Currently, urinary incontinence is understood as the involuntary release of urine from the urethra without the urge to urinate. Enuresis is persistent involuntary urination that occurs in an individual at different times of the day (night, day, combined) due to various etiological reasons.
In turn, primary nocturnal enuresis is urinary incontinence at night, which was not preceded by at least a 6-month period of bladder control in a child aged 5 years or more [1]. Primary nocturnal enuresis must in all cases be differentiated from secondary enuresis, as well as from other urination disorders, since the scope and choice of diagnostic and therapeutic measures are different [1-3].
It's hard to believe, but by the end of the 20th century. More than half a billion people worldwide suffered from urinary incontinence, and primary nocturnal enuresis was the most common among them [4]. In the pediatric population, it also predominates among other urinary disorders. The so-called age-dependence of this pathological condition is reflected in its prevalence among various age groups. Among 5-year-old children, about 10% suffer from enuresis, 5% of 10-year-olds, and by 14 years of age it affects 2%. Nevertheless, nocturnal enuresis occurs with significant frequency in adults. Thus, among individuals over 18 years of age, its prevalence is 1%, and among individuals over 18 years of age it affects about 0.5% [4, 5]. It is known that nocturnal enuresis is more typical for boys; in them it occurs 1.5-2 times more often than in girls.
When diagnosing primary nocturnal enuresis, one must first distinguish the primary (persistent) form from the secondary (acquired) form. Secondary nocturnal enuresis appears after a period of stable urinary control (at least 6 months).
In the relatively recent past, some confusion that occurred in terminological, diagnostic and therapeutic approaches to the problem of enuresis prevented the implementation of adequate diagnostic and therapeutic measures for various types of this urination disorder in childhood. Currently, such forms of nocturnal enuresis as, for example, functional and organic, neurotic or neurosis-like are rarely considered. The terms listed above are outdated and are of primarily historical interest.
Experience with the use of the drug minirin (desmopressin) in Russia
In 2002, the Russian Federation gained experience with the use of the drug minirin, a tablet form of desmopressin. During the multicenter testing of this drug, in which leading research and medical institutions in Moscow were involved, representatives of various pediatric specialties were involved in the research: pediatricians, pediatric neurologists, urologists, nephrologists and endocrinologists [15].
In total, Minirin (0.2 mg tablets) was prescribed to 65 children aged 5-14 years (47 boys, 18 girls) with a diagnosis of primary nocturnal enuresis. Of these, 16 children were treated as inpatients in specialized departments, and 49 patients received the drug on an outpatient basis. The clinical testing protocol used in institutions participating in the clinical testing of the drug included a whole group of requirements for the study being conducted and the patients being observed:
- age of children over 5 years;
- established diagnosis of primary nocturnal enuresis;
— absence of inflammatory diseases of the genitourinary system (GUS);
— absence of congenital and/or psychogenic (pathological) polydipsia;
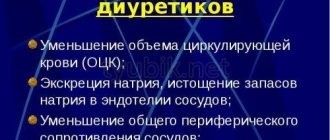
- absence of cardiovascular failure and other conditions requiring the use of diuretics;
- absence of mental retardation;
- absence of taking (any) anticonvulsants;
- absence of taking medications that have a diuretic effect;
- lack of taking antibacterial agents;
— absence of taking (other) hormonal medications;
— absence of taking drugs that have a pronounced sedative effect;
- lack of physiotherapeutic procedures during treatment with Minirin;
— absence of acute respiratory diseases (ARI) and exacerbations of somatic diseases.
The spectrum of concomitant pathology in the observed children with primary nocturnal enuresis was extremely wide: among psychoneurological disorders there were tic disorders, attention deficit hyperactivity disorder, minimal brain dysfunction, post-traumatic cerebrasthenic syndrome, various cephalgic syndromes, etc., and among somatic pathological conditions there were diseases with aspects of the cardiovascular system (sinus arrhythmia, mitral valve prolapse), MPS (incomplete renal duplication, dysmetabolic nephropathy), ENT organs (chronic tonsillitis, adenoid vegetations, etc.), allergic diseases (atopic dermatitis, bronchial asthma), diseases of the gastrointestinal tract (chronic gastroesophagitis, gastroesophageal reflux, biliary dyskinesia, chronic cholecystitis, chronic constipation, etc.) etc.
