Causes of frequent urination in men
It is not considered a pathology if the frequent urge to urinate in men during the day is a consequence of consuming a significant amount of liquid or water-rich foods. Frequent urination may also occur due to hypothermia, a stressful situation, or taking diuretic medications.
Frequent urge to urinate is a symptom of many infectious or inflammatory diseases, physiological characteristics, and psychological disorders. Therefore, treatment is to eliminate the root cause of the pathology.
If nothing like this happens in life, and the number of visits to the toilet reaches 10-15 times a day, then in this case you should immediately visit a specialist to determine the reasons and receive recommendations. It is especially important to consult a doctor if you experience discomfort when emptying your bladder: pain, burning or itching.
All the reasons why frequent urination in men may occur and require treatment are conventionally divided into hormonal, physical, inflammatory and concomitant.
Treatment
The direction of treatment for frequent urination depends on the diagnostic results. First-line drugs for prostatitis are fluoroquinolones (Levofloxacin) and cephalosporins (Cefotaxime, Ceftriaxone). To relieve pain, non-steroidal anti-inflammatory drugs (Ibuprofen, Ketonol) are prescribed. In addition to tablets, rectal anti-inflammatory suppositories (Vitaprost) are used.
Read more about the use of Vitaprost for prostatitis.
For cystitis, Monural and nitrofurans (Furamag, Furagin) are prescribed. Herbal medicines are a good auxiliary remedy: paste “Fitolysin”, “Urolesan”, “Uronorm” (more information about drugs for the treatment of cystitis).
Phytolysin is a combined herbal preparation that has a diuretic, anti-inflammatory, and antispasmodic effect. Price from 433 rubles
Alpha-1-blockers (Segetis, Kardura) will help relieve the symptoms of hyperplasia. In case of severe urination problems, surgical methods are used.
For OAB syndrome, M-anticholinergics (Spazmex, Driptan, Urotol), tricyclic antidepressants (Imipramine), alpha-1-adrenergic receptor blockers, vasopressin analogues (Desmopressin) are prescribed.
Drugs used to treat OAB
In older and elderly men, the possibilities of drug and surgical treatment are limited by the increased risk of adverse reactions and the presence of chronic diseases of the cardiovascular system. They try to replace surgical interventions with conservative therapy, including hormone replacement.
At home
At home, drug treatment for nocturia can be supplemented with exercises to strengthen the pelvic floor muscles. This is especially true for the elderly. Herbal decoctions help relieve inflammation and alleviate the symptoms of cystitis and urethritis:
- Chamomile: 2 tbsp. spoons, pour a glass of boiling water, leave in a thermos for half an hour, drink half a glass three times a day before meals.
- Black poplar buds: 2 tbsp. spoons of crushed raw materials, pour 500 ml of boiling water, leave for 2 hours. Take in the same way as chamomile.
- Bearberry: pour 10 g into a glass of water, boil for 15 minutes, leave until cool, drink throughout the day before meals.
- St. John's wort: 1 tbsp. Pour 200 ml of boiling water over a spoonful of herbs and leave for 20 minutes. Drink a quarter glass three times a day.
St. John's wort infusion
These remedies will help get rid of irritation of the mucous membranes of the bladder and urethra, as a result of which the urge to urinate is normalized.
For neurogenic disorders, you can drink mint tea (infusion of peppermint, lemon balm). St. John's wort, valerian, and linden are good natural antidepressants.
Physical causes of frequent urination
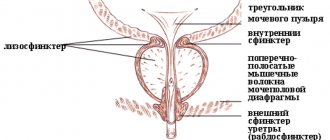
The physical reasons for which urine is released from a full bladder often and little by little is a narrowing of the lumen of the urethra as a result of:
- incomplete blockage of stones in urolithiasis;
- proliferation of the prostate gland (prostatitis and adenoma);
- formation of post-traumatic or congenital strictures (narrowing) in some areas of the urethra;
- malignant tumor.
With pathologies of the prostate gland, men experience pain and a frequent urge to urinate, even at night.
