candidiasis can be found in the form of erythematosquamous, vesiculobullous, scarlet-like and psoriasiform rashes. Candida erythroderma is also rarely observed.
Candidiasis of the nail folds and nails
(onychia and paronychia) is usually observed only on the hands, as an occupational disease among workers at fruit processing enterprises.
Rice.
3. Candidal onychia (thickening and clouding of the nail plates) and paronychia (inflamed nail folds, no eponychium). The process often begins with the nail fold, which becomes hyperemic, “cushion-shaped”, the cuticle disappears, and when pressed, a small drop of pus is released; The acute stage gradually turns into subacute and chronic. Later, the nail plate is involved in the process, the edges gradually become bumpy with transverse stripes and depressions or become thinner, sometimes easily peeling off. The color of the affected nail plates is brownish, less often with a greenish tint. Yeast paronychia and onychia (tsvetn. Fig. 3) can be the only manifestation of K. or combined with other forms of superficial or even visceral K.
Visceral Candidiasis
Rice.
4. Chronic generalized (granulomatous) Candidiasis - on the scalp and body of the child there are flaky infiltrated spots and tubercles with horny deposits. Chronic generalized (granulomatous) Candidiasis
- an independent wedge, variety K. As a rule, the disease begins in early childhood with thrush of the oral mucosa. Then, the process gradually involves the nail folds and nail plates of the hands and feet, the scalp, the skin of the face, torso and limbs. Frequently observed yeast cheilitis, especially damage to the lower lip, leads to the development of macrocheilia. Characteristic is the subsequent appearance on the skin of the scalp, face, torso and extremities of hyperemic and flaky spots with infiltration at the base, papules, tubercles and horny deposits (color. Fig. 4). Many patients experience recurrent pneumonia: (see Pneumomycosis) and epileptiform seizures; Possible damage to the liver and kidneys. The course of the disease is chronic with exacerbations. Most patients are exhausted, children lag behind in physical activity. development.
Candida panophthalmitis, iritis, endocarditis, etc. are observed.
Respiratory tract candidiasis can be primary or secondary. Damage to the pharynx and larynx is accompanied by attacks of dry cough, changes in voice timbre, laryngostenosis and sputum production. Candidal bronchitis is manifested by a persistent cough, mucopurulent sputum, and coarse wheezing. Primary yeast pneumonia often occurs during the treatment of some other disease with antibiotics, and secondary pneumonia can occur in patients with tuberculosis and occur as a complication of pneumonia of another etiology. Sometimes, due to the formation of cavities, mycotic pneumonia resembles tuberculous lesions of the lungs, which must always be taken into account when making a differential diagnosis (see Pneumomycosis). Sometimes it resembles pulmonary sarcoidosis.
Candidiasis of the digestive tract is manifested by various symptoms: decreased appetite, difficulty swallowing, vomiting with the release of cheesy films, liquid feces mixed with mucus, etc. As intestinal cancer progresses, dehydration of the body occurs, symptoms of intoxication and adynamia are expressed, and a febrile state may be observed.
Candidiasis of the urinary system is accompanied by the appearance of protein, blood and casts in the urine, and an abundance of fungal elements; the filtration capacity of the kidneys is impaired.
Secondary forms of candidiasis
Secondary forms of candidiasis (levurides, or mycids) occur in the presence of a primary focus in the internal organs, on the skin or mucous membranes, which sensitizes the body. Clinically, levurides appear as erythematosquamous, vesicular, parapsoriasiform or other elements. Secondary allergic rashes are usually symmetrical and may be accompanied by headache, malaise, cardiac dysfunction, and changes in the peripheral blood formula. Violations of the treatment regimen, irrational therapy, injury to K.'s foci or irritation of chemicals are of significant importance in the occurrence of levurides. substances.
Complications vary, but the most severe are septicopyemia and septicemia (see Sepsis).
Diagnostics
The diagnosis of K. of visible mucous membranes, skin, nail folds and nail plates is made on the basis of the wedge, manifestations and presence of fungi when examining material from the surface of the lesions. With visceral K., additional research is required, as well as infection of laboratory animals.
Laboratory research. The material for research is skin and nail scales, discharge from ulcers, pus, cerebrospinal fluid, blood, urine, bile, feces, pieces of biopsied tissue and cadaveric material. Patol, the material is microscopically examined in a 10% caustic alkali solution, or in a double-strength Lugol solution, or in a mixture of alcohol and glycerin (2 parts alcohol, 4 parts glycerin, 4 parts water).
Rice. 7. Candida in sections of kidney tissue when examined by luminescence (arrows indicate pseudomycelia). Schiff's reagent-rivanol SO2. Rice. 8. Germination of filaments of pseudomycelium (indicated by arrows) from yeast-like Candida cells. Staining using the PAS method.
Candida can be detected with gistol. study - staining of sections of lesions according to Gram-Weigert in various modifications (see Weigert staining methods, Gram method). They are best identified by staining for neutral mucopolysaccharides according to Hotchkiss-McManus or Shabadash (see McManus method, Shabadash methods): uniform staining of yeast-like cells and pseudomycelium of the fungus is observed, phagocytosed elements of fungi, as well as dying particles of the fungus are well identified . In the earliest stages of parasitism, the direct method of luminescence (fluorescent antibodies) is used, with the help of which candida is detected (Fig. 7). As the inflammatory process develops, the intensity of the fungal glow weakens, which is associated with the synthesis of antibodies against fungal antigens. In tissue sections, fungi are found in the form of round or oval yeast-like cells, sometimes budding, pear-shaped. Lateral budding is often visible at the junction of cells (whorls). As a result of filamentation (formation of filaments), thin, short, curved and long filaments of pseudomycelium are observed, sometimes with thickenings at the ends up to 7 µm thick (Fig. 8).