Minirin (desmopressin) was prescribed to children at an initial dose of 0.2 mg (1 tablet) once (in the evening). If there was no positive effect, the dose was increased by 0.1 mg (1/2 tablet) once every 5-6 days. The maximum permissible dose of minirin was 0.4 mg (2 tablets). The duration of treatment in our observations was 6 weeks. Among the general recommendations, it was practiced to limit the intake of any liquid after 19:00.
Before starting desmopressin therapy, all children were examined as follows:
- general urine analysis;
- general blood analysis;
- biochemical blood test (creatinine, urea, bilirubin, ALT, AST, glucose, Na, K, Ca, etc.);
— Zimnitsky test;
— ultrasound examination (ultrasound) of the kidneys and bladder;
— determination of the volume and rhythm of urination;
— electroencephalographic study.
Similar studies (excluding ultrasound of the kidneys and bladder) were carried out upon completion of the course of treatment with Minirin.
If the drug was missed 5 times or more (over a 6-week period), patients were excluded from the observation group.
To assess the clinical effectiveness of minirin, 4 rubrics were used:
- no effect;
- partial effect (i.e. reduction in the frequency of episodes of nocturnal enuresis by 25-30%);
- significant improvement (reduction in the frequency of episodes of nocturnal enuresis by more than 50%);
- complete remission (100% effect - complete elimination of episodes of nocturnal enuresis while taking the drug).
The clinical effect was assessed against the background of the maximum achieved dose of the drug, selected individually (but not more than 0.4 mg of desmopressin per day). At the same time, the frequency of episodes of nocturnal enuresis in patients was compared with that before the start of treatment (according to parents).
After excluding 5 patients from the observation group (due to low compliance - 3 children, the presence of mental retardation - 1 patient, detection of epilepsy with partial seizures - 1 child), the results of treatment of 60 children with primary nocturnal enuresis were analyzed. Most patients continued to take various medications (in addition to desmopressin): biotredin, elkar, tanakan, picamilon, glycine, flamin, duphalac, claritin, as well as multivitamin preparations. Only 21 (35%) children did not receive any medications other than Minirin during the 6-week follow-up period.
Only in 3 (5%) cases was there no effect. Partial improvement occurred in 6 (10%) patients, and significant improvement in 20 (33.3%) children. Complete remission was achieved in 31 (51.7%) children. The clinical effectiveness of minirin in tablet form was not inferior and even slightly higher than that of the nasal form of desmopressin in drops (adiuretin-SD): overall, effectiveness was demonstrated in 95% of patients.
Pediatric urologists especially emphasize that 100% effectiveness of treatment with the drug was achieved in children with a normal urination rhythm and increased nighttime diuresis (1.5-2 times compared to daytime). It was found that an increase in effective bladder capacity was noted after approximately 1 month. after starting to take the drug, and after another 2 weeks. There was a complete cessation of enuresis.
The lack of clinical effect in 5% of children with primary nocturnal enuresis appears to confirm the hypothesis that there are several subtypes of this pathological condition, one of which is characterized by the absence of any response to treatment with desmopressin.
As for adverse reactions to therapy, during clinical testing of the drug Minirin, in 1 case an exacerbation of atopic dermatitis was noted, and in 1 child recurrent abdominal pain was noted (the child was found to have chronic gastroduodenitis and biliary dyskinesia). Moderate drowsiness was noted in 2 children while taking Minirin. There were no cases of headache, nausea, vomiting, intestinal disorders, or seizures. Thus, drug tolerability was assessed as good in 58 (96.7%) patients, and satisfactory in 2 (3.3%) children.
The results of a multicenter study led to the conclusion that minirin (desmopressin) in tablet form can be used in the treatment of primary nocturnal enuresis in patients over 5 years of age (at a dose of 0.2-0.4 mg per day), both as monotherapy and as part of complex treatment. The minimum recommended course for treatment with desmopressin for this type of urinary pathology is 6 weeks, but if necessary, it can be extended to 3 (or even 6) months.
Minirin in pediatric practice
M
inirin (desmopressin, 1-desamino-8-0-arginine-vasopressin) is a synthetic analogue of the natural antidiuretic hormone of the posterior pituitary gland arginine-vasopressin, which regulates water reabsorption, acting directly on the kidneys.