Reasons why men may have difficulty urinating
There are different reasons for this disease. However, most often the cause of difficulty urinating is inflammation of the prostate gland or prostate hypertrophy (enlargement of the prostate gland). As a result, the outflow of urinary fluid becomes difficult and the stream of urine becomes rare, due to the enlarged prostate, which puts pressure and blocks the urethra. Also, the following reasons are typical: - the presence of infection in the pro.
These could cause infrequent urination.
Inflammatory diseases of the bladder
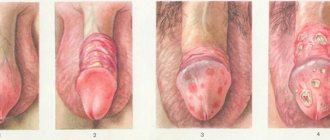
Inflammatory processes are formed in response to the introduction of pathogenic microorganisms into the organs of the urinary system (cystitis, urethritis, pyelonephritis, glomerulonephritis). A man’s body can react by frequent urination without pain both at night and during the day to an existing sexually transmitted disease (gonorrhea, chlamydia, trichomoniasis).
As a result of inflammation, the receptors of the bladder, ureters and urethra are constantly in a state of excitement. This manifests itself in the form of a false feeling of fullness and the urge to urinate frequently. Sometimes a similar condition in men occurs without pain, but more often it is accompanied by pain in the lower abdomen, a burning sensation during the process, and an increase in body temperature. The urine is cloudy due to the admixture of pus or blood, with an unpleasant odor.
Drug treatment for overactive bladder
Overactive bladder (OAB) is a clinical syndrome with symptoms of frequent and urgent urination with (or without) urgency urinary incontinence and nocturia (urination between falling asleep and waking up). OAB is based on detrusor hyperactivity of a neurogenic or idiopathic nature. is a consequence of neurological diseases. indicates that the cause of involuntary detrusor contractions is unknown. When frequent, urgent urination is not accompanied by detrusor overactivity in the absence of other causes of these symptoms, the term is used [5]. Thus, the term OAB is a general term to refer to all of the above urination disorders. However, the term OAB does not purport to replace the well-known terminology of the International Continence Society, which is used by a narrow circle of urologists. Figure 1 and Table 1 present urodynamic and clinical terms for frequent and urgent urination.
Rice. 1. Clinical and urodynamic terms for frequent and urgent urination
An analysis of the medical literature in recent years shows an increased interest among doctors in the problem of OAB, which was greatly facilitated by the results of epidemiological studies on the prevalence of OAB. According to the International Continence Society, OAB occurs in approximately 100 million people worldwide. In the United States, the diagnosis of OAB is more common than that of diabetes mellitus, gastric and duodenal ulcers, and is included in the 10 most common diseases. There is reason to believe that 17% of the European adult population have symptoms of OAB [14]. It is believed that imperative urination is observed in 16% of Russian women [3].
Despite the fact that OAB is more often noted in old age, symptoms of OAB are quite common in other age groups. According to our data, the largest number of patients was observed over the age of 40 years, while in men over 60 years of age there is a clear tendency towards an increase in incidence, while in women, on the contrary, a decrease [2]. The data presented clearly demonstrate that OAB is a very common clinical syndrome, occurring in various age groups and leading to physical and social maladaptation of such patients.
Clinically, patients with OAB more often have idiopathic detrusor hyperactivity, less often neurogenic, and even more rarely OAB without detrusor hyperactivity (according to our data, in 64%, 23.5% and 12.5%, respectively). If idiopathic detrusor hyperactivity is observed 2 times more often, and OAB without detrusor hyperactivity is 6 times more often in women, then neurogenic detrusor hyperactivity occurs almost equally often in both women and men [2].
Etiology and pathogenesis
It has been reliably established that OAB can be a consequence of neurogenic and non-neurogenic lesions. The first are disorders at the level of the supraspinal centers of the nervous system and the spinal cord pathways, the second are a consequence of age-related changes in the detrusor, bladder outlet obstruction and anatomical changes in the position of the urethra and bladder.
