The concept of “coma” is quite broad and represents a set of symptoms. Most often they talk about coma when a person is unconscious and often does not respond to external stimuli. In severe cases, this condition leads to death - usually they talk about such risks in a IV degree coma.
In this case, there are two types of coma - natural and artificial. Moreover, mentions of the second are often found in various medical news. But what is the difference between these two types?
Between life and death. How does a person in a coma feel? More details
Life in a coma
A state of prolonged absence of consciousness is accompanied by the disappearance or sharp weakening of the reaction to external stimuli, extinction of reflexes, disturbances in the frequency and depth of breathing, and changes in vascular tone. The pulse also quickens or slows down greatly, and temperature regulation is disrupted.
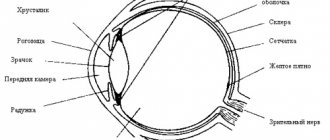
Coma develops when the brain is damaged, which causes acute circulatory disorders. As a result, deep inhibition occurs in the cortex - it spreads to the subcortical sections of the victim’s central nervous system.
Causes of coma:
- head injury - leads to swelling of the brain or hemorrhage into it;
- oxygen starvation (hypoxia) - caused by drowning, suffocation, as well as cardiac arrest;
- stroke - leads to cessation of blood supply to the brain stem or to swelling;
- a sharp change in blood sugar levels in diabetic patients;
- infectious damage to the central nervous system - meningitis or encephalitis;
- poisoning of the body by decay products - occurs when the systems or excretory organs fail as a result of poisoning or disease;
- epileptic seizures - when repeated after a short period of time.
There is also a medically induced coma. It is induced by doctors to protect the body from disorders that negatively affect the activity of the cerebral cortex - hemorrhages with further swelling. Artificial coma is also used as an alternative to anesthesia during neurosurgical operations or when recovering from status epilepticus.
Coma may develop gradually or occur suddenly. The period of entry into this state ranges from several minutes to several days.
Coma depth gradation:
- Precoma - severe retardation or psychomotor agitation. Reflexes are preserved, but coordination of movements and the thought process are impaired.
- 1st degree - there is sleep or stupor, reactions to external stimuli are inhibited, but the patient can take liquid food and perform simple movements.
- Stage 2 - deep sleep, complete lack of contact, pathological forms of breathing, rare chaotic movements, weakened reaction of the pupils to light, spastic contractions and muscle fibrillation.
- 3rd degree (atonic) - lack of consciousness and reaction to pain, depression, loss of reflexes, arrhythmic breathing. Convulsions are possible, blood pressure and body temperature decrease.
- 4th degree (exorbitant) - complete absence of reflexes, muscle atony, a sharp decrease in pressure and temperature. The medulla oblongata does not function, spontaneous breathing stops. The patient's condition is maintained with the help of an artificial lung ventilation device (ALV) and parenteral (injection) nutrition.
Most often, death occurs in an extreme coma. But if the patient can be brought out of this state within half an hour and there are positive dynamics in the future, then complete or partial restoration of brain functions is possible.
Features of the use of artificial coma
Introducing the patient into a state of medicated sleep is carried out exclusively in the intensive care unit. The patient is under constant supervision of medical personnel.
To introduce the patient into a state of medicated sleep, the following is used:
- hypnotics used for short-term anesthesia (propofol allows you to put the patient into a state of medical sleep for several hours, and due to its short-term action it has the lowest risk of complications);
- tranquilizers benzodiazepines (diazepam preparations allow you to put the patient into medicated sleep for up to three days);
- barbiturates (provide the best neuroprotective effect for head injuries or strokes, and also help prevent the development of cerebral edema).
The patient's breathing in a state of medicated sleep is supported by ventilation. All functions of internal organs are constantly monitored using hardware and laboratory diagnostics (electrocardiogram, electroencephalogram, blood biochemistry).
For reference. With prolonged drug-induced sleep, the patient is transferred to parenteral (intravenous) nutrition. Mandatory prevention of the development of bedsores and concomitant bacterial infections is also carried out.
Use in resuscitation therapy
An artificial coma is often performed for pneumonia, when acute respiratory failure develops against the background of pneumonia. More often, such pathologies are detected in patients with complicated influenza, who quickly develop viral or bacterial pneumonia and respiratory distress syndrome (a life-threatening condition characterized by diffuse infiltration and hypoxemia - a decrease in the concentration of oxygen in the blood).
Patients are placed in the intensive care unit, where they are sedated with medication and connected to a ventilator. In some cases, patients may remain in this condition for longer than 2 weeks. Typically, the drugs used for sedation are sodium oxybutyrate and benzodiazepines, and for muscle relaxation - Pipecuronium bromide.
In the case of an ischemic stroke , the patient is placed in an induced coma if a large lesion is detected, which is associated with a high risk of progression of neurological disorders - this measure in some cases can improve the outcome of stroke. Severe traumatic brain injuries resulting from an accident, bruise, or attack are associated with acute disruption of blood flow, cerebral edema, dislocation and compression of the brain matter.
For reference. If the patient lies in a coma, cerebral edema decreases, which often leads to stabilization of brain functions; how long the patient needs to remain in this state will be determined by the attending physician. Medication-induced sleep after complex neurosurgery reduces the risk of brain damage.
