Causes of nystagmus
Most often, nystagmus occurs in people suffering from the following diseases:
- Meniere's disease: a disease of the inner ear of unknown origin that has only symptomatic treatment.
- Intracerebral hemorrhage is a dangerous condition that requires emergency medical attention. The formation of an intracerebral hematoma is usually caused by a ruptured arterial aneurysm or stroke.
- Myasthenia gravis is a neuromuscular disease accompanied by weakness of skeletal muscles, including damage to the oculomotor system.
- A concussion is a medical condition that can cause severe symptoms and requires medical attention. With traumatic brain injury, a variety of symptoms of damage to the nervous system are observed.
- Alcohol withdrawal syndrome is a pathology that occurs when a person suffering from alcoholism sharply reduces or stops drinking alcohol.
- Hydrocephalus is the accumulation of fluid between the membranes of the brain, which leads to its compression and swelling.
- Wernicke-Korsakoff syndrome is a nervous system disorder associated with a lack of vitamin B1.
- Multiple sclerosis is a steadily progressive lesion of the central nervous system.
- Vitamin B1 deficiency is a lack of vitamin B1, found in milk, legumes, vegetables, meat and whole grains.
- Neuroblastoma is a rare form of malignant tumors that primarily affects the sympathetic nervous system and is more common in children.
- Labyrinthitis is an inflammation of the part of the inner ear responsible for the sense of balance and body position in space.
- Acute cerebellar ataxia is a pathology of the part of the brain responsible, among other things, for balance and coordination of movements.
- Abetalipoproteinemia is a hereditary disease in which the body does not absorb certain dietary fats.
- Albinism is a rare genetic disease accompanied by hypopigmentation of the skin, hair, eyes and visual impairment.
- Chediak-Higashi syndrome is a rare type of albinism that primarily affects the visual organ.
Idiopathic nystagmus is often observed, the cause of which cannot be identified. In this case, disorders of the brain can only be functional in nature, which means they will not be visible on MRI or CT images.
As a rule, nystagmus is not inherited. The exception is when this symptom is part of a genetic disease.
If nystagmus is detected in a child, first of all, ophthalmological pathology is excluded, for example, Leber's amaurosis, other hereditary diseases of the retina, tumors, retinopathy of prematurity, and color blindness. Of the systemic diseases, the cause of nystagmus in children is most often albinism. In addition, this is a sign of some neurological diseases, such as cerebral palsy.
If nystagmus is not congenital, but appears six months or more after birth, research is necessary to rule out brain tumors. The same must be done if nystagmus acquires uncharacteristic signs:
- episodic or unilateral;
- eyeballs move in different directions;
- there are headaches, convulsions, and developmental delays.
In clinical practice, the most common vestibular nystagmus is caused by damage to the inner ear or parts of the brain responsible for balance and coordination. In addition, this symptom is often observed in diseases of the extraocular muscles.
Timely detection and treatment of nystagmus in children and adults is a necessary condition for maintaining normal vision or coordination of movements.
Nystagmus in children
Immediately after the birth of a child, it is impossible to immediately diagnose nystagmus, since newborns are characterized by a lack of gaze fixation on an object. If at the age of 1-1.5 months the baby does not fix his gaze on the toy, the ophthalmologist may suspect eyeball nystagmus in the child.
This can definitely be said in the second or third month of a child’s life. In the first year of life, the visual apparatus is still developing, so babies are not diagnosed with “eyeball nystagmus” until they are one year old; until this age, it is not considered a deviation. If there are compelling prerequisites for making this diagnosis, a neurologist and an ophthalmologist monitor the child’s health.
Possible causes of nystagmus in children:
- Pathology of intrauterine development;
- Birth injury;
- Albinism.
To preserve the child’s visual acuity, he is carefully examined, special glasses and other complex measures (hardware and surgical treatment) are prescribed. If treatment is carried out correctly and in a timely manner, visual acuity in children does not deteriorate.
Symptoms of nystagmus
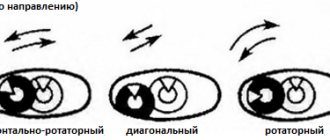
Nystagmus is rapid uncontrolled eye movement. Depending on the direction, horizontal, vertical, rotational and diagonal nystagmus are distinguished. Most often, horizontal movement is detected.