In terms of structure, Minirin has two fundamental differences from vasopressin: the absence of an amino group at position 1 and the replacement of D-arginine at position 8. These modifications increase the resistance of the Minirin molecule to enzymatic degradation, enhance antidiuretic activity and eliminate the vasopressor effect (does not affect smooth muscles). Thus, Minirin has a more powerful prolonged antidiuretic effect
.
After taking tableted Minirin, it begins to be detected in the blood plasma within 15–30 minutes. The maximum concentration is reached no later than 2 hours after taking the drug (Baylis R.N., 1975; George CP et al., 1975). After oral administration of desmopressin, its absorption occurs mainly in the duodenum and the proximal small intestine. If the drug passes quickly through these parts of the intestine, its absorption may be less effective (when taking Minirin with food).
Clinical studies have shown the effectiveness of tableted Minirin in patients with central diabetes insipidus (Cunnah D., et al., 1986; Westgren U. et al., 1986).
Minirin is available in tablets of 0.1 and 0.2 mg, 30 pieces per package. According to the manufacturer's recommendations, the dose of Minirin is selected individually. For patients with central diabetes insipidus, the recommended dose is 0.1–0.2 mg 2–3 times a day. The effectiveness of Minirin is increased by the correct time of taking the drug - 30 minutes before meals or 2 hours after meals (Lam KS et al., 1996). It is recommended to transfer patients from intranasal therapy with Adiuretin to oral administration of Minirin in the evening. The dose equivalent ratio for intranasal and oral forms of desmopressin varies among patients and averages 1:8 (Janknegt RA et al., 1997). In addition to diabetes insipidus, Minirin is used in the treatment of enuresis in children.
In the children's department of the Endocrinological Research Center (ERC) of the Russian Academy of Medical Sciences, in January–May 2002, an open post-marketing study was conducted to develop a regimen for the use of a tablet form of desmopressin (Minirin) for the treatment of diabetes insipidus of central origin in children and adolescents.
The group examined consisted of 15 patients (8 boys, 7 girls). Chronological age averaged 13.1±4.0 years (5.0–21.0), most patients were between 9 and 17 years old, two patients were aged 20–21 years. Bone age averaged 10.4±3.9 years (4.0–18.0). The clinical status of the patients at the time of the initial examination is presented in Table 1. The distribution of patients by age and gender is presented in Table 2.
The etiology of central diabetes insipidus included craniopharyngioma in 14 patients (93%) and chorionic carcinoma of the pineal and chiasmal-sellar region in one girl (7%). All patients underwent surgery for these brain tumors at the Institute of Neurosurgery named after. N.N. Burdenko, (Moscow). A girl with chorionic carcinoma of the pineal and chiasmal-sellar region had combined therapy: surgical treatment and radiation therapy. The average duration of central diabetes insipidus in the group was 4.94±1.12 years (1.0–16.0), the average duration of treatment for diabetes insipidus with Adiuretin-SD was 4.68±1.15 years (1.0–16 ,0).
The hormonal status of the examined patients is presented in Figure 1. 12 patients (80%) had panhypopituitarism, 3 patients (20%) had hypopituitarism. Panhypopituitarism was characterized by loss of GH/TSH/ACTH/ADH (antidiuretic hormone) and LH, FSH in four patients with pubertal bone age. Two patients had hypopituitarism with GH/TSH/ADH deficiency and preserved corticotroph function. One patient with pubertal bone age had a deficiency of GH/TSH/ADH/ACTH and spontaneous puberty.
Rice. 1. Hormonal status in the studied group of children with central diabetes insipidus
In addition to the studies presented above, the adequacy of hormone replacement therapy was assessed based on a standard clinical examination by an endocrinologist at the pediatric department of the Endocrinology Center of the Russian Academy of Medical Sciences.
At the time of the initial examination, all patients were compensated with appropriate hormones. Diabetes insipidus in patients was relatively compensated by Adiuretin, the dose of which ranged from 1 to 3 drops per day (1 drop of Adiuretin contains 5 mcg of the drug). In urine tests according to Zimnitsky, significant fluctuations in daily diuresis and urine specific gravity were noted during the day.
According to the manufacturer's recommendations, Minirin (0.1 mg/0.2 mg) tablets were prescribed 30–40 minutes before meals or 2 hours after meals. An adequate dose of Minirin was selected mainly during the first 3–4 days of treatment.
