Red and even just reddish or pink urine can appear for various reasons. It can be colored by foods consumed the day before and medications taken. But most often, reddish urine in men is a symptom of a certain disease, which often poses a serious threat to health. In this situation, we are no longer talking about random urine pigmentation, but hematuria - the penetration of red blood cells into the urine, which should not normally happen.
Pathological causes of urine pigmentation
In a normal physiological state, the kidneys extract urine that has a yellow tint. Why does my urine turn red? Among the possible causes, the most likely development of the following pathologies:
- Tumors of malignant and benign etiology. It compresses adjacent vessels of the genitourinary system (GUS) and causes them to overstrain. The result is an increase in the permeability of the vessel walls or their complete rupture. This is followed by the penetration of red blood cells (erythrocytes) into the urine and the coloring of urine pink, reddish or dark red, depending on the severity of vascular damage.
- Congenital cystic malformations of the MPS, similar to tumors in their dysfunctional effect.
- Stones in the kidneys, bladder and ureters, which mechanically injure the urinary tract and cause bleeding. Injuries caused to this area from outside the body can lead to the same consequences.
- Infectious lesions of the genitourinary organs, leading to bacterial destruction of their tissue and vascular structure.
- Anemia, leukemia, insufficient blood clotting, prostatitis and nephritis also cause red blood cells to enter the urine and color it various shades of red.
Hemospermia: causes, diagnostic search
30.04.2018
11447
4
The topic of hemospermia is not often discussed at professional meetings of urologists, however, every urologist encounters patients with this symptom. Anton Yuryevich Tsukanov, urologist, Doctor of Medical Sciences, Professor of the Department of Surgical Diseases and Urology of the Omsk State Medical Academy of the Ministry of Health of Russia, made a report on the possible causes, as well as methods of diagnosing and treating hemospermia at the Moscow meeting of the ASPECT DOK.
| A.Yu. Tsukanov Doctor of Medical Sciences, urologist, professor of the Department of Surgical Diseases and Urology of the Omsk State Medical Academy of the Ministry of Health of Russia |
The problem has been known to doctors since ancient times, its first descriptions belong to Hippocrates and Galen, and later ones - A. Pare and G. B. Morgagni. In the textbook of urology edited by N. A. Lopatkin, well known to Russian specialists, it is noted that hemospermia (haemospermia) - the appearance of blood in the ejaculate - can be either true or false. With true (haemospermia vera), the blood uniformly stains the sperm a rusty, dark red color and the sources are the testicle or prostate. With false hemospermia (haemospermia spuria), blood is mixed with sperm in the form of separate filamentous clots, and the source is the urethra.
Statistical data
Statistically, hematospermia accounts for about 1% of all urological symptoms. It may occur in a single episode or in multiple episodes. Patients, however, usually consult a doctor after the first one, for fear of malignancy or sexually transmitted diseases (Dean E.). The problem occurs in men of all ages, the average age is 37 years (Ng Y. H et al., 2013), the presence of hemospermia lasts, usually 1–24 months (Mulhall JP, Albertsen PC, 1995; Amano T. et al., 1994). When screening 26,126 people over 50 years of age for prostate cancer, hemospermia was found in 0.5% of cases (Han M. et al., 2004). According to the results of another study, the probability of any malignancy against the background of hemospermia is about 3.5% (Ahmad I., Krishna NS, 2007). It is worth considering, however, that the exact percentage of cases of hemospermia is unknown, since it is often impossible to examine the ejaculate during coitus during unprotected intercourse.
Causes of hemospermia
A systematic review undertaken more than 10 years ago (Kumar P., Kapoor S., Nargund V., 2006) identified a number of common causes of hemospermia. Thus, a category of congenital causes has been identified, which include cysts of the seminal vesicles and ejaculatory tract. Inflammatory causes include urethritis, prostatitis, epididymitis, vesiculitis, urethral condylomas, tuberculosis, schistosomiasis and viral lesions. Also, the reason may lie in obstruction - this includes post-inflammatory changes, calculi, diverticula and seminal vesicle cysts, as well as urethral strictures. It is necessary to consider a number of possible cases of malignant diseases: neoplasms of the prostate, bladder, seminal vesicles and scrotal organs. Vascular factors are represented by varicose veins, hemangiomas and sexual excesses. Traumatic - direct injury, as well as consequences of minimally invasive treatment of hemorrhoids and iatrogenicity (for example, after a prostate biopsy). Finally, systemic factors may also be present: hypertension, pathology of hemostasis, and the use of certain medications.
