Sex is not only a mechanism for satisfying libido or a method of reproduction.
Intimacy is a unique expression of the emotional connection between partners.
Therefore, many women and men are interested in the question of continuing sexual intercourse with diseases of the pelvic organs.
In particular, in the case of cystitis development.
What sexually transmitted infections contribute to the development of the disease and where to go, we will consider further.
What causes cystitis after sex
This infection occurs as an ascending disease.
Pathogenic bacteria are first localized in the urethral canal, affecting its mucosa.
In most cases (>80%) these are gram-negative bacteria, such as Escherichia coli (Escherichia coli), Proteus penneri, Klebsiella, Pseudomonas aeruginosa and enterococci.
They can be identified as a trigger (root cause).
Bacteria that do not have a cell wall can also contribute to the development of cystitis, in particular mycoplasmas and ureaplasmas.
Cystitis often develops against the background of chlamydia.
More rarely, inflammation of non-infectious etiology can be found.
Non-infectious causes of cystitis include radiogenic or chemical irritants, such as cytostatics such as Cyclophosphamide.
In addition, allergic reactions and certain types of urological tests can cause inflammation of the bladder.
Cystitis of the secondary type develops against the background of pathologies of the bladder or diseases of nearby organs.
In men, cystitis is more often associated with prostatic hyperplasia.
In addition to the main reasons, there are risk factors that can become a trigger for the development of cystitis:
- A woman's first sexual experience (“honeymoon cystitis”)
- Pregnancy
- Estrogen deficiency
- Urinary disorders
- Bladder stones
- Vesicoureteral reflux
- Diabetes
- Hypothermia (hypothermia)
Today it is customary to distinguish the following forms of the pathological process:
- Acute cystitis
- Chronic
- Bacterial
- Abacterial
- Uncomplicated
- Complicated
- Interstitial cystitis (non-infectious inflammation, 10 times more common in women)
The pathology that develops after intimacy is accompanied by pain in the pelvic area, most often aching pain and spasms.
The frequency of deurination increases, which is often accompanied by a burning sensation in the urethra.
Other symptoms include:
- Nocturia
- Pollakiuria (characterized by increased frequency of urination with small amounts of urine)
- Painful urination (often accompanied by a burning sensation)
In addition, hematuria, urinary incontinence, and itching in the genital area or urinary tract may be present.
Fever does not usually occur with cystitis, indicating an ascending urinary tract infection.
The likelihood of acute cystitis can be systematically assessed using the Acute Cystitis Symptom Score (ACSS).
Here, differential diagnoses and secondary data such as pregnancy, infections, and existing STDs are requested.
Complications may include pyelonephritis, prostatitis and epididymitis.
Persistent cystitis after sexual intercourse: causes, treatment
Antibacterial drugs, most often prescribed, are temporary therapeutic in nature.
Because they do not affect the root cause of the disease.
The main reason why acute cystitis develops after sex is the deep location of the urethral canal or gaping of the urethra.
In this case, during sexual intercourse, the penis is a kind of “pump”.
It pushes bacteria (usually Escherichia coli) into the bladder.
How soon after sex can cystitis develop?
After about one day or several days, symptoms of acute inflammation develop.
The main and effective method of treatment is surgery.
Its goal is to normalize the location of the urethra.
After normalizing the location of the urethra, the possibility of bacteria entering the bladder during intimacy will automatically be eliminated.
A type of surgery called “urethral transposition” is used.
The procedure is urological-type reconstructive plastic surgery.
Today this is the only effective method of eliminating chronic, postcoital cystitis.
Upon admission to the hospital, blood tests, a chest x-ray, and a cardiogram will be performed.
In the first few days after surgery, there may be a burning sensation in the urethra.
Small drops of blood may appear in the urine.
At the time of surgical manipulation, only a few minimal incisions are made.
Next, the urethra is isolated and fixed in its anatomical place.
The surgery is minimally invasive, the period of complete recovery is observed after 10-14 days.
In the postoperative period, you need to take about 1500 ml of fluid per day.
You should avoid drinking coffee, alcohol, smoking, and anything that can cause symptoms of irritation.
In some cases, the inflammatory response spreads to other organs, such as the kidneys or prostate gland.
For this reason, patients often complain of pain in the back or lumbar area.
Women suffering from inflammation of the bladder are susceptible to the spread of the pathological process to nearby pelvic organs and the vagina.
Severe symptoms of cystitis indicate an acute course of the disease.
Then it is strongly recommended not to resort to sexual intercourse, at least until the clinical picture is relieved.
Exacerbation of cystitis is also possible after anal sex.
If the patient does not want to exclude sex during cystitis, it is imperative to visit a doctor.
The specialist will warn you about possible consequences and tell you the rules to minimize complications.