Some morphological changes in the detrusor are known due to its hyperactivity
. Thus, in most patients with OAB, a decrease in the density of cholinergic nerve fibers is detected, which, in turn, have increased sensitivity to acetylcholine. These changes are defined as “postsynaptic cholinergic detrusor denervation” [12]. In addition, using electron microscopy, it was possible to establish violations of normal intercellular connections in the detrusor of the GMF in the form of protrusion of intercellular connections and protrusion of the cell membrane of one myocyte into another neighboring myocyte with the convergence of intercellular boundaries - “a tight connection of two parallel planes of adjacent myocytes” [11,18] . Based on these morphological changes, which are believed to be characteristic of OAB, Brading and Turner in 1994 proposed a theory of the pathogenesis of the development of detrusor hyperactivity, which is based on the increased excitability of myocytes that are in close connection with each other in places of denervation [9,10].
It is believed that the cause of denervation, in addition to nervous disorders, may be detrusor hypoxia
due to age-related ischemic changes or due to bladder outlet obstruction. In the latter case, this is confirmed by the presence of OAB in 40–60% of men with benign prostatic hyperplasia [8]. Thus, the pathogenesis of detrusor overactivity in OAB is presented as follows: hypoxia that occurs in the detrusor as a result of age-related arteriolosclerosis or as a result of IVO, leading to hypertrophy and infiltration of the detrusor connective tissue, leading to detrusor denervation (detected in detrusor biopsies for all types of detrusor hyperactivity), as a result, structural changes occur in myocytes (close contact between myocytes with increased nervous excitability and conductivity), as a compensatory reaction to a deficiency of nervous regulation. In this case, any spontaneous or provoked by stretching of the bladder wall (the period of urine accumulation) contraction of individual myocytes in the form of a “chain reaction” leads to involuntary contractions of the entire detrusor. The proposed theory of the development of detrusor hyperactivity in OAB is currently leading.
Clinical course and examination tactics
Frequent daytime and night urination, as the predominant symptoms of OAB, we observed approximately 2 times more often without urgent urination and 3 times more often without urgent urinary incontinence, which is undoubtedly the most severe manifestation of OAB, since it causes incomparably significant suffering for patients. A feature of the course of OAB is the dynamics of its symptoms. During a 3-year follow-up period, in almost a third of patients, urge urinary incontinence spontaneously regresses without treatment and recurs again at different times. The most persistent symptom is frequent urination, which often reaches such a level that it makes patients completely unable to work and pushes them to make rash decisions.
In addition to collecting anamnesis and physical examination, all patients with frequent and urgent urination are assessed for urination frequency (based on a 72-hour urination diary), urine sediment examination and urine culture for sterility, ultrasound scanning of the kidneys, bladder, prostate, with determination of residual urine. The results of the urination diary are most important: having assessed them, one can largely assume OAB and, based on this, quickly decide on the initiation of treatment and its methods. OAB is eligible for diagnosis if there are at least 8 urinations and/or at least 2 episodes of urge urinary incontinence during the day
. It is important that the results of such an initial examination, which is carried out at the outpatient stage, often make it possible to identify diseases that are accompanied by symptoms of frequent and urgent urination, but are not related to OAB.
When OAB is detected, treatment can be started immediately to improve the patient’s quality of life by stopping frequent and urgent urination. In case of ineffectiveness of treatment or at the request of the patient, to clarify the form of OAB (idiopathic or neurogenic detrusor hyperactivity, OAB without detrusor hyperactivity), cystometry and special tests with cold water and lidocaine are performed, which allow one to suspect neurological disorders underlying the development of detrusor hyperactivity. In all cases, when detrusor overactivity is detected, a detailed neurological examination is indicated.
Treatment
Treatment of patients with OAB is aimed primarily at restoring lost control over the storage capacity of the bladder. For all forms of OAB, the main treatment method is medication. Anticholinergics
(M-anticholinergics)
are standard drugs for such treatment
.
