MYELITIS
(
myelitis
; Greek myelos bone marrow + -itis) is an inflammation of the spinal cord, usually involving most of its diameter, affecting both gray and white matter. Inflammation limited to several segments is designated as transverse M. In diffuse (disseminated) M., the lesions are localized at several levels of the spinal cord. A special variant of M. is subacute necrotic M., described by Foix and Alajouanine (Ch. Foix, Th. Alajouanine) in 1926.
Etiology
In most cases, the cause of isolated inflammation of the spinal cord cannot be determined. M., arising as part of acute or subacute disseminated encephalomyelitis (see), may be caused by a neurotropic virus; scattered M., in which the lesion is limited only to the spinal cord, is very rare. In case of encephalomyelitis complicating mononucleosis, herpes zoster, leptospirosis, typhus and brucellosis, penetration of a specific pathogen into the nervous tissue should be assumed. Encephalomyelitis can also occur with measles, mumps and chickenpox. Neurol, complications observed in the first days of the disease are associated with direct viral damage to the brain, and complications that develop after 10-14 days are allergic in nature. Disseminated encephalomyelitis caused by rabies and smallpox vaccinations is also allergic. Syphilitic M. is extremely rare. Bacterial M. can occur with meningococcal and other purulent meningitis, with osteomyelitis of the spine and penetrating wounds (traumatic M.). Hematogenous introduction of a pyogenic infection into the spinal cord is also possible. Acute damage to the diameter of the spinal cord can sometimes be the first manifestation of multiple sclerosis (see). The cause of subacute necrotic M. is either thrombophlebitis of the spinal veins or a congenital anomaly of the venous vessels of the spinal cord.
Myelitis - description of the disease
The pathogen and/or its toxins penetrate the spinal cord and provoke inflammation in the latter. In this case, the bodies and processes of nerve cells are affected, the membranes, nerve trunks and roots can be damaged.
In neurology, there are several types of spinal cord myelitis, each of which has its own symptoms, severity of manifestations and prognosis.
For example, neuromyelitis optica (neuromyelitis optica, Devic's disease (syndrome)) is not typical for childhood, and if it develops in children, then, unlike adults, it is relapse-free, single-phase, and also has a favorable prognosis.
On the other hand, before mass vaccination, children, much more often than adults, had a pathology such as polio, which is provoked by a special virus and has a high probability of death and disability.
A significant role in the development of secondary myelitis pathology in children is played by diseases common at this age: measles, whooping cough, chickenpox and others.
We advise you to study - Degrees of scoliosis
Pathological anatomy
Most often, the inflammatory process in M. is localized in the thoracic spinal cord. Upon examination, the affected area of the brain is swollen, hyperemic, and in the most severe cases, softening is noted - myelomalacia. Microscopic examination reveals inflammatory infiltration of the pia mater. The brain tissue is infiltrated with lymphoid cells, edematous, changes in nerve fibers and nerve cells of varying degrees and even their death are noted. The vessels of the affected area are thrombosed, and perivascular infiltrates are observed. With a purulent infection, the pathogen can be isolated from the lesion. In cases of disseminated encephalomyelitis in pathomorphology, the picture is dominated by a demyelinating process, apparently of an allergic nature. In later stages, a connective tissue and glial scar is formed at the level of the lesion. In subacute necrotic M., at autopsy, extensive foci of necrosis, cavities, and often thrombosis of the superficial and deep veins of the spinal cord are found.