Sex during cystitis is possible, subject to the following rules:
- Before and after sexual intercourse, personal hygiene should be carried out using antiseptic agents for the intimate area.
- Before planned sexual intercourse, it is necessary to avoid excessive fluid intake, which will avoid increased pressure on the inflamed bladder.
- With cystitis, sex positions should be as comfortable as possible for the patient and not cause additional discomfort or pain.
- Without fail, sex with a diagnosis of cystitis must occur with the use of barrier methods of contraception in the form of a condom, which will avoid complications of the disease after unprotected sex.
How long can you not have sex after an exacerbation of cystitis?
It all depends on the patient’s condition and general well-being.
After the acute signs of cystitis have been relieved, it is necessary to allow the body to recover and provide rest for at least a few days.
It is also worth remembering that an exacerbation of pathology can follow after violent sex.
Cystitis in women is accompanied by pain in the lower abdomen, which can intensify significantly during sex.
In men, cystitis may be accompanied by severe pain during ejaculation.
Why does cystitis start after sex?
Very often, in women, the onset of sexual activity coincides with the onset of cystitis after sex, and each exacerbation of cystitis is associated with sexual intercourse and occurs either immediately or within 24 hours after sex. This is very difficult for girls, as well as their partners, as they become afraid of sex.
Cystitis occurs after sex
After sex, postcoital cystitis begins. Manifestations of cystitis after sex
can vary, from discomfort in the urethra, to sharp pain with every urination, to blood in the urine.
An appointment with a urologist ends with the prescription of antibacterial drugs, a urine test, and an ultrasound scan. Many women treat cystitis after sex
on their own on the advice of relatives and friends.
What is the cause of cystitis after sex
or postcoital cystitis?
Dystopia of the external urethral meatus
And the occurrence of cystitis after sex
This is due to the fact that the external opening of the urethra is located very close to the entrance or on the anterior wall of the vagina, which leads to traumatization during sexual contact, and it does not matter whether the contact is protected or not.
This arrangement of the urethra is called dystopia of the external urethral meatus . To diagnose urethral dystopia, it is enough to examine the woman in a chair, and everything will become clear whether there is urethral dystopia or not.
In what cases should you refuse sex if you have cystitis?
This is recommended in the following cases:
- In the case of a prolonged course of the pathological process with periods of deterioration and exacerbation of inflammation.
- With concurrent diseases of the genitourinary system, in particular sexually transmitted infections.
- If the day before there was a fact of hypothermia, which is already a trigger for the onset of urinary inflammation. In this case, intimate intimacy should be avoided or condoms should be used.
Experts strongly do not recommend sex during acute cystitis and its treatment.
Any physical activity slows down the healing process and can worsen the patient's condition.
These recommendations especially apply to women.
Gynecologists insist on excluding sex when treating cystitis.
The use of antibacterial drugs, suppositories, vaginal creams often leads to a decrease in the production of vaginal secretions.
Insufficient natural lubrication during therapy can lead to mechanical damage to the vaginal mucosa, causing microtrauma and erosion.
In this case, it is recommended to abstain from sexual intercourse for 3-5 days.
If pain continues to bother you, you should definitely visit a gynecologist.
How soon can you have sex if you are diagnosed with cystitis?
Ideally, any sexual activity should occur after complete recovery.
It is also recommended to exclude anal sex during cystitis until the signs of the disease are completely relieved.
Sex with chronic cystitis has fewer contraindications.
Since pain symptoms are usually absent or not accompanied by severe discomfort.
However, it is necessary to exclude excessive sexual activity.
Because after “hard” sex or too frequent sex (more than once a day), chronic inflammation can sharply move into the acute phase.
In women whose cystitis occurs in a chronic form, an exacerbation of the pathology after intimacy is possible.
Often, patients turn to a gynecologist with a complaint that sometimes after sex they develop a feeling of cystitis.
In most cases, the main cause of this phenomenon is considered to be ineffective treatment.
Or incomplete therapy for previously diagnosed acute inflammation.
In addition, a violation of the rules of personal hygiene can serve as a provoking factor in the development of the inflammatory reaction.
If thrush and cystitis develop after sex, you should be thoroughly examined by a gynecologist and complete the entire course of therapy prescribed by the doctor.
It should also be noted that in case of thrush due to cystitis, both partners undergo treatment.
To avoid re-transmission of candidiasis and inflammation.
If signs of cystitis do not disappear after a few days, it is recommended to undergo a medical examination.
This is especially important for patients who are pregnant or currently undergoing fertility treatment.
What causes the disease
The main reason is the structural features and location of the urethra (urethra). In women, this organ has a shorter and wider structure than in men. This makes it easier for pathogenic microorganisms to enter.
