Classification of nystagmus
Nystagmus has several classifications. They differ in the characteristics of vibrations and the reasons for their occurrence. If we talk about the types of oscillations, then the following types of nystagmus are distinguished:
- Horizontal, in which the eyes move from left to right and vice versa.
- Vertical. Oscillatory movements occur from top to bottom or bottom to top.
- Diagonal. Eye movement is directed in accordance with the diagonals.
- Rotatory, in which the eyes rotate.
Classification
According to the IBC 10 classification, this disease is coded H55. The pathology is beyond human control; it is necessary to undergo a set of procedures to correct the situation.
The following forms of horizontal nystagmus are distinguished:
- A spontaneous form of pathology is possible with direct gaze or when turning the gaze. Its direction is assessed by the fast component, forcing you to fix your gaze on the doctor’s index finger.
- Pendulum tremor involves rhythmic harmonious vibrations.
- Jerky tremor is most often acquired. Spherical formations in the orbit move in different directions at different rates. The jerky form indicates a dysfunction of the central or peripheral part of the vestibular analyzer.
- The tonic form of the disease indicates serious damage to the vestibular sensory system. It develops when the brain is damaged. Indicates intracranial hemorrhage, stroke, hypertension.
- The congenital form of the pathology involves the discovery of the disease shortly after the birth of the child. Eye movement is impaired, and bilateral horizontal nystagmus is observed.
- A small-scale type of pathology is when the amplitude of movements is small and equal to no more than 2.5 mm. The cause of the disease is diseases of the labyrinth of the inner ear.
- The horizontal rotatory type of the disease is characterized by horizontal rotation of the eyeballs. He is accompanied by dizziness and loss of consciousness.
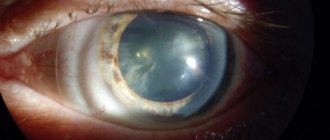
- Infantile. Most often develops at the age of 2–3 months. The eyes tend to move horizontally. It is often associated with other conditions such as albinism, congenital absence of the iris (the colored part of the eye), underdeveloped optic nerves, and congenital cataracts.
- Acquired. Develops later in childhood or adulthood. The cause of this condition often remains unclear. The acquired form can develop due to impaired functioning of the central nervous system, metabolic disorders, or the toxicity of alcohol and certain drugs.
Nystagmus in children
In children, suspicion of nystagmus arises when, by the beginning of the 2nd month of life, they cannot fix their eyes in one position. In this case, the disease is accompanied by the following symptoms:
- When a child sleeps, the eyeballs cannot be seen moving.
- Horizontal or jerky oscillations of the eyes appear.
- If the child directs his eyes in a certain direction, the vibration stops.
- There may be a decrease in visual acuity.
If a child has albinism, then there is no coloring pigment in his eyes. Nystagmus, which manifests itself with such a deviation, is defined as a separate group.
Nystagmus code according to ICD
ICD-10 Category: H55
ICD-10 / H00-H59 CLASS VII Diseases of the eye and its adnexa / H55-H59 Other diseases of the eye and its adnexa
Definition and general information[edit]
Nystagmus is rapid, repetitive, involuntary, oppositely directed, rhythmic movements of the eyeballs. There are two types of nystagmus: jerky (clonic) nystagmus, in which slow movements of the eyeball (slow phase) alternate with oppositely directed fast movements (fast phase). The direction of such nystagmus is determined by the direction of its fast phase. Pendulum-like (swinging) nystagmus is a rarer form in which the eyeballs perform pendulum-like movements of equal amplitude and speed in relation to the average position (although when looking away to the side, two different phases can be observed, the faster of which is directed towards the gaze).
Nystagmus can be either a normal phenomenon (for example, with extreme abduction of gaze) or a sign of damage to the brain stem, cerebellum, peripheral or central part of the vestibular system. In each of these cases, nystagmus has its own characteristic features.
The easiest way to observe nystagmus is during a smooth pursuit test, in which the patient follows the movement of the examiner's finger or hammer.