At the same time, in men under 40 years of age, the prevalence of inflammatory factors is in first place - 15%, stones and calcifications cause hemospermia in 1.4% of cases, malignancy (primarily testicular cancer) - also in 1.4%. In the age group over 40 years old, however, the picture changes. Inflammatory factors lead to the appearance of symptoms in 10.3% of cases, stones and calcifications in 2.2%, and malignant neoplasms (mainly prostate cancer and urethral carcinoma) in 6.2%.
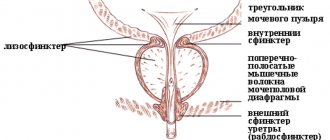
A. Yu. Tsukanov also presented a table of the percentage of the contribution of ejaculatory structures to the formation of seminal fluid. For example, the testicles and epididymis contribute 1–3%, the Kupffer glands — 5–10%, the paraurethral glands — 0.5–1%, the prostate — 20–25%, and the seminal vesicles — 60–80%. Accordingly, the percentage of probability of damage to the relevant organs during hemospermia will be the same.
As A. Yu. Tsukanov emphasized, speaking about such a frightening symptom for patients as hemospermia, it is necessary to name a number of possible rare causes. For example, one of the studies available today (Amasanti M. et al.) considers hemospermia as a manifestation of severe hypertension in youth. The authors described a case of hemospermia in a 28-year-old patient associated with severe hypertension, after correction of which with ramipril the hemospermia disappeared. The man had 4 episodes of hemospermia over 10 days; no abnormalities were detected in the examined organs and systems; the only symptom present was high blood pressure (228/135) of unknown etiology.
Another rare case is hemospermia as a consequence of Zinner syndrome. A 2021 paper (Canales-Casco N. et al.) describes a clinical case of a 17-year-old patient with a complaint of hemospermia after the onset of sexual activity. The results of the microbiological examination of the young man were negative, PSA level was 0.5 ng/ml, ultrasound revealed the presence of a cyst in the left caudal bladder and the absence of the left kidney, MRI showed a giant cyst of the left seminal vesicle with left-sided renal aplasia. As a result, the patient was diagnosed with Zinner syndrome. This pathology, described in 1914, is characterized by unilateral cystic dilatation of the seminal vesicle, unilateral renal aplasia and obstruction of the ejaculatory duct. It is more often found in men aged 30–50 years. Typically asymptomatic, but may manifest as mild perineal pain, dysuria, or infertility. The syndrome develops as a result of pathology of the duct of the primary kidney (mesonephros).
Diagnosis and search for the cause
In the process of diagnosing a patient with a complaint of hemospermia, it is necessary to pay attention to the accompanying symptoms: the presence of pain, general oncological symptoms and symptoms of the lower urinary tract. It is also important to assess the likelihood of having an STI, consider the epidemiological and sexual history, pay attention to blood pressure and the state of the blood coagulation system (Leocadio DE, Steia BS, 2009).
When collecting anamnesis, it is recommended to pay attention to the timing, frequency and duration of hemospermia and the color of the sperm: bright red with or without clots (fresh bleeding) or brown (old blood). Symptoms indicating infection are also taken into account: dysuria, frequency or severity of urination, visible hematuria, pain in the abdomen, scrotum, pelvis and perineum.
In addition, factors such as recent urological studies or interventions should be considered; a history of prolonged or excessive bleeding or easy bruising from minor trauma or surgery; bleeding bleeding disorders; travel to regions where tuberculosis and schistosomiasis are endemic; family history: prostate cancer, especially in the first degree and in relatives diagnosed before 60 years of age, as well as coagulopathy.