Clinical picture
M. occurs acutely or subacutely, often against the background of general infectious symptoms (fever, malaise, chills). Back pain appears, radiating to areas corresponding to the zones of innervation of the affected roots; Paresthesia may also occur in these same areas. Following the pain syndrome below the level of the spinal lesion, paralysis develops (see Paralysis, paresis), conduction disturbances of sensitivity and pelvic disorders. In the acute period, regardless of the level of damage, paralysis is sluggish: the tone in the paralyzed limbs is reduced, reflexes are difficult to evoke or are absent. However, already in the early stages of the disease the following are detected: usually Babinski's symptom (see Babinski reflex) or other pyramidal reflexes. With M. of cervical and thoracic localization, after a few days, flaccid paresis gradually transforms into spastic ones. As a rule, tissue trophism suffers, as a result of which bedsores quickly develop (see). In severe cases, M. is complicated by septicopyemia (see Sepsis). The entry points for superinfection are primarily bedsores and the urinary tract; in the cerebrospinal fluid there is usually an increased protein content and pleocytosis - neutrophilic in case of pyogenic infection and lymphocytic in cases of a viral or allergic nature of the disease. Queckenstedt's test (see CSF tests) usually reveals normal patency of the subarachnoid space; Only occasionally is a block detected, caused either by a sharp swelling of the spinal cord (edematous, pseudotumorous M.) or by an adhesive process. The course of the disease may vary. In favorable cases, after the acute period has passed, the process stabilizes, and subsequently spinal symptoms regress to one degree or another. In some patients, the pattern of transverse spinal cord lesions persists for life. In the most malignant cases, an ascending progression of M. is observed, in which inflammation can spread to the brain stem; an example would be subacute necrotizing M. The disease is more often observed in older people. Wedge, the picture is characterized by increasing spastic-atrophic paresis of the legs, variable sensitivity disorders and pelvic disorders. Damage to the lower parts of the spinal cord and cauda equina can increase over several years, gradually spreading upward. The protein content in the cerebrospinal fluid is increased.
Classification
Have you been trying to heal your JOINTS for many years?
Head of the Institute for the Treatment of Joints: “You will be amazed at how easy it is to cure your joints by taking the product every day for 147 rubles...
We advise you to study - Reasons and timing for issuing sick leave for osteochondrosis
There are several types of myelitis, differing in symptoms, severity and prognosis. According to the severity of symptoms, they are distinguished:
- Acute transverse myelitis;
- Subacute;
- Chronic.
Depending on the location of the lesion, myelitis is distinguished:
- Limited, or focal - develops in separate areas;
- Disseminated, or scattered, or multifocal - affects several areas;
- Transverse - extends to several nearby segments;
- Diffuse or widespread - affects the entire brain.
Depending on the cause, myelitis occurs:
- Infectious (viral or bacterial) – develops when an infection enters the body;
- Traumatic – caused by injury;
- Toxic – provoked by toxic substances;
- Post-vaccination – a unique form that appears after vaccination;
- Radiation – caused by radiotherapy;
- Idiopathic - the cause cannot be determined.
Infectious myelitis, in turn, is divided into:
- Primary – develops under the influence of viruses that selectively infect nerve cells;
- Secondary – caused by other infections (measles, scarlet fever, syphilis, sore throat, erysipelas, pneumonia, sepsis).
A separate form of the disease is neuromyelitis optica. In this case, in addition to the characteristic symptoms, vision deterioration and even loss are observed.
Diagnosis
The diagnosis is made based on the presence of general infectious symptoms combined with the development of acute damage to the spinal cord. The greatest difficulty is in differentiating transverse M. from epiduritis (see Pachymeningitis), since their clinical picture is similar. The decisive role is played by myelography (see), which reveals in the case of an epidural abscess one or another degree of blockade of the subarachnoid space. In doubtful cases, laminectomy (see) is indicated to exclude epidural abscess, too late removal of which is fraught with irreversible damage to the spinal cord. A picture similar to M. can be given by malignant tumors of the epidural space and spinal stroke (see Spinal cord). Apoplectiform damage to the spinal cord caused by tumor metastasis is accompanied by significant emaciation of the patient, the appearance of an earthy coloration of the skin, anemization and a sharp acceleration of ROE. Spondylograms for metastases in the spine in many cases do not reveal destruction and their role in diagnosis is relatively small; metastatic disease is confirmed by the detection of visceral carcinoma. Spinal stroke - most often a heart attack, less often hematomyelia (see) - unlike M., is not accompanied by general infectious symptoms. In addition, the cause of most heart attacks is the pathology of the anterior spinal artery basin, and when it is turned off, a very characteristic wedge is observed, a picture in the form of damage to 2/3 of the spinal cord with the posterior columns intact. The presence of patol, reflexes, conduction disturbances of sensitivity and pelvic disorders make it possible to differentiate M. from Guillain-Barre polyradiculoneuritis (see Polyneuritis), characterized by the acute development of flaccid paralysis of the lower extremities, often tending to spread upward to the trunk, arms, and in some cases involve stem sections of the brain. If M. is formed as a component of acute disseminated encephalomyelitis, the diagnosis of the latter is facilitated by the presence of supraspinal symptoms. With neuromyelitis optica, the diagnosis does not cause difficulties if M.'s development is preceded by optic neuritis (see).