Often, a comatose state develops spontaneously as a protective reaction of the body to a negative external influence - head injury, impaired cerebral blood flow, taking a large dose of alcohol or a narcotic substance, impaired respiratory and cardiac activity due to complicated, acute somatic pathology.
Your doctor will tell you how to get out of a coma in such cases. Typically, therapeutic measures are reduced to maintaining the vital functions of the body.
The patient regains consciousness on his own or enters a vegetative state (minimal consciousness). The patient can fall asleep and wake up, swallow food, blink, but does not respond to speech at all, does not speak, and does not walk independently.
The duration of the vegetative state, like the coma itself, is difficult to predict. It can last for years and even a lifetime.
Features of carrying out in childhood
Psycho-emotional reactions of patients often complicate the treatment process and negatively affect recovery. Drug sedation as an alternative to local anesthesia is indicated for some types of dental treatment. Painful manipulations, stress, and unfamiliar surroundings negatively affect the child’s psycho-emotional status.
Usually in such cases, adequate doses of hypnotics (hypnotics) or anxiolytics (tranquilizers, psychotropic drugs that eliminate anxiety) are administered. The disadvantage of sedation is that children are unable to answer important questions during sleep that the doctor may have during treatment.
For reference. Deep medicated sleep is indicated in cases where a child is connected to a ventilator. The procedure of tracheal intubation (insertion of a breathing tube into the tracheal cavity) and the lack of speech contact cause discomfort and fear in pediatric patients, which is accompanied by an increase in the concentration of cortisol, a hormone involved in the development of stress reactions.
In parallel, reactions such as increased blood pressure, increased heart rate, and tachypnea (rapid, shallow breathing) occur. In these cases, sodium thiopental or Midazolam is usually used.
Patient's feelings
A patient in a vegetative state is quite capable of perceiving external stimuli. What a person feels is known from the stories of those who came out of a coma. They claim that the sensations were akin to a dream. There are no memories even of extreme situations - heart attacks and other critical disorders in the body. Many people report that while in a coma they see a pipe with a light at the end. But the testimonies of patients differ quite greatly.
Usually a person has no idea what happened to him, where and why he is. After a coma, the patient will receive many revelations: information about the current date and a description of the course of the disease.
It is a common misconception that a person in a coma can hear or feel what is happening around them. Although it is possible that he senses certain things at the subconscious level.
Thus, the UK Department of Health recommends:
- When visiting a patient, introduce yourself to him and convey positive news.
- Tell how the day went, as if the patient were receiving the information.
- Keep in mind that everything said can be heard by a person who is in a coma.
- To express your support to the patient, even just sitting next to him and holding his hand is enough.
- Let me listen to my favorite music on headphones.
To bring a patient out of a vegetative state, doctors may need many attempts, and the process itself takes an indefinite amount of time.
The rehabilitation period after leaving a coma must be carried out under the supervision of doctors, otherwise it may be prolonged or develop negative dynamics. It is recommended to take advantage of a rehabilitation course at a specialized center.
How to be brought out of an induced coma
Bringing a patient out of an induced coma is an extremely complex procedure that requires special training. The administration of medications that support the patient's medicated sleep is stopped gradually.
Relatives of the patient need to understand that recovery from a coma and further rehabilitation can last many months.
The patient's consciousness is restored gradually, periods of delirium, memory impairment, speech impairment and motor activity are possible.
For reference. During rehabilitation, patients gradually learn to eat, get out of bed, and walk on their own. Restoring memory, speech and motor activity can take from several months to a year.
How does nutrition happen?
The patient is provided with food enterally (through the gastrointestinal tract) or parenterally (intravenously), and combined nutrition is also organized.
When using a probe, liquid and semi-liquid (cream-like) products are served. They go directly to the stomach. Dense dishes are ground and diluted taking into account the nature of the mixture - boiled water, tea, broth, vegetable decoctions, milk, juices and other components are used for this.
Parenteral nutrition involves the intravenous administration of nitrogenous drugs, energy substances, and saline solutions in quantities that are necessary to maintain the strength of a person in a coma. First, a daily infusion program is developed, which indicates the method and sequence of drug administration, as well as the volumes of solutions, the rate of infusion and the necessary drug additions. To monitor the patient's condition, control laboratory tests are regularly carried out.
How to determine that a patient has died
The patient's condition is monitored using laboratory tests: blood tests, coagulation tests, determination of the content of electrolytes, toxic substances in serum and urine, and the state of cerebrospinal fluid.
The cause of brain pathology is determined clinically through a careful history and physical examination. Diagnostic imaging studies using computed tomography or magnetic resonance imaging are done to prove that brain damage is irreversible. In some cases, cerebral angiography is used.
Death is characterized by the absence of any visible signs of brain activity. A lethal outcome is recorded if the patient does not respond to external stimuli (including pain) and does not show signs of brainstem activity. It is necessary to exclude pharmacological neuromuscular blockade - for this purpose, history data or stimulation of peripheral nerves are used.
There are two types of tests that confirm brain death: the disappearance of bioelectrical activity (measured using electroencephalography, sensory evoked potentials, brainstem auditory evoked response) and cessation of blood flow, which is determined by pancerebral angiography, scintigraphy, transcranial Dopplerography.
Even with intensive cardiovascular support, most patients die within two days of brain death.