These drugs are used both as monotherapy and in combination with other drugs (Table 2). Below we will report which anticholinergic drugs are advisable to use in the modern treatment of OAB symptoms. Typically, medications are combined with behavioral therapy, biofeedback, or neuromodulation. The mechanism of action of anticholinergic drugs is the blockade of postsynaptic (M2, M3) muscarinic cholinergic receptors of the detrusor. This reduces or prevents the effect of acetylcholine on the detrusor, reducing its hyperactivity. In humans, five types of muscarinic receptors are known, of which the detrusor contains two - M2 and M3. The latter make up only 20% of all muscarinic receptors in the bladder, but they are responsible for the contractile activity of the detrusor. Location of M2 – heart, hindbrain, smooth muscle, potassium channels; M3 – smooth muscles, glands including salivary glands, brain. The cellular response to M2 stimulation is negative, isotropic, decreased presynaptic release of transmitters; M3 – contraction of smooth muscles, secretion of glands, decrease in presynaptic release of transmitters. It has been proven that activation of M2 receptors leads to inhibition of the sympathetic activity of the detrusor, which increases its contractile activity. Thus, blockade of M2 cholinergic receptors is essential along with blockade of M3 in suppressing detrusor hyperactivity. It is believed that M2 cholinergic receptors are largely responsible for the development of detrusor hyperactivity in neurological diseases and in elderly patients. M receptors are the main target of drug treatment for OAB
. M3 anticholinergic medications remain the drugs of choice, among which highly selective ones play a special role. According to their chemical structure, anticholinergic drugs are divided into secondary, tertiary (oxybutynin hydrochloride, tolterodine tartrate) and quaternary (trospium chloride) amines. From a practical point of view, this division allows us to assume the development of side effects depending on the chemical structure of the drug. In particular, it is believed that quaternary amines, compared to secondary and tertiary amines, penetrate the blood-brain barrier to a lesser extent and, therefore, are less likely to develop side effects from the central nervous system. This point of view has not yet been fully confirmed in clinical practice, since the development of side effects is also determined by other features of anticholinergic drugs (organ specificity, drug pharmacokinetics, drug metabolites, type of receptors blocked).
The use of anticholinergic drugs was limited due to the severity of systemic side effects, primarily dry mouth, which developed with blockade of M receptors of the salivary glands, often forcing patients to refuse treatment.
When using the immediate-release form of oxybutynin (used since 1960 and remains the standard for comparison with other anticholinergic drugs), only 18% of patients continue treatment during the first 6 months due to side effects [13]. Side effects include not only dry mouth, but also impaired vision clarity, decreased tone of smooth muscle organs and associated inhibition of intestinal motility and constipation, tachycardia, in some cases central effects (drowsiness, dizziness), etc. Side effects lead to the need for dose titration (for oxybutynin - from 2.5 to 5 mg 3 times a day). A significant step forward is the synthesis of a new anticholinergic drug, tolterodine.
, proposed specifically for the treatment of OAB.
Tolterodine is a mixed antagonist of M2 and M3 cholinergic receptors, which has a distinct organ specificity of action in relation to the detrusor. Unlike oxybutynin, which has pronounced selectivity for M1 and M3 receptors, tolterodine demonstrates almost identical sensitivity to different subtypes of M receptors. Our experience with the use of an immediate-release form of tolterodine at a dose of 2 mg 2 times a day in 43 patients with idiopathic detrusor overactivity indicates its high effectiveness. After 12 weeks of use, the number of urinations per day decreased on average from 13.5 ± 2.2 (9–24) to 7.9 ± 1.6 (6–17), and episodes of urge urinary incontinence from 3.6 ± 1. 7 (1–6) to 2.0±1.8 (0–3). The immediate-release form of tolterodine is relatively well tolerated, as evidenced by data from clinical trials in which 82% and 70% of patients completed 6- and 12-month courses of treatment, respectively, indicating that the effectiveness of therapy is maintained over the long term. The incidence of side effects with the immediate-release form of tolterodine was practically the same as in the placebo group, with the exception of dry mouth, which was observed in 39% of patients taking tolterodine and in 16% of the placebo group [6]. Our data also indicate good efficacy and tolerability of the immediate-release form of tolterodine
(4 mg) over 6 months. treatment in 16 patients with neurogenic detrusor hyperactivity. There was a decrease in the average number of daily urinations by 5.7/day, episodes of urgent urinary incontinence by 2.7/day and an increase in the average effective bladder volume by 104.5.