During the physical examination, it is recommended to examine the external genitalia, palpate the scrotum for swelling, elasticity, tuberosity of the testicles and epididymis, and perform a digital rectal examination to evaluate the prostate for enlargement, elasticity, mobility, and the presence of nodules. It is also recommended to look for signs of mild bruising or bleeding, such as large bruises (greater than 5 cm in diameter) in the absence of trauma or petechiae. It is important to examine the peritoneal cavity for the presence of hepatosplenomegaly, which may indicate underlying hematologic, hepatic, or infectious diseases. Blood pressure should also be measured to detect hypertension.
Next, the speaker cited the results of a Japanese study (Furuya S. et al.), conducted with the participation of 189 men with hemospermia. Of these, two were diagnosed with prostate cancer, one with bladder cancer, three with chronic bacterial prostatitis, two with urethrocystitis, and two with distal urethral hemangioma.
Of the remaining patients, 168 (88.9%) had hemospermia that resolved spontaneously. The average duration of the disease was 1.5 months (1–42 months). Moreover, of those 21 (11.1%) in whom this did not happen, in 15 hemospermia persisted during observation. The average duration of the disease here was 22 months (3–48 months). In 6 people, the cause of the symptom remained unclear, two of them died, and four refused follow-up. The mean follow-up period was 52 months (range 2–167 months).
It is important to understand that persistent and recurrent hemospermia predetermines urological examination, since there is a proven connection with prostate cancer. Thus, according to one of the available studies, out of 900 episodes of the disease, prostate cancer is detected in 3.5% of cases (Ahmad I, Krishna NS, 2007). However, other work indicates 5.7% based on a review of responses to 300 cases (Leary FJ, Aguilo JJ, 1974).
Among the available research methods, TRUS provides clear visualization of the prostate, seminal vesicles and adjacent structures. Many studies have proven the advantage of this method in correct diagnosis (detection of stones, calcifications, cysts, remnants of the Müllerian duct, prostate varicose veins and inflammatory changes).
As for MRI, one of the British studies was devoted to it (Luke A. et al). It analyzed data from patients who visited the clinic's outpatient department over a two-year period. The authors compared the rate of prostate biopsy and the rate of cancer detection in patients who did and did not undergo MRI due to hemospermia.
A total of 47 patients were considered and also underwent TRUS and PSA testing. Of these, 19 MRI was not performed; in this group, four men had a prostate biopsy, and one adenocarcinoma was detected. In 24, MRI was performed, in this group there were 17 biopsies and 3 adenocarcinomas were detected. Thus, in the MRI group, 71% of patients underwent biopsy, and in the non-MRI group, 21% underwent biopsy. The rate of detection of prostate cancer in the group with MRI was 18%, and without it - 25%. As a result, the authors concluded that careful use of MRI is necessary, which expands the indications for biopsy without increasing the detection rate of prostate cancer.
Algorithm for examining patients with hemospermia
The standard algorithm for examining patients with hemospermia begins with a history and physical examination, including blood pressure measurement. This is followed by a blood test and coagulogram; urological analysis, including bacterial culture and microscopy; as well as culture and microscopy of ejaculate. In the future, you should proceed from the situation. Patients over forty years of age with a single episode and at any age with recurrent episodes are referred for additional urological studies (TRUS, PSA level test, biopsy). In a single case of hemospermia in men under 40 years of age, systemic causes and secondary pathologies, as well as infections, can be considered, for which antibacterial therapy is prescribed according to indications. Idiopathic hemospermia is also possible, in which the patient must be reassured and advised to return in case of relapse.
As Anton Yurievich emphasized, it is necessary to explain to the patient that hemospermia is not always associated with a specific disease. Moreover, the probability of its spontaneous resolution after 1 month is 57.7%, after 3 months – 34.2%, after 6 months – 23.3%, and after 12 months – 12.5%. The cure period may be longer if the seminal vesicles are dilated, there is a median prostate cyst, or there is obstruction of the seminal tubercle.