Etiology and pathogenesis[edit]
Normally, the eyeballs should follow an object, moving smoothly and consistently. Mild clonic nystagmus (several low-amplitude rhythmic movements), which appears with extreme abduction of the eyeballs, is physiological; it disappears when the eyes move a little closer to the midline and does not indicate pathology. The most common cause of large-scale clonic nystagmus with extreme abduction of the eyeballs is the use of sedatives or anticonvulsants. Optokinetic clonic nystagmus is a variant of physiological reflex nystagmus, which occurs when tracking similar objects moving past (for example, trees flashing in a train window, fence slats, etc.). It is characterized by slow tracking movements of the eyeballs, which are involuntarily interrupted by fast saccades directed in the opposite direction. In other words, the eyes fixate on a moving object and slowly follow it, and after it disappears from the field of view, they quickly return to the central position and fixate on a new object that comes into the field of view, beginning to pursue it, etc. Thus, the direction of optokinetic nystagmus is opposite to the direction of movement of objects.
Clinical manifestations[edit]
Pathological nystagmus occurs when the function of complex mechanisms that ensure gaze fixation is disrupted. The forms of pathological nystagmus are numerous and varied; so, L.F. Del Osso (LF Dell Osso, 1983) identified 41 variants of nystagmus. Pathological nystagmus can be optical, but in most cases it is vestibular.
Optical nystagmus
- caused by impaired gaze fixation due to low vision, manifested from birth or early childhood.
It is possible, in particular, with a high degree of myopia (6 or more diopters) and with various diseases leading to a decrease in visual acuity. In cases of decreased visual acuity in only one eye, optical nystagmus can be monoocular.
Congenital nystagmus
It manifests itself from the moment of birth, it is constant, large-scale, it also appears when the gaze is directed forward, and when the gaze is turned to the sides, its amplitude usually increases. Congenital nystagmus is often horizontal, pendulum-shaped, but can also be jerk-like. Despite the severity of oscillopsia, the patient does not experience a sensation of vibration of the visible space with congenital nystagmus.
Often congenital nystagmus is caused by low vision and in such cases it is called congenital optical nystagmus. It is usually horizontal, often pendulum-shaped (swinging), and manifests itself, in particular, in albino patients. However, congenital nystagmus can also occur with relatively preserved visual acuity. Its pathogenesis and localization of the lesion often remain unspecified. There is an opinion (Kamyanov I.M., 1989, etc.) that in such cases, nystagmus may indicate congenital minimal cerebral dysfunction, then it is often combined with stuttering, psychopathy, bedwetting and other neurological disorders. Congenital nystagmus can be hereditary. Hereditary forms of congenital nystagmus are most often transmitted by a recessive, X-linked type, and less often by an autosomal dominant type.
A rare form of congenital nystagmus, inherited in an autosomal recessive manner, is nystagmus-myoclonus, or Lenoble-Aubino syndrome
. It manifests itself as periodic twitching of the eyes, more often due to hypothermia or under the influence of irritating factors, sometimes spontaneously, and may be accompanied by diffuse hyperkinesis of the myoclonus type. This form of nystagmus was described by the French doctors Lenoble and Aubineau.
It must be borne in mind that if a patient with nystagmus follows a moving object, then in the case of congenital nystagmus the amplitude of its oscillations decreases over time, and in acquired nystagmus it increases. This clinical phenomenon, which helps differentiate congenital and acquired nystagmus, is known as the Louis-Bar symptom (described by the French doctor D. Louis-Bar).
Nystagmus acquired in early childhood
, like congenital nystagmus, usually pendulum-shaped. It may be due to progressive bilateral vision loss, in particular arising in connection with intracranial pathology. It is difficult to distinguish from congenital nystagmus, but should not be considered congenital unless confirmed by medical documentation. In rare cases, nystagmus may appear in a child after loss of vision in one eye.
Acquired pathological nystagmus
, manifested in adults, is often jerk-like, but can also be pendulum-like. Pendulum-like acquired nystagmus is usually central and reflects dysfunction of the brainstem and/or cerebellum. It may be a consequence of the manifestation, in particular, of vascular and demyelinating brain lesions. Acquired pendulum-like nystagmus is often horizontal, but can also be multivector, sometimes accompanied by head trembling. The severity of nystagmus may not correspond to the degree of decrease in visual acuity.
Spontaneous jerky vestibular nystagmus
biphasic, it is characterized by alternating an active slow phase and a corrective fast phase. As noted above, the direction of jerky nystagmus is determined by its fast phase.
Jerky nystagmus
can be tonic or clonic. Tonic nystagmus is characterized by a slow phase extended over time (the ratio of fast and slow phases is 1:10-1:30), while the nystagmus is slowed down, but its rhythm remains. Tonic nystagmus is a sign of a patient’s serious condition; it usually occurs with brain damage and often indicates an acute pathological process - impaired circulation in the brainstem, severe traumatic brain injury, stage of decompensation of intracranial hypertension, etc.