Clinical studies show that anticholinergic drugs lead to a reduction in the frequency of OAB symptoms within 1–2 weeks of treatment, with maximum effect achieved by 5–8 weeks. At the same time, treatment involves long courses. Despite this, in most cases of monotherapy with anticholinergic drugs, after their withdrawal, a relapse of OAB symptoms is observed, which makes it necessary to take them continuously in order to maintain an adequate therapeutic effect.
The use of anticholinergic drugs, in particular tolterodine, requires careful monitoring and caution, especially in patients with neurogenic detrusor overactivity. The fact is that with prolonged uncontrolled use of these drugs, patients may experience a disturbance in the contractile activity of the detrusor, with the development of chronic urinary retention, urethrohydronephrosis and chronic renal failure. For timely monitoring of possible side effects, it is necessary to evaluate the amount of residual urine. We recommend that in the first three months after the prescription of anticholinergic drugs, the amount of residual urine is determined at least once every two weeks, and subsequently once a month. Patients should be warned about the possibility of such a complication and immediately inform the doctor if they experience incomplete emptying of the bladder.
It is known that, along with drugs, their metabolites are responsible for the development of side effects, the concentration of which in the blood and their affinity for M - cholinergic receptors often exceeds those of the original drugs. For example, the metabolism of oxybutynin leads to the formation of N-desityl oxybutynin, and tolterodine - to the active metabolite - 5-hydroxymethyl derivative. These data provided the basis for the use of anticholinergic drugs other than oral forms. In particular, intravesical administration of oxybutynin
or rectal suppositories.
Penetration of the drug directly into the blood, bypassing the liver, with such forms of administration is not accompanied by the formation of metabolites, which reduces the number of side effects. Since 1999, a slow-release form of oxybutynin
based on the OROS osmotic delivery system, which provides prolonged release of the drug and its constant concentration in the blood plasma over 24 hours. Clinical studies show that the slow-release form of oxybutynin is effective in reducing the symptoms of urinary urgency , comparable to the immediate-release form with fewer side effects (25% versus 46%). It is believed that this is why 60% of patients with OAB continue to take the slow-release form of oxybutynin for 12 months. at a dose of 15 mg per day [7].
Currently, the effectiveness and tolerability of the S-form of oxybutynin is being studied, and transdermal ( OXYtrol patch)
) and intravesical (
UROS
) forms of oxybutynin.
The slow-release form of tolterodine consists of many small beads made of polystyrene. The active substance is located on the surface of the beads and is covered with a special capsule. The drug is released when the capsule is destroyed by the acidic contents of the stomach. This delivery system ensures a constant level of the drug in the blood over 24 hours. The slow-release form of tolterodine has a more significant reduction in episodes of urge urinary incontinence and is better tolerated compared to the immediate-release form. Patients receiving slow-release tolterodine had 23% fewer cases of dry mouth [19].
Considering the insignificant number of side effects when using slow-release forms of anticholinergic drugs, the issue of increasing their dose in the treatment of patients with OAB has recently been discussed in the literature. This is due to the fact that most patients have a positive effect when using a standard dose of anticholinergic drugs and only some of them get rid of OAB symptoms completely. At the same time, despite good tolerability, doctors usually do not increase the dose of drugs to completely eliminate the symptoms of OAB. Clinical research and practice show that a significant number of patients with successful results of therapy with anticholinergic drugs may subsequently have clinical improvement in symptoms with increasing doses of these drugs [16].
A separate question arises about the possibility of using anticholinergic drugs in patients with OAB and bladder outlet obstruction.
. Despite the fact that anticholinergics reduce frequency and urgency of urination, doctors are wary of using them in patients with concomitant bladder outlet obstruction due to the risk of developing acute urinary retention. Only two randomized controlled trials have examined this issue. These studies showed that the immediate-release form of tolterodine, used alone or in combination with tamsulosin (a1-blocker), is safe against the potential development of acute urinary retention and improves quality of life in patients with detrusor overactivity in combination with mild to moderate bladder outlet obstruction and moderate amount of residual urine [4,8].