The daily dose of Minirin in the study group was on average 0.35±0.2 mg, fluctuations ranged from 0.06 to 0.8 mg (Fig. 2). In the majority of patients (11 people, 73%), the daily dose of Minirin was 0.1–0.4 mg. Three patients suffering from concomitant diencephalic obesity received 0.5–0.8 mg of Minirin per day. One patient received 0.06 mg of Minirin per day. There was no correlation between the age of the patients and the daily dose of Minirin. Thus, a 5-year-old patient received 0.2 mg of Minirin per day, and a 16-year-old patient received 0.06 mg of Minirin per day.
Rice. 2. Daily dose of Minirin in children and adolescents with central diabetes insipidus
The frequency of administration of Minirin was 2–3 times a day (morning – afternoon – evening), and the distribution of patients receiving the drug in a two-time (53%) and three-time (47%) mode was almost uniform (Fig. 3). In 4 patients (27%), the frequency of desmopressin intake per day was increased from 2 times the use of intranasal Adiuretin to 3 times the use of tablet Minirin.
Rice. 3. Frequency of administration of Minirin in children with central diabetes insipidus
Analysis of the ratio of the dose equivalent of intranasal Adiuretin and tablet Minirin in the studied cohort of patients showed that in 7 patients (47%) 1 drop of Adiuretin corresponded to 0.1–0.15 mg of Minirin, in 8 patients (53%) 1 drop of Adiuretin-SD corresponded 0.2–0.25 mg Minirin (Fig. 4). The average daily dose of Adiuretin was 9.8±2.7 mcg, the average dose of Minirin was 350.7±195.3 mg.
Rice.
4. Correspondence of the dose of Minirin and Adiuretinau for children and adolescents with central diabetes insipidus Results of treatment with Minirin
During treatment with Minirin tablets in the studied group of children and adolescents with central diabetes insipidus, a pronounced positive effect of the drug
– both clinical and according to laboratory studies.
Thus, during therapy with Minirin, thirst and polyuria were absent in patients. All patients noted the significant convenience of taking tableted Minirin compared to intranasal Adiuretin, which somewhat increased their psychological tone and quality of life. According to the children and their parents, when intercurrent catarrhal diseases occurred, the advantage of tablet Minirin was undeniable (during the study, three patients suffered an acute respiratory disease). During treatment with Minirin tablets, the study group of children and adolescents with central diabetes insipidus was diagnosed, both clinically and according to laboratory tests.
Thus, during therapy with Minirin, thirst and polyuria were absent in patients. All patients noted the significant convenience of taking tableted Minirin compared to intranasal Adiuretin, which somewhat increased their psychological tone and quality of life. According to the children and their parents, when intercurrent catarrhal diseases occurred, the advantage of tablet Minirin was undeniable (during the study, three patients suffered an acute respiratory disease). Diuresis during treatment with Adiuretin ranged from 1.2 to 3 liters per day, during treatment with Minirin - from 1.1 to 2.1 liters per day. In urine tests according to Zimnitsky during treatment with Minirin, low specific gravity in individual portions was less common.
To illustrate the positive effect of Minirin in the treatment of patients with central diabetes insipidus, we present two clinical observations.
The first patient, 13 years old (Table 3), during treatment with Adiuretin 1/2 drop x 3 times a day, had a daily diuresis of 1330 ml, with fluctuations in the specific gravity of urine 1003–1021. When switched to 0.3 mg of Minirin (0.1 mg x 3 times a day), daily diuresis was 1160 ml, the specific gravity of urine ranged from 1008 to 1021. There was no thirst during 2 months of treatment with Minirin.
The second patient, 21 years old (Table 4), before taking Minirin, excreted more than 3 liters of urine, with fluctuations in the specific gravity of urine from 1002 (3 portions) to 1020. The dose of Adiuretin was 2 drops per day (1 drop x 2 times a day) .
When the patient was transferred to Minirin at a daily dose of 0.15 mg (0.05 mg x 3 times a day), daily diuresis decreased to 1980 ml, the specific gravity of urine ranged from 1004 (1 serving) to 1016. Side effects
Side effects and complications on During treatment with Minirin, children and adolescents with central diabetes insipidus were practically not detected. Only three patients out of 15 (20%) examined experienced side effects during the first 3–4 days of dose selection.
Side effects and complications during treatment with Minirin in children and adolescents with central diabetes insipidus were practically not detected. Only three patients out of 15 (20%) examined experienced side effects during the first 3–4 days of dose selection.