The amplitude of oscillations can be the same in both directions, and then they speak of pendulum-like nystagmus. Sometimes the fast phase of nystagmus prevails over the slow one, and in this case the patient is forced to turn his head in the direction of rapid movements of the eyeballs. At the same time, the weakness of the extraocular muscles is compensated, and the range of eye movements decreases. If the head is turned to the left, there is weakness in the external rectus muscle of the left eye and the internal rectus muscle of the right eye, and the nystagmus itself is called left-sided.
There is also a mixed type, when one patient has both pendulum-like and jerky eye movements.
The amplitude of eyeball movements during nystagmus can be different:
- if it is more than 15°, they speak of sweeping or large-caliber nystagmus;
- with a deviation within 5 - 15°, the nystagmus is considered medium-caliber;
- if the deviation angle is less than 5°, this is minor nystagmus.
Finally, this sign can be detected when the patient looks straight ahead, or towards the fast or slow phase.
Diagnostics
Diagnosis of the disease is carried out by two specialists: an ophthalmologist and a neurologist. After a detailed interview with the patient, the first one checks the visual functions and determines the type of nystagmus, and the second one looks for the cause of the pathology. The following diagnostic methods are usually used:
- study of visual potentials;
- examination of the fundus and retina (ophthalmoscopy, retinography);
- electronystagmography;
- CT and MRI;
- various blood tests, etc.
In some cases, consultation with an otolaryngologist and neurosurgeon is required. A complete examination usually takes about two weeks.
When the severity of the disease, its causes and main symptoms are identified, a final decision is made regarding treatment tactics. It should be noted right away that the horizontal type, like any other, is extremely difficult to cure. The therapeutic process is complex and lengthy, but not always effective.
Dependence of characteristics of nystagmus and accompanying diseases
Spontaneous nystagmus found under normal conditions is almost always vestibular. Its name is determined by the direction of the fast phase, that is, the side where the eyeballs move faster than they return to their normal position.
- With horizontal eye movement, the doctor should suspect a pathology of the inner ear (labyrinth) or the middle parts of the rhomboid fossa of the brain.
- If the eyes move upward or diagonally, this may be a sign of damage to the upper part of the rhomboid fossa.
- Rotational nystagmus occurs when the lower part of this part of the brain is affected.
- Converging (converging) nystagmus is observed in diseases of the midbrain.
Horizontal rapid eye movement, sharply predominant in only one direction, occurs with unilateral damage to the labyrinth or brain. It occurs with purulent unilateral labyrinthitis, thrombosis of its artery, a crack in the pyramid of the temporal bone, or a tumor of the vestibulocochlear nerve.
On the contrary, a significant predominance of the slow phase, especially in combination with floating eye movements, is a sign of serious illnesses: stroke, traumatic brain injury, meningitis or encephalitis, tumor, sharp increase in intracranial pressure.
Spontaneous unilateral nystagmus occurs in diseases such as damage to the oculomotor nerve or brain stem.
To treat nystagmus in children or adults, an accurate diagnosis of its causes and types is necessary.
General characteristics of the disease
Nystagmus is a spontaneous oscillatory movement of the eye.
The following types of nystagmus are distinguished:
- pendulum-shaped, clonic (push-like) and mixed;
- in direction - horizontal, vertical, rotatory and diagonal (the direction is assessed by the fast phase of oscillations);
- in scope - large-, medium- and small-scale (oscillations are 15°, 10°, 5°, respectively).
The frequency of oscillatory movements can exceed several hundred per minute. Acquired nystagmus is always accompanied by blurred visual perception (although central vision may be high) and dizziness, while congenital nystagmus does not cause dizziness.
Nystagmus, like paralysis, is based on central or local genesis.
The development of nystagmus can be caused by lesions of the cerebellum, pons, medulla oblongata, second frontal gyrus, roof plate (quadrigeminal), pituitary gland and some other parts of the cerebrum due to inflammatory and tumor processes or vascular disorders.
On the other hand, it can occur in connection with low vision in both eyes due to opacities, anomalies of the optical media and changes in the choroid, retina and optic nerve.
With lesions of the central parts of the nervous system, cortical, vestibular, diencephalic, hysterical, and other types of nystagmus occur. Damage to the peripheral part of the visual or auditory analyzer causes optical and labyrinthine nystagmus.