We used an immediate-release form of tolterodine (2 mg twice daily) in 12 patients with OAB in combination with benign prostatic hyperplasia [1]. In 2 patients, in the first 3 weeks of treatment, the appearance of residual urine in a volume of up to 100 ml was noted, which was an indication for discontinuation of treatment. In 10 patients, after 12 weeks of treatment, the average I-PSS score decreased from 17.2 to 11.7 due to irritative symptoms, and the average quality of life score decreased from 5.2 to 3.1. The number of urinations according to the urination diary decreased from 14.6 to 9.2. The maximum urine flow rate not only did not decrease, but even slightly increased from 12.3 to 13.4, which is likely due to an increase in the storage capacity of the bladder. There is no doubt that further research is needed to clarify the possibility of using anticholinergic drugs in patients with OAB and bladder outlet obstruction.
There are isolated reports of a scattered nature on the use of other drugs in patients with OAB. In particular, the use of tricyclic antidepressants, calcium ion antagonists, α1-adrenergic blockers, prostaglandin synthesis inhibitors, vasopressin analogues, β-adrenergic stimulants and potassium channel openers has been reported. However, due to the small number of observations, an accurate assessment of the results of their use in the treatment of OAB is currently not possible. These drugs are usually used in combination with anticholinergic drugs.
Recently, the successful use of capsaicin
and
resiniferotoxin
[17]. These substances are injected into the bladder in the form of a solution. Capsaicin and resiniferotoxin are drugs with a specific mechanism of action, which consists of reversibly blocking the vanilloid receptors of the afferent C-fibers of the bladder. These drugs are used today mainly in patients with neurogenic detrusor overactivity in the absence of effect from traditional medications.
We tested a new method of drug treatment for OAB, which is considered very promising throughout the world. The method consists of sequential injection of a total of 200–300 units of botulinum toxin type A into various parts of the detrusor
. The mechanism of action of the toxin is to block the release of acetylcholine from the presynaptic membrane at the neuromuscular synapse, which leads to a decrease in the contractile activity of the detrusor. In most cases, previous muscle activity is restored within 3–6 months. after the introduction of the toxin, but often this can occur after a year or more. Our results of using botulinum toxin type A in 3 patients with neurogenic detrusor overactivity indicate an increase in bladder capacity, which is clinically manifested by a decrease in the number of urinations and episodes of urge urinary incontinence. However, there is not yet sufficient data to characterize with great certainty the effectiveness of this treatment method.
Thus, literature data and our own experience indicate that among drug treatment methods, anticholinergic drugs occupy a leading place in the treatment of OAB and allow obtaining good results in a significant number of patients.
Improving the methods and forms of administration of anticholinergic drugs while maintaining therapeutic effectiveness can reduce the number of side effects. It is hoped that as knowledge expands regarding the pathophysiological processes underlying the development of detrusor overactivity, fundamentally new targets for pharmacological treatment will emerge. Literature:
The influence of concomitant diseases on urine output
Sometimes the causes of frequent urination without pain in men are diseases that do not have a direct connection with the urinary system, but at the same time they have a significant impact on it. These include iron deficiency anemia, spinal cord injuries, reactive arthritis, and neurological disorders.
Overactivity of the muscular layer of the bladder and an increase in the acidity of its contents also often cause frequent urination in men without pain, both during the day and during the night.
Treatment of illness in men
If you have problems with obstructed urine flow, it is necessary to treat the disease.
The disease will not go away on its own, and if the situation is not improved, you can get a number of severe harmful complications that will cause colossal harm to men’s health.
The doctor, before prescribing treatment, sends the potential patient for diagnostics. After a full examination has been completed, we can talk about the diagnosis and prescribe individual treatment for the man. Treatment consists not only of reducing pain and alleviating the patient’s condition, but also of eliminating the causes of the disease. If the cause of difficulty urinating is an infection, then the doctor will prescribe antibiotics in combination with other medications.