One 5-year-old boy, while taking 0.2 mg (0.1 mg x 2 times a day) of Minirin per day, experienced some fluid retention - daily diuresis decreased to 600 ml, with an increase in the specific gravity of urine to 1042–1058. There were no clinical equivalents of these laboratory parameters (edema, disturbances in general well-being). When the dose was reduced, these laboratory changes disappeared.
Two boys, 13 and 15 years old, experienced swelling on the face in the first days of taking Minirin at a dose of 0.1 mg x 3 times a day. In one patient, the previous dose of Adiuretin was 3 drops per day, in the second patient the previous dose of Adiuretin was 2 drops per day. With a minimal reduction in the dose of Minirin, these side effects quickly disappeared.
conclusions
1. The tablet form of desmopressin – the drug “Minirin” 0.1/0.2 mg (“Minirin”, Ferring) has a pronounced antidiuretic effect in children and adolescents with central diabetes insipidus.
2. Minirin has no side effects.
3. The duration of action of Minirin is from 8 to 12 hours, and therefore the frequency of dosing of the drug should be 2-3 times a day.
4. For better absorption, Minirin should be taken 30–40 minutes before meals or 2 hours after meals.
5. The ratio of the dose equivalent of intranasal Adiuretin and tablet Minirin in 47% of patients is 1 drop of Adiuretin: 0.1–0.15 mg of Minirin, in 53% of patients – 1 drop of Adiuretin: 0.2–0.25 mg of Minirin.
6. The dose of Minirin should be selected individually for each patient. Treatment should begin with a lower ratio of Adiuretin and Minirin (1 drop of Adiuretin - 0.1 mg Minirin), followed by increasing the dose according to the presence of thirst and diuresis and specific gravity of urine.
7. Particular attention should be paid to the first 2–3 days of taking Minirin, when an overdose may cause short-term swelling of the face and slight fluid retention with an increase in the specific gravity of urine.
8. In obese patients, the need for Minirin is increased.
9. The advantage of using the tableted drug “Minirin” compared to the intranasal drug “Adiuretin” (especially for catarrhal symptoms) was noted by all patients.
10. When using Minirin, there is no such effect as atrophy of the nasal mucosa, which is typical for intranasal forms.
Pharmacological properties of the drug Minirin
Minirin tablets contain desmopressin - a synthetic analogue of the natural hormone of the posterior lobe of the pituitary gland - arginine vasopressin (antidiuretic hormone). Desmopressin was obtained as a result of changes in the structure of the vasopressin molecule: deamination of 1-cysteine and replacement of 8-L-arginine with 8-D-arginine. Compared with vasopressin, desmopressin has a minor effect on vascular smooth muscle with more pronounced antidiuretic activity. Thanks to the described structural changes, Minirin activates only V2 vasopressin receptors located in the epithelium of the convoluted tubules and a wide part of the ascending loops of Henle, which causes an expansion of the pores of nephron epithelial cells and leads to increased reabsorption of water into the bloodstream. After taking the drug, the antidiuretic effect occurs within 15 minutes. Taking 0.1–0.2 mg of desmopressin provides an antidiuretic effect lasting up to 8–12 hours in most patients. The use of Minirin in patients with an established diagnosis of diabetes insipidus of central origin leads to a decrease in the volume of urine excreted and a concomitant increase in its osmolarity. As a result, the frequency and severity of nocturia decreases. No teratogenic or mutagenic effects of desmopressin have been identified. Desmopressin begins to be detected in the blood 15–30 minutes after administration. The maximum concentration in the blood plasma is reached after 2 hours. The half-life of desmopressin in the blood plasma is 1.5–3.5 hours. The drug is excreted in the urine, partly unchanged, partly after enzymatic breakdown.
Overdose of the drug Minirin, symptoms and treatment
Overdose increases the risk of hyponatremia and fluid retention in the body. Although treatment for hyponatremia must be individualized, there are general recommendations:
- in case of asymptomatic hyponatremia, treatment with Minirin should not be interrupted and the patient’s fluid intake should be further limited;
- in case of symptoms caused by hyponatremia, an iso- or hypertonic solution of sodium chloride should be administered intravenously;
- in severe cases of fluid retention in the body, manifested by convulsions and/or loss of consciousness, furosemide should be included in complex (symptomatic) therapy.