There is also physiological nystagmus, which includes such types as optokinetic, labyrinthine and nystagmoid twitching (with extreme abduction of the eyes). As is known, based on optokinetic nystagmus, visual acuity can be checked in children and aggravants.
The study of labyrinthine nystagmus plays an important role, for example, in assessing the functional state of the vestibular apparatus in astronauts.
Treatment of nystagmus is difficult and often unsuccessful. All efforts are aimed at eliminating the common cause that caused it, which is the lot of many specialists.
All therapeutic measures that improve visual acuity (treatment of amblyopia, correction with glasses, reflexology, cataract extraction, keratoplasty, etc.), as well as restoring muscle tone, can lead to a decrease in nystagmus.
Surgical intervention on the muscles is effective mainly only with horizontal nystagmus.
Kinds
There are congenital and acquired nystagmus, which is determined by its cause. In addition, this condition can be triggered in a healthy person. These are the following types of nystagmus:
- caloric: appears when water is infused into the external auditory canal at a temperature of 25°, and then 19°; normally it appears after 30 seconds and is associated with warming and cooling of the sensitive cells of the labyrinth; with pathology, its characteristics change;
- rotational and post-rotation: occurs during rotation in a special chair and lasts up to 30 seconds after stopping; with pathology, this time is extended, or it does not occur;
- pressor: when pressing on the tragus of the ear, it does not normally appear, it is characteristic of the destruction of the walls of the labyrinth in chronic purulent otitis media;
- optokinetic: occurs after rotation of the special drum under study in front of the eyes and quickly passes; changes in its parameters indicate pathology of the posterior lobe of the brain.
Also, in a healthy person, when overtired, nystagmoid twitching of the eyeballs may occur when trying to focus on one object. This phenomenon is not considered a pathology. Some people are capable of causing nystagmus, which in this case is of the voluntary variety, through an effort of will.
Another type of nystagmus that can be detected in a healthy person is installation nystagmus. It occurs when the gaze is fixed as far as possible to the side, as a result of overwork of the oculomotor muscles.
Pathological types of nystagmus:
- professional, which occurs when working in harmful conditions with increased vibration, is observed, for example, among workers in the mining industry;
- congenital: observed when there is a violation of oculomotor regulation in the area of the brain stem, often combined with albinism, color blindness, congenital cataracts; it is usually diagnosed 1 – 1.5 months after the birth of the baby, when the child begins to fixate his gaze;
- latent: congenital form, manifests itself only when one eye is closed or special studies, is considered a sign of diseases of the brain stem;
- free: occurs when the gaze is fixed on one object or when this object approaches the eyes (during convergence); caused by tension in the oculomotor muscles;
- myoclonus: horizontal frequent (up to 13 per second) series of movements of the eyeballs, observed in acute encephalitis or damage to the cerebellum;
- myorhythmia of the soft palate with nystagmus: simultaneous twitching of the eyes and uvula of the palate with pathology of the dentate nucleus or olive - special brain centers;
- undulating: a type of congenital, manifests itself at the age of 1 - 1.5 years, accompanied by a rhythmic shaking of the head when looking in a certain direction; has a favorable course and usually stops after a year;
- nystagmus in the blind: caused by completely blind people being unable to coordinate gaze position;
- paroxysmal: appears periodically, usually serves as a symptom of epilepsy;
- dissociated: expressed differently in both eyes; if it occurs during fixation of gaze, it serves as a symptom of ophthalmoplegia or damage to the brain, in particular the cerebellum;
- alternative: characterized by a changing direction and amplitude of pathological eye movements, may be congenital or a sign of a tumor or other serious brain disease;
- with damage to the extraocular muscles: usually observed with myasthenia gravis, occurs when a healthy eye is closed, and is temporary;
- medicinal or toxic: associated with the effects of large doses of alcohol or barbiturates.
nystagmus
Nystagmus
(
nystagmus
; Greek nystagmos drowsiness) - rapidly repeating movements of the eyeballs (eye tremors). The following types of nystagmus are distinguished: vestibular, which occurs when the receptors of the vestibular apparatus are irritated, and optokinetic, which appears when the visual analyzer is irritated (looking at uniformly moving objects). Other types of nystagmus (professional, congenital, fixation and installation, voluntary) are also relatively rare.