The connection between spinal cord lesions and multiple sclerosis is indicated by the presence of decoloration of the optic discs, nystagmus (see) and paralytic Lange curve in the cerebrospinal fluid (see) obtained during lumbar puncture.
Subacute necrotic M. is almost never diagnosed during life. Spinal lesion syndrome, clinically indistinguishable from subacute necrotizing M., can be observed with paraneoplastic neuropathy complicating visceral carcinoma (see Paraneoplastic syndromes).
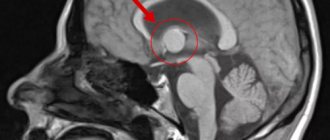
Diagnosis of myelitis
If myelitis is suspected, a mandatory procedure is a lumbar puncture to analyze the cerebrospinal fluid.
The presence of inflammation is indicated by its traces and the absence of protein. The same study allows us to detect the presence of microorganisms in the fluid, which means that the spine has become infected. In addition to the puncture, the patient is sent for magnetic resonance imaging or tomography using contrast. As a rule, one of these tests, chosen at the discretion of the doctor, is sufficient. Necessary measures are the use of suboccipital myelography and analysis to identify microorganisms and other pathogens in the cerebrospinal fluid.
Since myelitis can be the result of a large number of processes, it is necessary to carry out a differential diagnosis to accurately exclude diseases such as multiple sclerosis, spinal stroke, cystic arachnoiditis and other pathologies with symptoms that are similar at first glance.
In addition to these conditions, it is necessary to make sure that the patient does not have epiduritis, a disease with an equally similar clinical picture that requires surgical intervention. In difficult situations, additional research may be required when the doctor prescribes an exploratory laminectomy. Diagnosis of epiduritis involves studying the affected tissues for purulent foci, radicular pain and syndrome of increasing compression of the spinal cord substance, which distinguishes this disease from myelitis.
It is necessary to differentiate myelitis from acute Guillain-Barré polyradiculoneuritis, which differs from it in the absence of conduction disorders, disorders of the pelvis and spastic phenomena.
Spinal cord tumors that need to be excluded during diagnosis have their own characteristic differences: a slow course, a clearly defined stage of radicular pain, a block in liquorodynamic tests, protein-cellular dissociations in the cerebrospinal fluid.
Excluding hematomyelia and hematorahis, you need to know whether elevated body temperature is present among the symptoms, since it is its absence, combined with a sudden onset and rapid development, that is a sign of these diseases. Hematomyelia causes damage to the gray matter, and when there is hemorrhage under its membranes, the patient experiences meningeal symptoms. Such pathologies often develop as a result of injuries.
Acute transverse lesion requires the exclusion of cerebrospinal circulatory disorders and multiple sclerosis, although the latter is always accompanied by such signs as damage to the white matter in certain areas, diffuse damage not only to the spinal cord, but also to the brain, and a decrease in the intensity of symptoms after a few days.
Myelitis also needs to be differentiated from chronic meningomyelitis, which is characterized by slow progression at normal temperatures. Meningomyelitis is caused by syphilis, detected using serological tests.
Treatment
Hospitalization is required. For viral and allergic M., as well as for M. of unknown nature, massive doses of glucocorticoid hormones are prescribed - up to 100-120 mg of prednisolone orally per day. After a few days, the dose is gradually reduced. The duration of hormonal therapy is determined by the dynamics of the disease. Vigorous dehydration therapy (Lasix, Uregit, mannitol) is also indicated. Antibiotics are prescribed from the first days of illness to prevent superinfection. For purulent M., antibiotics are required in the highest possible doses. Constant skin care and regular bladder catheterization are required. Symptomatic remedies are vitamins, analgesics, amidopyrine and other pyrazolone derivatives. After the acute period has been eliminated, rehabilitation is necessary: exercise therapy, massage, physiotherapy, for spastic paralysis - Elenium, Seduxen, Mydocalm.
The prognosis depends on M.'s etiology and its severity. Pyogenic M. usually have an unfavorable outcome. The prognosis is also very poor for ascending forms of M. However, the use of artificial ventilation allows saving the lives of some patients. Massive damage to the diameter of the spinal cord is often complicated by septicopyemia, which significantly aggravates the prognosis. M., which occurs as part of acute disseminated encephalomyelitis, usually proceeds favorably. As a rule, there is a significant restoration of spinal functions.