In addition, the external opening of the urethra is located close to the vagina and anus. Sexual friction leads to its displacement into the vagina, which also contributes to infection and inflammation.
Intimate filling is used to eliminate the cause of postcoital cystitis
Additional provoking factors include:
- wearing thongs and synthetic tight underwear;
- a large number of sexual partners or their frequent change;
- improper hygiene care before and after sex;
- presence of gynecological diseases;
- frequent use of spermicidal contraceptives;
- “dry” sex, that is, intimacy without a sufficient amount of natural lubrication.
The risk of developing the disease increases many times if a woman has hormonal disorders or metabolic problems.
Diagnosis of cystitis
Diagnosing cystitis is not difficult, especially in the acute phase of the disease.
To confirm the diagnosis, the doctor may prescribe some diagnostic measures:
- Urinalysis according to Nechiporenko. Diagnostics will give a detailed result regarding the presence of an inflammatory process and the presence of certain formed elements - leukocytes, erythrocytes.
- Urine PCR. Prescribed to determine the causative agent of bladder inflammation and concomitant STIs. The analysis is prescribed in extreme cases, since the most informative diagnosis is a smear from the vagina or urethral canal.
If pyelonephritis is suspected, additional examinations are necessary to rule out serious complications.
For example, imaging methods such as ultrasound or excretory urography (x-ray of the urinary tract).
In case of recurrent inflammation or the appearance of cystitis after each sex, cystoscopy is prescribed.
Cystoscopy is an important diagnostic test.
In this case, the urologist can visualize and evaluate the inside of the urethra and bladder using a special endoscope.
The device is a catheter with an optical system.
It has an eyepiece.
Allows direct observation of the bladder.
Also connect to a special camera, enlarge the image and record the diagnostic results on DVD.
It is necessary to note that diagnosis is not carried out in the presence of an acute phase of cystitis.
TOP 8 main hygiene mistakes before, during and after sex
It would seem, what kind of omissions can adults and civilized people make when it comes to intimate relationships? You will be surprised, but many problems of the genitourinary system are often provoked precisely by the negligent attitude towards hygiene that both partners allow themselves. We bring to your attention a selection of the eight most common mistakes that can spoil your well-being and mood for a long time after an intimate date.
Go to the toilet a little before sexual intercourse.
Some girls try to visit the toilet before making love. Their motivation is quite clear. However, from a hygiene point of view, this is not worth doing! The fact is that urine leaves a woman's body through the urethra, a short tube located directly above the entrance to the vagina. When you pee before sex, you open the door for bacteria from the vagina and rectum to enter the urethra and bladder. Urologists and gynecologists advise going to the toilet after intimacy. This will not give bacteria a chance to rise up the urethra and provoke the development of cystitis and other unpleasant diseases.
Ignore water procedures before going to the bedroom.
Often, both partners are too excited to think about little things like washing their hands together before sex. This is a serious mistake! If you do not take care of hand hygiene, you risk introducing fungal infections into the vagina and urethra. Remember that “hand washing” is an item that both partners must do. “What about the shower,” you ask? In principle, this rule of hygiene is so obvious that it is somehow awkward to talk about it. Of course, before going to bed, it is important to take a shower, or at least use a bidet. Tight underwear, hair, a sedentary or, on the contrary, active lifestyle provoke the growth of bacteria and cause an unpleasant odor in the bikini area, even in healthy people. You can use intimate hygiene products or mild soap to care for this area.
Do not use condoms during all types of sex.
If you and your partner feel the difference between sex with and without a condom, then you will have to make an effort. A condom can protect both of you from most sexually transmitted diseases (STDs). It's not just about vaginal sex. Few people like oral sex with a condom, but it should be remembered that there is a whole “bouquet” of ailments that a man can get from his partner if he ignores this method of protection. Sore throat, scarlet fever, caries, herpes on the lips, inflammation of the upper respiratory tract, ARVI... Impressive, isn't it? We recommend purchasing special condoms for oral sex. They have pleasant tastes and will reliably protect against pathogenic bacteria that can provoke inflammatory diseases of the genitourinary system and microflora disorders.
Have unprotected sex during menstruation.
Doctors have an ambiguous attitude towards sex during menstrual periods. If you and your partner perceive this process positively, then, in principle, you can afford such exotic things. But there are several restrictions: be sure to use condoms and wash your hands thoroughly before and after intercourse. The fact is that during menstruation the cervix opens slightly, which increases the risk of contracting STDs and fungal infections many times over. Men are also at risk when they have unprotected sex with a woman these days—discharge can get into the urethra and cause inflammation.
Wash and store sex toys incorrectly.