Clonic
jerky spontaneous or experimental nystagmus is recognized. It may be peripheral or central.
Peripheral nystagmus
occurs when the peripheral structures of the vestibular system are damaged and can only be horizontal or horizontal rotatory. It occurs with pathology of the labyrinths or vestibular nerves (vestibular portion of the VIII cranial nerve). Therefore, peripheral nystagmus can be a manifestation of labyrinthitis, Meniere’s disease, perilymphatic fistula, labyrinth trauma (usually due to a fracture of the temporal bone), labyrinthine apoplexy, toxic damage to the labyrinth (streptomycin, etc.), acoustic neuroma, pressure on the proximal part of the VIII cranial root nerve of adjacent vessels, etc. When the labyrinth receptors are irritated, the nystagmus is directed in its direction, and when the labyrinth is destroyed - in the opposite direction. With peripheral nystagmus, provoked during the caloric test, a shortened latent period lasting 3-10 s is common, its duration is approximately 10 s, and its attenuation is pronounced, nausea and vomiting are possible.
Diagnosis of nystagmus
Visual examination allows you to immediately identify nystagmus. To determine its cause, the following studies are carried out:
- Determining the degree of visual acuity.
- Determination of the condition of parts of the visual organs - fundus, retina, motor system, optic nerve.
- Electroretinogram.
- Determination of characteristics of optical media.
After receiving the results of the study, the patient is referred to a neurologist. He is prescribed an MRI of the brain or an electroencephalogram. Sometimes a patient with nystagmus is sent to an otolaryngologist.
Causes of nystagmus
The causes of occurrence are local . Nystagmus of the eyeball is congenital or developed as a result of visual impairments such as: albinism, strabismus, farsightedness , myopia, retinal dystrophy, optic nerve atrophy .
Also, the reasons may be general , eye tremors appear:
- As a result of damage to the pons, bulbus, cerebellum, pituitary gland or labyrinth. For example, after experiencing a stroke , inflammation of the inner ear , cranial wounds, oncology .
- In case of poisoning with medications (anti-epileptic, anti-malarial, sleeping pills, as well as gold drugs, salicylates and neuroleptics ) and narcotic substances.
Treatment of nystagmus
First of all, the doctor tries to eliminate the disease that led to disorders of the oculomotor system. Subsequent treatment is aimed at combating ophthalmological defects. To cure nystagmus, the following methods are used:
- Optical correction. To improve vision, the patient is given glasses or contact lenses. In the case of albinism, the patient is prescribed to wear glasses with light filters, which perform both a corrective and a protective function.
- Pleoptic treatment. Used to normalize visual functions and stabilize the refraction of light rays by the eye. This method involves stimulating the retina and performing various exercises. For stimulation purposes, illumination on a monobinoscope using a red filter and color or contrast tests are used.
- Conservative treatment. The purpose of medicines in this case is to improve metabolic processes and blood circulation, nourish the eye tissue with vitamins and minerals.
- Surgical intervention. Used in cases of pronounced oscillatory movements of the eye. In this case, the surgeon weakens some muscles and strengthens others. As a result, vision improves and the vibration frequency decreases. Internet users describe the operation this way:
Prevention of nystagmus
Nystagmus is very difficult to cure. Therefore, it is worth paying special attention to preventing its occurrence. There are only two basic rules for reducing the risk of disease. The expectant mother should already take care of his health while carrying a child, protecting her body from any negative influences. Avoiding self-medication will help prevent the appearance of acquired nystagmus. This means using only those medications that were prescribed by a doctor. In addition, it is necessary to balance the diet so that it includes a sufficient amount of dairy and plant products.
Nystagmus:
- NOS
- congenital
- as a result of visual deprivation
- disunited
- latent
Excluded:
- mechanical complication from:
- intraocular lens (T85.2)
- other ocular prosthetic devices, implant and graft (T85.3)
ICD-10 text search
Search by ICD-10 code
Search by alphabet
ICD-10 classes
- I Certain infectious and parasitic diseases (A00-B99)
In Russia, the International Classification of Diseases
10th revision (
ICD-10
) was adopted as a single normative document for recording morbidity, reasons for the population’s visits to medical institutions of all departments, and causes of death.
ICD-10
introduced into healthcare practice throughout the Russian Federation in 1999 by order of the Russian Ministry of Health dated May 27, 1997. No. 170
The release of a new revision (ICD-11) is planned by WHO in 2020, 2018, 2022.