Vestibular nystagmus is important for topical diagnosis and reflects the dynamic changes occurring in the c. n. With. and on the periphery. Nystagmus can be examined in a patient regardless of the severity of the condition, even in a coma.
Scheme of anatomical formations that provide conjugal reflex movement of the eyes and nystagmus (according to B. N. Klossovsky): 1 - labyrinth, 2 - vestibular part of the vestibulocochlear nerve, 3 - superior nucleus of the vestibulocochlear nerve, 4 - commissural fibers between the superior nuclei of the vestibulocochlear nerve -cochlear nerve, 5 - ascending uncrossed vestibuloculomotor connections as part of the posterior longitudinal fasciculus, 6 - nucleus of the oculomotor nerve, 7 - lateral rectus muscle of the eye, 8 - superior rectus muscle of the eye, 9 - inferior rectus muscle of the eye, 10 - medial rectus muscle eyes, 11 - ascending crossed vestibuloculomotor connections from the medial vestibular nucleus as part of the posterior longitudinal fasciculus, 12 - nucleus of the abducens nerve, 13 - medial vestibular nucleus.
The anatomical structures with the help of which vestibular N. is carried out are the neuroepithelium of the ampullae of the semicircular canals, the vestibular node, the vestibular part of the vestibulocochlear nerve, the vestibular nuclei at the bottom of the fourth ventricle, crossed (for horizontal Nystagmus) and uncrossed (for vertical Nystagmus) vestibuloculomotor pathways running in an ascending direction at the bottom of the IV ventricle to the nuclei of the oculomotor (VI) and abducens (III) nerves (Fig.). Through the vestibuloculomotor connections passing in the posterior longitudinal fasciculus, vestibular impulses reach the eye muscles. In the same way, reflex combined deviations of the eyes occur, as a result of which the direction of gaze does not change when the position of the head changes, N. and compensatory adjustment of the eyes is carried out. The mechanism of vestibular N. is closely related to the mechanism of movement of the eyeballs. This connection is carried out through a complex system of the posterior longitudinal fasciculus. Some of its fibers connect the system of vestibular nuclei with the nuclei of the oculomotor and abducens nerves.
Adequate stimulation of the vestibular analyzer is the movement of endolymph in the semicircular canals. In this case, a whole complex of vestibular reactions arises (see), including vestibular H.
Vestibular nystagmus is divided into spontaneous, which is always a sign of a pathological process in any part of the reflex arc that carries out vestibular N., and artificially caused, or experimental, N., detected using a caloric test or rotation (see Vestibulometry). Artificially caused N. is usually present and normal; with pathology, its indicators change—duration and character; This type also includes pressor N., which occurs when air pressure in the external auditory canal increases.
Spontaneous vestibular nystagmus has the following characteristics: direction, amplitude, degree, binocularity and monocularity (dissociated N.), predominance in a certain direction, changing character, alternation of phases, rhythm.
The direction of spontaneous vestibular N. is judged by its fast phase. It can have different directions: horizontal, vertical, diagonal, rotatory, converging, mixed (horizontal-rotatory). Horizontal N. occurs most often and is observed when the middle parts of the rhomboid fossa are affected. Vertical N. is usually less pronounced, rarely isolated, and more often diagonal (horizontal and vertical). Vertical and diagonal N. occur when the upper parts of the rhomboid fossa are affected, and rotatory N. occurs when the lower parts are damaged. Converging N., in which the eyeballs move towards each other, is a symptom of damage to the midbrain.
Depending on the amplitude, Nystagmus is divided into small, medium and large. With small N., the movements of the eyeballs are barely noticeable and the amplitude of their vibrations is 1–2 mm; the amplitude of large-scale N. can reach 8–10 mm; in rare cases, the eyeballs move during N. across the entire palpebral fissure from the external commissure to the internal one and back. Large-scale N. is characteristic of brainstem lesions.
Spontaneous vestibular N., depending on the direction of gaze, in which it appears, is divided into three degrees. First degree nystagmus appears only when looking towards the fast phase of H.; II degree occurs with direct gaze; III degree occurs when looking towards the slow phase of the N. Spontaneous vestibular N. usually intensifies when looking towards the fast phase, and the appearance of spontaneous N. with a direct look and towards the slow phase indicates stronger irritation of the vestibular apparatus.