Cultural diagnosis is achieved by inoculating patol, material on Sabouraud media and wort with streptomycin, penicillin, chloramphenicol to suppress the growth of accompanying microbes. For the detection of pseudomycelium and the formation of chlamydospores, the most suitable are 4-5-day streak cultures on slanted carrot-potato, corn or rice agar media. The growth of a large number of yeast colonies (over a thousand per gram of test material in cultures on solid media) indicates that this organism may be an etiol, an agent of the disease; however, repeated cultures of the same test material are necessary.
Serol, K.'s diagnosis is achieved through the agglutination reaction (see) and the complement fixation reaction (see). A sharply positive agglutination reaction in a serum dilution of at least 1:200 is considered reliable, and the reaction gives clearer results with an autoantigen - a culture obtained from the patient. The complement fixation reaction is more specific; the most clear results are obtained with generalized and visceral forms.
Specific immunofluorescence (see) turned out to be useful for determining serotypes and identifying candida.
Rice. 5. A sharply positive skin reaction to candida antigen on the skin of the shoulder.
The most important thing for K.’s diagnosis is the increase in antibody titers during the course of the disease; increase in the number of yeast-like fungi with repeated studies of patol, material. Positive allergic skin reactions (color Fig. 5) are important in combination with other data.
It is necessary to carry out differential diagnosis between candida, aspergillus (see Aspergillosis) and nocardia (see Nocardiosis).
Treatment
Therapy is carried out with mandatory consideration of pathogenetic factors. So, for example, normalization of carbohydrate metabolism or thyroid function, improvement of the general condition of the body can lead to the elimination of the wedge, manifestations of K. Etiol drugs, effects accelerate healing. General restoratives and proper nutrition for patients are important: food should be rich in proteins and vitamins, but the amount of carbohydrates should be limited. The prescription of repeated courses of nystatin, levorin or their salts is indicated (both antibiotics are most effective for K. of the digestive tract). Nystatin is prescribed orally for adults at 6,000,000 - 8,000,000 units per day (breaks are taken between courses). Amphotericin B is indicated for severe forms of visceral K. and generalized hron. TO.; it is prescribed intravenously in a 5% glucose solution in the form of drip infusions at the rate for adults of 250 units per 1 kg of the patient’s body weight with a total course dose of 1,500,000 - 2,000,000 units. Immunotherapy of patients with K. is used quite widely; a polyvalent vaccine (or autovaccine) is prescribed. Preparations from the fungus C. albicans, containing a complex of proteins, polysaccharides and lipids, are also used.
External therapy means are varied. 1-2% alcohol or aqueous solutions of aniline dyes, Castellani liquid, benucide, mycoseptin, zincundan and other fungicidal liquids are successfully used. Ointments used are amphotericin, levorin and nystatin, 10% sulfur and 3% salicylic, etc. For K. of the oral mucosa, lubrication (2-3 times a day) with aqueous solutions of aniline dyes, 10-20% solution is recommended borax in glycerin, rinsing with 1-2% aqueous solution of tannin or 1% aqueous solution of iodinol, as well as tablets with decamine in the form of caramel.
For the treatment of children, use 1-2% solutions (aqueous) of aniline dyes, 5-10% solutions of borax in glycerin - lubricating the lesions 3-4 times a day; mouth rinse with 5-10% tannin solution, caramel with decamine.
For vulvovaginitis, tampons with a 20% solution of borax in glycerin, foaming tablets of levorin, and lubrication with a 1-2% aqueous solution of aniline dye are used.
Prevention
In the production of fruits and vegetables, juices and syrups, it is necessary to introduce mechanization and automation, eliminating the use of manual processing. For infectious and other diseases, long-term use of antibacterial antibiotics should be combined with nystatin (up to 400,000-600,000 units per day) and a complex of vitamins, especially group B. It is recommended to use rubber slippers in baths and showers. Prevention is especially important for newborns and infants; in maternity hospitals and nurseries, people who have signs of K. should not be allowed to work with children. At home, patients with K. should avoid communicating with children; Dishes, linen and towels must be disinfected.
Bibliography:
Arievich A. M. and Stepanishcheva Z. G. Candidiasis as a complication of antibiotic therapy, M., 1965, bibliogr.; Blinov N.P. Pathogenic yeast-like organisms. M., 1964, bibliogr.; Kashkin P. N. and Sheklakov N. D. Guide to medical mycology, M., 1978; Moroz E. Ya. Candidiasis in children, L., 1971, bibliogr.; Khmelnitsky OK Histological diagnosis of superficial and deep mycoses, L., 1973, bibliogr.; Tsinzerling A.V. Pulmonary candidiasis, L., 1964, bibliogr.; Sheklakov N. D. and Milich M. V. Fungal diseases of humans, M., 1970; Bader G. Die viszeralen Mykosen, Jena, 1965; Baker RD The pathological anatomy of mycoses, B.-NY, 1971; Сonant NF ao Manual of clinical mycology, Philadelphia, 1971; Emmons CW, Binford CH a. Utz JP Medical mycology, Philadelphia, 1970, bibliogr.; Fungous diseases and their treatment, ed. by RW Ridell a. G. T. Stewart, p. 25, L., 1958, bibliogr.; Winner HI a. Hurley R. Candida albicans, L., 1964.
A.H. Arabian, P.N. Kashkin, N.Ts. Sheklakov; O. K. Khmelnitsky (pat. an.).