However, sometimes conservative treatment is not suitable, and then only surgical intervention is required. But this happens extremely rarely and only in particularly advanced cases. Preventive measures: - eliminate alcohol consumption or reduce the amount of consumption to a minimum; - take medications only as prescribed by a doctor, avoid self-medication; — contact your doctor with problems in a timely manner.
pochkipro.ru
Diagnostics
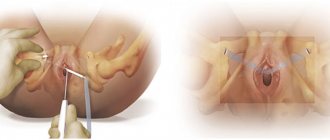
With the problem of difficulty urinating, contact a urologist. To identify pathogens in the genitourinary system, a general analysis and culture of urine, a blood test are done, a smear is taken from the urethra, and prostatic juice is taken for culture.
To determine the location of the urethral stricture, an x-ray examination is performed - urethrography, urethroscopy, uroflowmetry. To assess the condition of the urethra from the bladder side, fiberoscopy is performed.
Ultrasound allows you to determine the condition of the kidneys, prostate and bladder, and measure the amount of residual urine. Urethrocystoscopy is used to examine the walls of the bladder.
Progress of the urethrocystoscopy procedure
Folk remedies
If treatment for urinary retention is carried out at home, men and women are allowed to additionally use folk remedies. For internal use, you can prepare an infusion of rose hips. The fruits are infused for a week in vodka or alcohol. Light brown medicine is taken 2 times. per day in the amount of 10 drops, diluted with a small amount of water.
Celery juice as a folk remedy for treating difficulty urinating is useful to drink half an hour before meals. Squeeze it out from the freshly dug rhizome of the plant. Drink 2 tsp several times a day.
During the flowering period of lily of the valley, it is easy to find fragrant flowers. In the amount of one pinch, they are brewed with a glass of boiling water. Take 2 tsp of useful steam. up to 5 r. in a day.
When a man complains “I can’t pee,” his condition will be alleviated by an infusion of common chicory. Phyto-raw materials (1 tsp) are doused with a small amount of boiling water and left for a couple of hours. Use the product 2 times. before meals, adding sugar if desired.
For acute spasms of the bladder, a herbal mixture consisting of the following components will be useful:
- Rue herb – 3 parts.
- Potentilla greens – 3 tsp.
- Valerian roots – 2 tsp.
- Melissa roots and leaves – 2 tsp each.
The plants are thoroughly mixed, 1 tbsp is taken. and pour a glass of boiling water over the mixture. Infuse the liquid for half an hour and take it warm.
A pumpkin stalk, one of the most effective folk remedies, will save men and women from dysuria. 20 g of crushed product along with 400 ml of water are brought to a boil and immediately removed from the stove. Drink pumpkin broth 1/2 cup up to 4 r. per day.
For strangury, an infusion of hop cones is effective. 1 tbsp. the raw materials are steamed in a glass of boiling water. It is recommended to drink the resulting tea 3 times a day. 1 large spoon per day.
For painful urination with sluggish, cutting pressure, the following recipe is suitable for women and men:
- Take equal parts of fennel and caraway seeds and elderberry and adonis inflorescences.
- Place three times more juniper fruits and parsley seeds.
- Mix the ingredients and take 1 tbsp.
- Pour a glass of boiling water over the mixture and leave for 6 hours.
- Additionally, boil the infusion for 15 minutes.
- Take the entire volume in small portions throughout the day.
Any problems of the urinary system with weakened urine pressure and pain in the abdomen have long been eradicated by folk healers with bearberry leaves. The plant is known as bear's ear. 1 tbsp. raw materials are brewed with a glass of boiling water and wait until the liquid cools. Take the medicine three times a day, 1 tbsp.
Here is another recipe that will help you forget forever about the symptoms of strangury (insufficient urinary pressure, discomfort when visiting the toilet, frequent episodes of urination in small portions). Its ingredients are:
- Nettle – 3 parts.
- Horsetail herb – 6 parts.
- Rose petals, black currant and birch leaves, cape grass, juniper berries and lavender flowers - 1 part each.
- Herb medicinal cap and leaves of bearberry, plantain, lingonberry - 2 parts each.