Usually both eyes are involved in nystagmus (binocular N.). Often, with brainstem lesions of the vestibular apparatus, the eyeballs do not participate equally in N.: one eye moves with a greater amplitude, and the other with a smaller one. In rare cases, only one eye takes part in N., while the other remains motionless (monocular N.). Monocular N. may be the result of damage to the posterior longitudinal fasciculus or the nuclei of the oculomotor and abducens nerves.
Often spontaneous nystagmus prevails in one direction. The prevalence of N. can be based on its degree, when N. appears at a smaller angle of eye abduction or even with direct gaze, as well as in amplitude and tonicity. More often, horizontal N. is prevalent, less often vertical. The prevalence of horizontal N. in any direction indicates uneven, asymmetrical damage to the labyrinths and roots of the VIII pair of cranial nerves. In case of acute loss of function of one of the labyrinths (purulent labyrinthitis, thrombosis of the labyrinthine artery, fissures of the temporal bone pyramid), spontaneous N. occurs, directed towards the healthy labyrinth, and disappears after 2-3 weeks.
Changing spontaneous N. is called positional or positional nystagmus, since it often changes or appears only in certain positions. Thus, when changing position, N. can change amplitude, degree, frequency (most often), direction, or occurs only in certain positions of the patient, or sharply changes its character without changing position (with tumors of the cerebellum and fourth ventricle).
Spontaneous vestibular K. consists of rhythmically alternating fast and slow phases. During the slow phase, the eyeballs slowly retract; when they reach a certain abduction amplitude, a fast N. phase occurs, during which the eyeballs return to their original position. The normal ratio between the fast and slow phases in duration is usually 1:3, 1:5. Depending on the nature of the alternation of phases, N. is divided into the following types. Pendulum-shaped, trembling, or undulating, N., in which the slow and fast phases are the same and eye movements resemble the movements of a pendulum, as a rule, is not associated with damage to the vestibular system, but is caused by decreased vision that arose in early childhood and impaired gaze fixation . In rare cases of severe primary brainstem lesions (pontine tumors, strokes, encephalitis), pendulum-shaped trembling N. of vestibular origin appears.
Clonic jerky nystagmus occurs in a compensated form of central vestibular syndrome, which occurs when the peripheral part of the vestibular analyzer is damaged.
Tonic N. is observed during strokes in the acute period, with moderate and severe traumatic brain injury, in the acute stage of brainstem encephalitis, during the period of decompensation of hypertensive syndrome due to brain tumors (see Hypertensive syndrome).
A sharply expressed unevenness of N. in amplitude, rhythm, and duration of alternation of phases is characteristic of severe stem lesions (strokes, stem tumors, and encephalitis). The loss of the fast phase of N., when the eyeballs “float” towards the slow phase during the caloric test and remain motionless, is a formidable symptom characteristic of patients in a comatose state. In an even deeper comatose state, the slow phase N also occurs.
Depending on the location, peripheral and central spontaneous vestibular II are distinguished. Peripheral spontaneous N. occurs when the labyrinth or root of the VIII pair of cranial nerves is damaged. In direction, this type of spontaneous N. is horizontal-rotatory, less often rotatory. Vertical, diagonal and converging N. do not occur with peripheral lesions. When one of the labyrinths dies, spontaneous N. is directed in the healthy direction, and when one of the labyrinths is irritated, it is directed towards the irritated labyrinth. N.'s character is rhythmic, with regular alternation of phases, binocular. It is often accompanied by an increase in vestibulo-vegetative and vestibulosensory reactions, as well as other vestibulosomatic reactions (spontaneous deviation of the arms and torso), while the deviation coincides in direction with the slow phase of spontaneous N. Peripheral N. disappears after 2-3 weeks. due to compensatory restructuring in the central sections of the vestibular analyzer.
Central spontaneous nystagmus, in contrast to peripheral nystagmus, is caused by damage to the vestibular nuclei and vestibuloculomotor connections in the posterior longitudinal fasciculus system. In direction, along with horizontal and rotatory, there are vertical, diagonal and converging N.; often N. becomes dysrhythmic, tonic, and monocular. The reaction of deviation of the arms and body does not always correspond to the slow phase of spontaneous N. (vestibular disharmony). With severe central N., patients often do not experience dizziness and vestibulo-vegetative reactions are not observed. Central N. can remain for a very long time, sometimes for life.