As part of the treatment, prostate or seminal vesicle cysts are aspirated under TRUS guidance. For repeated episodes of hemospermia, fibrourethrocystoscopy (dilated veins of the prostate and urethral abnormalities) is performed. The method of treating obstruction of the vas deferens in the area of the seminal tubercle is endoscopic opening of the site of stenosis.
The article was published in the journal “Urology Digest” No. 2/2018, pp. 10-15
Comments
Gaponenko Anatoly Dmitrievich - 05/07/2018 - 12:54:47
Very interesting article, thank you very much!
Yusupov Rustam Makhmudovich - 05/02/2018 - 15:25:17
Well, at least tuberculosis is mentioned in one line... From personal experience, there was a case when a person over 50 years of age who complained of a macroscopic admixture of blood in the ejaculate had a partner slightly older than 20. And in order to look macho in her eyes, his excesses manifested themselves 3-4 times a day. It was enough for him to recommend moderating the frequency of sex and hemospermia was gone...
Toshtemirov Umidjon Boymuratovich - 05/02/2018 - 10:43:24
Thanks a lot!)
Oreshkov Vasily Sergeevich - 05/02/2018 - 10:26:19
thank you very much for the article.
To post comments you must log in or register
Color change in the absence of pathologies
Red urine can appear in men for completely harmless reasons. Let's look at the most common of them.
Beet
Eating beets, especially in large quantities, inevitably leads to the excretion of some of the pigment through the excretory system, including urine. It is then painted in the appropriate color.
To verify this, it is enough to perform a simple chemical procedure yourself. You need to pour some of the urine into a small sterile vessel, add a little baking soda there, shake the liquid and pour in 9% vinegar with a spoon. The urine should eventually turn white and then turn red again. If this does not happen, then there is a possibility of another cause of redness. This may already be a reason to visit a doctor.
Another differentiating sign of nutritional pigmentation is the absence of pain when urinating.
Alcohol
Urine becomes reddish after taking large doses of alcohol, most often during a binge. In addition to typical somatic disorders associated with orientation in space, ethyl alcohol affects the kidneys: due to its hydrophilic properties, it draws fluid from the tissues into the walls of blood vessels, causing them to swell and narrow the internal lumens.
The result is an increase in pressure in the circulatory system, in particular in the renal glomeruli. It is from there that red blood cells, constrained by the compressed space of the bloodstream, infiltrate into the urine.
Usually this phenomenon is short-lived. A few days after drinking alcohol, everything goes away without a trace. With chronic heavy drinking, the picture gradually changes. Changes in the kidneys take on an organic nature, and it is no longer possible to do without medical intervention.
Sports activities
The mechanism of urine color change after prolonged exercise is explained by dehydration of the body and is similar to alcohol intoxication. The consequences are also temporary.
The shades of urine are directly affected by:
- Duration of physical effort and its intensity;
- Individual adaptability of the organism;
- Subjective factors of perception (sometimes the fear of slight pinkness in urine inclines one to emotional exaggeration).
In addition, in men who play sports, untreated inflammatory diseases can cause red urine.
Medicines and certain food products
Among the pharmacological agents, urine can be colored in various shades from pink to dark brown: phenolphthalein, quinine, potassium permanganate, rifampicin, metronidazole.
Foods that can pigment urine include colored lemonades, coffee and tea, blackberries, rhubarb, blueberries, and paprika.
Nature of the phenomenon
The normal color of adult urine is clear or deep yellow. The color of urine is influenced by a substance called urochrome. It is a product of the breakdown of hemoglobin that occurs in red blood cells. What factors can influence the color of urine? Firstly, this is the person's age. Many people have probably noticed that children's urine has a lighter shade. The amount of fluid consumed is also of great importance. People who drink a lot of water have almost clear urine. If there are disturbances in the body's water balance, the urine may take on an amber hue.
As a rule, a change in the color of urine attracts a person's attention. Why is urine red in men? Sometimes such manifestations can occur when changing your diet or taking potent medications. In any case, if you notice a reddish tint to the urine or the appearance of blood clots in the discharge, this is a serious reason to consult a doctor.