Bibliography:
Bogorodinsky D.K. and Skoromets A.A. Spinal cord infarctions, L., 1973, bibliogr.; Kreimer A. Ya. and Goldelman M. G. Clinic and complex therapy of diseases of the nervous system, p. 138, Tomsk, 1978; Lobzin V.S. and Sichko Zh.V. Rom-boencephalitis and myelitis in mumps, Zhurn, neuropath, and psychiat., t. 75, No. 2, p. 178, 1975, bibliogr.; Melnichuk P. V., Il and N and N. A. and Shtulman D. R. Emergency care for neurological diseases, p. 57, M., 1978; Multi-volume guide to neurology, edited by S. N. Da-videnkova, vol. 3, book. 1, p. 131, M., 1962, bibliogr.; Granata F. ea Su di un caso di mielite tranversa insorta dopo vacci-nazione anticolerica, Acta neurol. (Napoli), v. 29, p. 511, 1974; H o 1 t S. ao Diffuse myelitis associated with rubella vaccination, Brit. med. J., v. 2, p. 1037, 1976; Hughes JT Pathology of the spinal cord, L., 1966; N iko 1 i with M. a. L evi with Z. Comparative analysis of the therapy of acute transverse myelitis, Paraplegia, v. 14, p. 184, 1976.
D. P. Shtulman.
At the level of the cervical spine
Pathology of the spinal cord at different levels is called myelopathy. Myelopathy of the cervical spine is a very serious process, because if it is affected, there is a high probability of death. Operations in this department are very dangerous; they are carried out only if the risk is justified by preserving human life:
- hernia between the vertebrae;
- myelitis;
- congenital pathologies;
- pinching;
- infection;
- injury.
The spinal cord is responsible for the optimal functioning of the nervous system. Of course, cervical myelopathy makes negative adjustments to it. Often neck myelopathy is accompanied by the following symptoms:
- the appearance of severe pain in the neck, in the back of the head, between the shoulder blades;
- muscle spasms occur;
- arms become weak;
- upper limbs twitch involuntarily;
- the skin of the hands and neck becomes numb.
Myelopathy therapy requires very serious treatment! If you thinklessly treat this disease, then irreversible changes will begin in the body. Complete atrophy of the spinal cord will occur, paralyzing the limbs. And it will be almost impossible to restore their previous activities.
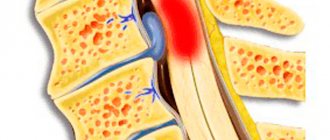
Acute disc protrusion
Protrusion of the cervical spine occurs when the supply of nutrients to the intervertebral discs is disrupted. If the power needed for normal operation is missing, then serious changes begin:
- the structure of the core changes (the jelly-like state becomes very dense);
- the fibrous membrane loses its elasticity;
- the core cannot remain in its normal position;
- the disc begins to shift, extending beyond the vertebrae;
- depreciation deteriorates.
If the disc protrudes beyond the vertebrae even by one millimeter, then there may be unpredictable consequences. It is possible that compression of the nerve roots and arteries of the spine will occur, which will lead to inflammation, pain and poor circulation. Protrusion has symptoms that depend on how much the disc has protruded and the degree of compression of the nerve roots:
- mobility is limited;
- pain in the cervical region;
- neck muscle spasms;
- tingling feeling;
- weakness of muscle tissue in the arms;
- numbness;
- edema;
- my hands hurt, namely their muscles.
Hydromyelia
This is a congenital pathology characterized by an expansion of the spinal cord canal. It affects its trunk and cervical region. Hydromyelia is often accompanied by hydrocephalus. The main reason for its appearance is a congenital anomaly of the canal. Enlargement of the spinal cord canal occurs and develops secondary to the influence of certain pathological changes in the body. Often secondary hydromyelia develops due to the formation of excess fluid, which occurs when the spinal cord is compressed or a cerebellar tumor.
The spinal canal in this disease is lined with ependyma, the boundaries of the canal are expanded from the outside, and fluid from the inside. The development of hydromyelia is often provoked by thinning of the posterior columns of the spinal cord.
It happens that the congenital defect is accompanied by diseases such as lateral aperture of the 4th ventricle, median atresia and internal hydrocephalus. Hydromyelia usually occurs without symptoms. This disease is treated only after identifying the cause that provoked it. It can be completely eliminated through surgery.
We advise you to study – Belt for back posture