To judge the topic of spontaneous N., it is necessary to analyze the signs of spontaneous vestibular disorders, data from studies of experimental vestibular tests and hearing, and also take into account the wedge and picture of the disease. Vestibular symptoms, including vestibular N., are especially clearly manifested during the acute development of the pathological process, for example. with acute labyrinthitis (see), acute swelling of the labyrinth during an attack of Meniere's disease (see Meniere's disease), in the acute period of traumatic brain injury (see), stroke (see), subarachnoid hemorrhages, with rapidly increasing hypertension due to malignant tumors brain Most often, spontaneous N. occurs when the labyrinth and stem sections of the brain in the posterior cranial fossa (pons) are damaged. With tumors of the posterior cranial fossa, spontaneous N. occurs in 92% of cases, varies greatly in direction, degree, amplitude, and the nature of the alternation of phases depending on the location, size, direction of growth, the nature of the tumor and the age of the patients. The closer the tumor is located to the primary arc of the vestibular reflex (vestibular nuclei, vestibulo-oculomotor connections in the posterior longitudinal fasciculus at the bottom of the fourth ventricle), the more pronounced spontaneous H.
So, for example, with tumors of the pons, spontaneous N. occurs in 100% of cases, of the cerebellopontine angle - in 95%, of the fourth ventricle - in 92.7%, of the cerebellum - in 84.2% of cases. With tumors of the cerebral hemispheres, spontaneous N. occurs only in 11-12% and is much less pronounced than with tumors of the posterior cranial fossa.
Spontaneous Nystagmus often occurs with cracks in the pyramid of the temporal bone, in the acute period of any traumatic brain injury, with vascular disorders in the vertebrobasilar system, with brainstem encephalitis, arachnoiditis and arachnoencephalitis, localized mainly in the posterior cranial fossa, with multiple sclerosis.
Usually spontaneous N. is examined visually (nystagmoscopy) or recorded (nystagmography). The method of electronystagmography (see), which allows accurate recording of nystagmus, has become widespread.
N.'s study is carried out in the following sequence: with direct gaze; with extreme aversions of gaze; tilting the head to the sides and back; lying on your back and side. Often spontaneous N. changes especially sharply when the head is tilted to the sides and when the patient lies on his side (positional nystagmus).
To clarify the diagnosis, functional loads are applied to the vestibular apparatus, using calorization, rotation and galvanic current.
Artificially induced vestibular nystagmus is caloric, rotational, post-rotational and pressor; Galvanic N is studied much less frequently.
Caloric nystagmus refers to movements of the eyeballs that occur during artificial cooling or warming of the labyrinth. Heat or cold causes movement of the eidolymph in the semicircular canals (cold particles go down, hot particles go up), which is an adequate stimulus to the vestibular analyzer. There are several options for performing a caloric test; The most rational option is to inject 100 ml of water at t°25° into the external auditory canal for 10 seconds. If there is no reaction, pour in water at a temperature of 19°. If there is a clear asymmetry of the vestibular reflexes obtained from both labyrinths, pour in 100 ml of hot water (over 37°). Normally, caloric N. according to this method appears after 25-30 seconds. and lasts 50-70 seconds. Sometimes, normally, caloric N. is absent, but the reactive deviation of the hands towards the slow phase of N. with eyes closed after calorization always remains clear. The caloric test allows you to explore each maze separately. To irritate the horizontal semicircular canal, it is given a vertical position, for which the patient’s head is tilted 60° back. When the horizontal semicircular canal is irritated with cold water, a horizontal caloric N. appears, which is directed in the direction opposite to the ear being examined, and when hot water is infused (over 37°), a N. appears, directed towards the ear being examined. The change in caloric N. can be in duration (normal, increased, decreased, no reaction) and in qualitative characteristics, which have the same meaning as with spontaneous vestibular N.