Diagnosis of MPS
The main objective of this event is to determine the cause of redness of male urine for pathology and anatomical localization of the source of bleeding. Non-pathological factors mentioned above should be excluded at the very beginning. To do this, before conducting basic tests, the patient is strongly advised to refrain from taking relevant foods and medications.
The simplest diagnostic methods include taking anamnesis—finding out the patient’s medical history from the moment its first symptoms appeared. This is followed by an external examination of the patient to identify any anatomical abnormalities, palpation of the problem area to identify pain.
More objective data is provided by urine and blood analysis, as well as ultrasound examination (ultrasound), which allows the diagnostician to trace changes in the location and anatomical shape of the kidneys, bladder, ureters and genital organs.
If there is ongoing bleeding, you can determine its intensity yourself using three glasses containing portions of urine from three consecutive urinations. Unchanging, stable color indicates severe bleeding. If the color gradually fades, the process is weaker. But, one way or another, a visit to the urologist is necessary.
To determine the location of the source of bleeding, they rely on external signs proven by experience:
- Blood stains on underwear and red urine in the absence of pain in the lower abdomen suggest the presence of a tumor;
- Brown urine indicates some kind of renal pathology;
- Scarlet urine - about damage to the lower part of the ureters;
- Red feces accompanied by severe pain indicate that the most likely cause may be stones in the kidneys or urinary system (possibly infection);
- Constantly changing shades of urine, a frequent desire to empty the bladder, temperature, and chills suggest a diagnosis of prostate inflammation.
Diseases that cause hematuria
These include:
- Glomerulonephritis. An inflammatory process that occurs after a recent illness (angina, lupus erythematosus, rheumatoid arthritis). The renal vessels become fragile, blood leaks into the urine. Signs of this disease include difficulty urinating, increased body temperature, weakness in the body, and pain in the lumbar girdle.
- Porphyria. A genetic type of pathology that causes disturbances in hemoglobin synthesis. The kidneys begin to produce porphyrin, which turns the urine red. The main signs of this problem include loss of body weight, anemia, fear of light, and brown color of the enamel coating of the teeth.
- Urolithiasis. Occurs due to the appearance of stones in the kidneys. Moving along the ureteric passage, the pebble causes injury to its walls, damaging blood vessels and capillaries. The main symptom of the disease is severe and sharp pain when visiting the toilet, increased frequency of the urge to urinate, and impaired urine outflow. Body temperature may rise, weakness appears in the body, and sand is excreted along with urine.
- Prostatitis. One of the most common diseases of the urinary and reproductive systems in men. It occurs in acute or chronic forms, manifested by fever, chills, increased urge to urinate, pain in the lower back, groin or perineum.
- BPH. It is a benign neoplasm that appears in men over fifty years of age. The patient begins to suffer from sexual dysfunction, pain when secreting biological fluid, frequent trips to the toilet, and a feeling of incomplete emptying of the bladder.
- Prostate oncology. Often found in men, it occurs due to untreated inflammatory processes. The disease passes without pronounced symptoms. When the condition is neglected, rapid weight loss, weakness in the body, swelling of the legs, and lower back pain are observed.
- Urethritis, cystitis. They may occur due to dangerous microorganisms entering the body. They cause general weakness, fever, increased urine output, accompanied by burning sensations, the appearance of blood in the urine, purulent accumulations and mucus, and pain in the groin.
- Tuberculosis of the genitourinary system. The disease affects the prostate. The cause of its appearance is considered to be tuberculosis pathogens that penetrate human organs through blood cells or a paired organ. The patient begins to feel severe pain in the groin, fever, and pain during urination.
We advise you to study - Male frigidity - what it is, symptoms and treatment
How to get rid of hematuria
Red urine in men is an urgent indication to consult a urologist. After a thorough examination of all parts of the genitourinary system and identification of the immediate focus responsible for vascular bleeding, conservative therapy is prescribed. It facilitates the removal of sand or stones from the MPS.