Those who want to make their intimate life bright and varied cannot do without toys from a sex shop. It is important to clean them thoroughly after each use, following the instructions and storing them in a special case or box. Bacteria, fungi and infections can remain on the surface of gadgets for adults! During your next sexual intercourse, you and your partner may become infected with them if you ignore the hygiene rules.
Practice vaginal sex immediately after anal sex.
It’s no secret that all kinds of bacteria “live” in the rectum. If you do not follow the “safety rules” during anal sex, they can penetrate the vagina and cause serious problems. Be sure to use a condom and change it after each change of location. It is best for both of you to wash yourself thoroughly with soap after anal sex, if vaginal sex is also planned.
Don't shower after sex.
The vagina cleans itself after intimacy, so there is no need to douche after sex or use any harsh cleansers. But it won't hurt to take a shower or wash yourself. This way you can avoid developing yeast or bacterial infections. If it is not possible to carry out this simple cleanliness ritual, at least use special wipes for intimate hygiene.
Put on underwear immediately after making love.
Doctors do not recommend wearing panties, especially synthetic ones, immediately after intimacy. This material provokes a “greenhouse effect”. Allow the genitals to get rid of excess moisture by providing free access to air. If your butt is cold, wear cotton panties.
Ignore examinations by specialized specialists.
It is important for both you and your partner to undergo examinations from specialized specialists from time to time and be tested for major sexually transmitted diseases. Unfortunately, many infections are hidden, especially among the stronger sex. Being a carrier of the disease, a man may not even suspect it due to the absence of obvious symptoms and ailments. Remember that most delicate diseases can be cured without consequences if they are diagnosed at an early stage. Experts strongly recommend using condoms until you are both sure that you are healthy. This attitude towards intimate life is guaranteed to save your health, material resources and nerves!
Do you have doubts about intimate health? We recommend making an appointment with experienced and tactful medical specialists.
.
A gynecologist and urologist will be happy to answer the most unexpected questions related to sexual hygiene. With us, if necessary, you can quickly pass all tests. check the doctors' schedule and make an appointment with them by calling (0512) 777-888
.
When to do cystoscopy for cystitis
There are many reasons why your doctor may recommend that you get tested:
- In cases where there are symptoms of infection/inflammation of the lower urinary tract, which are accompanied by increased frequency of urination, dysuria, nocturia. Diagnosis helps assess the capacity of the bladder and the amount of urine that can remain in it after urination.
- In the case of macroscopic hematuria, the study can diagnose various pathological conditions of the bladder: the presence of stones, sand, neoplasms.
- Bladder cystoscopy is also used during some urological procedures, such as ureteral catheterization.
Treatment of cystitis after sex
In most cases, cystitis is a consequence of the penetration of bacterial microflora into the organ.
For simple cystitis, a three-day course of treatment is sufficient.
Therapy uses antibiotics to suppress the activity of gram-negative bacteria.
First of all, antibiotics of the fluoroquinolone group are preferred.
Fluoroquinolones have a secondary bactericidal effect and inhibit the activity of proliferative pathogens.
For urinary infections, Norfloxacin (Noroxin, Sophasin) is most often prescribed.
The drug is a medicine from the group of gyrase inhibitors (fluoroquinolones), which are used as a broad-spectrum antibiotic.
For cystitis, the drug is prescribed 2 capsules twice a day, for 5-7 days.
As an alternative, Azithromycin can be used for a short course (3 days) or Macropen 1 tablet 3 times a day, 5-7 days.
If cystitis recurs and the cause is the same bacteria, a long antibacterial course of treatment is prescribed (from 14 to 20 days).
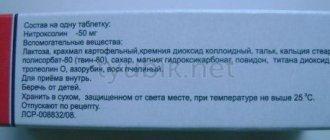
Nitrofurantoin may also be prescribed for bladder treatment.
It is an antibiotic drug used for the pharmacological treatment of bacterial urinary tract infections (urethritis, cystitis).
A particular advantage is the extremely wide spectrum of bactericidal activity.
In the acute phase of cystitis, anti-inflammatory drugs and painkillers may be recommended.
In case of severe pain, Nemisil can be used.
This drug belongs to the NSAID group and is recommended for use for no more than three days.
You can use Ibuprofen or Panadol as a replacement.
How to understand that you have postcoital cystitis
The first painful manifestations appear the next day after sex or 2 days later. Sometimes the disease is accompanied by rare episodes and goes away on its own, but in most cases cystitis is prone to relapse. The chronic course is characterized by the appearance of painful symptoms every time after sex.
Symptoms of the disease may be:
- Frequent urge to urinate.
- Urine is released in small portions.
- Discomfort in the lower abdomen.
- Pain, burning sensation when going to the toilet.
Deterioration in general health rarely occurs. In most cases, no increase in temperature is observed. Women often complain of a false urge to go to the toilet, and there is also increased pain at the end of urination.