In case of peripheral and nuclear damage to the vestibular analyzer during calorization with hot and cool water, the severity of N. depends on the labyrinth being studied: regardless of the direction of the caloric N., reactions from the labyrinth will be normal, increased or decreased. With subcortical lesions during hot and cold calorization, N. will be expressed more in one direction, often towards the lesion, regardless of which labyrinth is irritated. Distinct vestibular asymmetries of caloric N. of the peripheral-nuclear or subcortical type are usually found in the decompensated phase of diseases of c. n. With. and with damage to the peripheral part of the vestibular analyzer.
Rotational and post-rotational nystagmus occur during and after rotation. In this case, the right and left semicircular canals are always irritated simultaneously, however, according to Ewald’s law, the greatest irritation will be in that semicircular canal where the endolymph flow goes in the direction of the ampulla: this stronger irritation masks the irritation from the other labyrinth, where the endolymph flow comes from the ampulla .
Therefore, rotational Nystagmus is directed in the direction of rotation, and post-rotational Nystagmus is directed in the opposite direction. Rotation is a stronger and more short-term irritant than calorization. The rotational test is performed either in a Barany chair or on special electronically controlled vestibular stands, which make it possible to accurately dose angular positive and negative accelerations, rotation speeds and stop stimuli over a wide range, carry out rotation according to a variety of programs and objectively record vestibular reflexes.
In healthy people, as well as with unilateral loss of vestibular function, post-rotational N. is preserved during intense vestibular stimulation. Post-rotational N. falls out only in case of bilateral death of the labyrinths or roots of the vestibular nerves (bilateral total neuritis of the VIII pair of cranial nerves after meningitis, the use of ototoxic antibiotics), as well as in the decompensated phase of diencephalic-subcortical damage, but in the latter case the vestibular-vegetative, sensory and motor ones sharply increase reactions. Pressor N. can be caused directly by pressing a finger on the tragus. The appearance of pressor N. indicates the presence of a destructive process (fistula) in the bone wall of the labyrinth, most often the horizontal semicircular canal, due to chronic purulent inflammation of the middle ear (see Otitis).
Galvanic N. occurs under the influence of irritation of the labyrinth by direct electric current.
Optokinetic nystagmus is caused artificially by rotating a special drum under study in front of the eyes; like the vestibular one, it has a slow and fast phase, but its reflex path is different: visual stimulation from the retina goes through the visual pathways to the occipital lobe of the brain, where the optomotor path begins, which crosses in the upper parts of the brain stem at the level of the posterior cranial fossa and ends in the vestibular nuclei, and irritation through the system of vestibular-oculomotor connections goes to the oculomotor nuclei.
Violations of optokinetic N. are of great practical importance in the clinic. When the peripheral vestibular analyzer is damaged, optokinetic N. does not change; when lesions appear in the posterior cranial fossa, it is directed towards the lesion. Lesions in the cerebral hemispheres cause contralateral loss or weakening of horizontal optokinetic N. (when lesions are localized in the occipital and temporal regions, homonymous hemianopia appears on the side opposite to the lesion, and in the frontal region it proceeds without hemianopsia).
Other types of nystagmus.
Professional nystagmus of coal miners and miners, associated with impaired gaze fixation in low light, working in a half-bent position, has a tremulous pendulum-like character. Due to the improvement of working conditions in mines, this pathology is rare.
Congenital (hereditary) N. often accompanies other hereditary diseases of the nervous system; it is caused by insufficient development of the vestibular system.
Fixation and adjustment N. occur in healthy people with extreme gaze aversion. Fixation N. is longer, installation N. quickly disappears. These types of N. are caused by fatigue of the eye muscles with extreme abduction of gaze.
Voluntary Nystagmus is caused in rare cases by Ch. arr. in persons who have the ability to contract other muscles that do not normally obey voluntary activity (for example, movement of the ears).
Bibliography:
Ageeva-Maikova O.G. and Zhukovich A.V. Fundamentals of otorhinolaryngoneurologpi, M., 1960; Blagoveshchenskaya N. S. Clinical otoneurology for brain lesions, M., 1976; Differential diagnosis of otogenic and vascular vestibular disorders, Study of positional nystagmus, Guidelines, comp. G. M. Grigoriev, Chelyabinsk, 1976; Kalinovskaya I. Ya. Stem vestibular syndromes, M., 1973; Khechinashvili S.N. Vestibular function, Tbilisi, 1968, bibliogr.; Kekhaiov A. N. Differential diagnostic problems in otoneurology, Sofia, 1962, bibliogr.; Ktonas PY a. O. Effect of electronic filters on electro-nystagmographic recordings, Arch. Otolaring., v. 101, p. 413, 1975; Ryu JH a. McCabe BF Central vestibular compensation, ibid., v. 102, p. 71, 1976; Spector M. Electronystagmographic findings in central nervous system disease-Ann. Otol. (St Louis), v. 84, p. 374, 1975, Tantchev KS Particularites diffe; rentielles et diagnostiques du nystagmus de position peripherique et centrale, Rev. Laryng. (Bordeaux), t. 95, suppl., p. 449, 1974.