If the latter cannot be achieved with therapeutic methods, surgery is prescribed. The same is done in the presence of operable tumors.
The methods and timing of treatment for hematuria depend on the reasons that caused it. If this is playing sports or using contraindicated medications, then to return to normal it is enough to simply ease the rhythm of training and eliminate drugs that cause allergies.
Inflammations of an infectious nature, causing the appearance of blood in the urine, are effectively relieved by antibiotics. Traumatic injuries are treated comprehensively: physiotherapy and massage are added to the medication. The results of treatment largely depend on the severity of the injury.
The greatest difficulty is the treatment of urolithiasis, glomerulonephritis, prostatitis and prostate adenoma - pathologies that are the most common source of blood in urine. In this case, you need to tune in to long-term therapy. Its effectiveness is higher the sooner the patient contacts a urologist.
To prevent MPS diseases, men are recommended, first of all, to avoid excessive physical activity. You need to drink more fluids, especially in hot weather. And most importantly, limit yourself to smoking and drinking alcohol, which leads to narrowing of blood vessels and increased permeability of their walls.
Therapy of pathologies of the genitourinary system
Treatment of red urine in men, or rather, the types of medications, duration of the course, and the need for hospitalization depend entirely on the type of disease:
- Infectious diseases require antibacterial therapy.
- Traumatic injuries are eliminated with anti-inflammatory, hemostatic agents along with massage and physiotherapeutic procedures.
- Urolithiasis, prostatitis, and glomerulonephritis are difficult to treat and require an integrated approach.
Surgery is recommended if tumors are detected. With medication you can only stop their growth, but cannot destroy them. The same applies to large kidney stones, against which medications are powerless.
Attention! If a change in the color of urine is detected, you should consult a urologist.
What is included in the complex
- Cyfra 21-1 in urine
- Chlamydia, DNA (Chlamydia trachomatis, PCR) urine, count.
- Ureaplasma, DNA (Ureaplasma species, PCR) urine, count.
- Mycoplasma, DNA (Mycoplasma genitalium, PCR) urine, count.
- Mycoplasma, DNA (Mycoplasma hominis, PCR) urine, count.
- Gardnerella, DNA (Gardnerella vaginalis, PCR) urine, count.
- Trichomonas, DNA (Trichomonas vaginalis, PCR) urine, count.
- Gonorrhea, pathogen DNA (Neisseria gonorrhoeae, PCR) urine, count.
- Candida, DNA (Candida albicans, PCR) urine, count.
- Herpes virus types 1,2, DNA (HHV-1,2, PCR) urine, count.
- Cytomegalovirus, DNA (Cytomegalovirus, PCR) urine, count.
- General urine analysis
Clinical picture
Urine that is reddish in color, due to the presence of red blood cells, unused hemoglobin, myoglobin, or porphyrin, is considered primarily a symptom rather than a disease. And first it is recommended to find out why there is red color in the urine.
This may not be associated with pathological changes. For example, athletes, after heavy exercise, experience muscle tissue release, which causes reddish urine.
In addition, blood can appear from hemorrhoids, penetrating into the urine. But this is determined quite simply, because in this case the feces also turn red.
There are even medical procedures after which blood is likely to appear in the urine.
Why is urine red in men?
In addition to the general causes of hematuria in men, it can also occur due to:
- prostatitis or stagnation of blood in the prostate;
- scrotal injuries;
- injuries of the urethra;
- prostate cancer.
The nature of the lesion can be recognized by the color of the urine. If it is dark in color (red-brown, brown), then blood has entered the urine from the kidneys. If the color of the urine is bright red, it means blood is being released from the urinary or genital tract. In this case, there may be small blood clots.
When contacting a doctor, try to tell about additional symptoms - weakness, fatigue, swelling, shortness of breath, injury, infectious diseases, urination problems. In serious diseases, hematuria is not the only symptom. In addition, the doctor will ask you about your appetite and drinking habits, medications, allergies
Important information will be the time of onset of symptoms and their duration