A few grams of the resulting mass are poured over 2 cups of boiling water and covered with a lid for half an hour. The drug is consumed warm, 150 ml several times a day.
Prevention of dysuria
Preventing urinary problems is always easier than treating them. In order for urine to pass easily, painlessly, with pressure, men are advised to give up bad habits, change their diet towards avoiding fried, fatty and spicy foods and eat more fruits, herbs and vegetables.
Also, you should not overcool and enter into casual relationships with untested partners (you can get STDs from them). At the same time, sex life should be regular, and the overall lifestyle should be active.
increase member.rf
Causes
Why do problems arise in this area? There are several main factors:
- Infections, diseases, injuries or irritations of the urinary tract. For example, these could be bacterial infections or urolithiasis.
- Diseases in which urine production increases.
- Damage to muscles, nerves, or other structures that affect bladder function.
- Violation of the normal anatomical location of the pelvic organs, for example, the appearance of cystocele, the development of benign prostatic hyperplasia, urethral strictures.
- Pregnancy.
- Taking medications - diuretics, anticancer drugs (cyclophosphamide).
- Carrying out procedures to treat cancer, such as radiation therapy to the pelvic area.
Frequent, painless urination may occur when drinking large amounts of liquid, alcohol, or caffeine.
Treatment of urinary incontinence in men at home
- Antihistamines
Antihistamines block the action of the chemical histamine during an allergic reaction to an irritant (allergen). Allergic symptoms such as sneezing or itching are significantly reduced by taking an antihistamine.
Before giving antihistamines to children, be sure to consult a doctor.
Some antihistamines are purchased with a prescription, and some are purchased without it. They are taken by mouth (oral) or directly through the skin (topical). Pills and capsules contain a clearly defined dose of this drug. Its amount in a cream or ointment is more difficult to calculate: it depends on how much of the substance is applied to the skin in one procedure. Excess antihistamine that enters the body through the skin can have a toxic effect (this is especially dangerous for children), so doctors do not recommend the use of cream or ointment containing antihistamine.
- Sedatives or tranquilizers
Tranquilizers are medications that have a calming effect on the human body. Typically, sedatives and tranquilizers weaken and slow down a number of body functions or the activity of certain organs, such as the heart.
Mild sedatives and tranquilizers can be used to reduce anxiety or other nervous system problems, promote drowsiness, or regulate the functioning of an organ. For example, a small dose of a sedative can reduce coughing, nausea, and cramps. Stronger drugs are used for severe sleep disturbances, severe nervous shock, symptoms of psychotic disorders (for example, hallucinations or acute delusions), and also as anesthesia. These types of sedatives and tranquilizers should only be taken as prescribed by a medical professional, as they can be addictive. Excessive use of potent substances can lead to serious health problems.
- Narcotic drugs
Narcotics (also called opioids or opiates) are substances that can relieve pain and reduce the emotional response to pain by reducing the number of pain signals sent by the nervous system. Narcotic drugs provoke a feeling of well-being (euphoria) and cause mood changes, inhibition of mental operations and deep sleep.
The most commonly prescribed narcotics are meperidine, butorphanol, codeine, morphine, and hydrocodone. Don't forget: heroin is an illegal drug. Side effects of narcotic drugs include constipation and nausea. Frequent use of drugs causes addiction to them.
- Calcium channel blockers
Calcium channel blockers are medications commonly used to:
- Reducing blood pressure and preventing chest pain in people with angina pectoris.
- Treatments for high blood pressure.
The following calcium channel blockers may also slow your heart rate:
- Diltiazem (eg, Cardizem, Dilacor XR, Tiazac)
- Verapamil (eg Kalan SR, Isoptin SR)
Diltiazem and verapamil are used for atrial fibrillation.
By slowing the heartbeat and normalizing blood pressure, calcium channel blockers reduce the workload on the heart. These drugs can also improve blood flow to the heart by causing spasms in the coronary artery, which carries blood to the heart muscle. Successful treatment of high blood pressure also helps reduce the risk of atrial fibrillation.