N. S. Blagoveshchenskaya.
Diagnosis of nystagmus
If nystagmus appears, consultation with an ophthalmologist, ENT doctor and neurologist is necessary. After an objective examination of the patient and determination of external manifestations of pathology, the following additional studies are prescribed:
- blood test to detect hypovitaminosis;
- X-ray, MRI or CT scan of the brain;
- electroneuromyography for diagnosing myasthenia gravis;
- electroencephalography to detect epilepsy or focal brain damage, such as a tumor.
Treatment of nystagmus
Due to the fact that it is not possible to completely cure the disease, treatment is aimed at reducing the progression of the disease and improving visual functions. The treatment regimen is based on therapy of the underlying disease that provoked the appearance of nystagmus. To improve visual functions, vision correction is performed. Contact lenses and glasses are used for myopia and farsightedness. Correcting astigmatism has a very significant effect on inhibiting further progression of the pathological process.
Vitamin therapy, drugs that support the immune system and vasodilators are used. For special indications, surgery is performed to correct the oculomotor system to reduce eye fluctuations.
Conditions resembling nystagmus
Nystagmus may resemble eye movement disorders such as:
- convulsive twitching of the eyeballs with a characteristic rectangular signal (small jerky movements away from the point of fixation and back)
- trembling of the eyeballs (horizontal pulsating vibrations)
- opsoclonus (frequent saccadic oscillations)
- myokymia of the superior oblique muscle (monocular rotatory-vertical movements)
- ocular bobbing (ocular bobbing - rapid deviation of the eyeballs down with a slow return to the top)
- periodic movements of the eyeballs in a horizontal direction with a change in the direction of deviation every few seconds
Visual disturbances and movements of the eyeballs are a signal of danger, the recognition of which greatly increases the knowledge of a neurologist and neurosurgeon. A neurologist or neurosurgeon who is alert to such visible signals that the eye can send will not only recognize and differentiate them from each other, but will also understand their clinical significance.
Symptoms of the disease
Ocular nystagmus develops when there is a certain eye disease; its symptoms are similar to those of the underlying disease. The patient experiences sensitivity to light, frequent dizziness, and poor vision. Often patients complain of a blurry image before their eyes, or its fluctuation and trembling.
During examination, the ophthalmologist notes a significant fluctuation of the eyeball, which can have a variety of directions. Eye movement can occur either spontaneously or due to certain provoking factors.
Depending on the direction there are:
- Horizontal view;
- Vertical.
The right eye moves to the right side faster than to the left, this phenomenon is jerky. Sometimes there is a mixed type, in which when a person looks straight ahead there is a pendulum movement, and in one direction there is a jerky movement.
Symptoms in children are divided into several types.
After the first month of life, the child’s gaze must focus. If this does not happen, then suspicion falls on the existence of nystagmus in the eye. Sometimes, this phenomenon is congenital in nature, and is formed during intrauterine development. This deviation has the following features:
- Formed in the second month and occurs throughout life;
- Pathology is absent when the eyes are closed;
- The nature of the direction is horizontal and jerky.
In some directions the symptom does not manifest itself in any way.
Spasm of a sternocleidomatous nature. It appears between the ages of three months and one year. If the cause cannot be determined, then sometimes it completely goes away by the age of three. Sometimes the reason lies in the development of a pathological tumor. Low-amplitude nystagmus is sometimes accompanied by head nodding.
Latent nystagmus. Occurs in the presence of strabismus not accompanied by various types of paresis. A characteristic of this condition is that nystagmus does not appear when the eyes are open, and occurs only when the lighting deteriorates. This disease can occur in people with albinism, a condition where there is no pigment in the iris.