Renal colic (RC) develops as a result of an acute violation of the outflow of urine through the upper urinary tract - the renal collecting system and the ureter. Although we often associate PC with urolithiasis, the causes of impaired urine outflow can be very different: tumor process, inflammation, papillary necrosis, etc.
- Emergency treatment
- Infusion therapy
- Antibacterial therapy
- Survey
- Further treatment
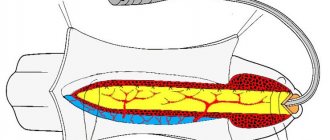
In response to increased intrarenal pressure, the interstitial cells of the renal medulla release prostaglandin E2, which in turn increases renal blood flow to maintain the glomerular filtration rate. Which leads to a further increase in intrapelvic pressure and the development of pain. Stretching of the upper urinary tract stimulates contraction of the smooth muscle fibers of the ureter, which will vigorously cease to move to advance the obstruction that caused the obstruction. These prolonged muscle contractions lead to a buildup of lactic acid, which stimulates pain receptors. Renal colic is characterized by acute, unbearable pain in the kidney area. The pain can radiate to the back, groin, iliac region, causing the patient to rush around and change body position.
In most cases, pain is accompanied by nausea and vomiting, which makes it impossible to take enteral medications, and in some cases leads to significant dehydration of the patient. Also characteristic is a combination of pain with the urge to urinate and gross hematuria.
Emergency treatment
Anesthesia
Diagnostic procedures must be preceded by the elimination or reduction of pain. Most experts believe that unless there are contraindications, the best initial treatment option is the use of nonsteroidal anti-inflammatory drugs (NSAIDs). Their effectiveness is associated with inhibition of the synthesis of prostaglandin E2 in the kidneys, which helps to reduce renal blood flow and reduce urine production and intrapelvic pressure.
Due to the anti-inflammatory effect, NSAIDs reduce swelling in the occlusion area. Compared to narcotic analgesics, they are less likely to cause nausea and vomiting and do not depress breathing. But there is a certain problem - there is a small choice of drugs that can be administered intravenously.
Use one of the drugs:
- Ketoprofen (Ketonal) has a pronounced anti-inflammatory and analgesic effect. Intravenously - infusion of 100-200 mg in 100 ml of physiological sodium chloride solution for 0.5-1 hour every 8 hours;
- Diclofenac. More often, 75 mg of the drug is administered intramuscularly. If necessary, the injection can be repeated, but not earlier than 30-60 minutes after the first injection. Some manufacturers allow intravenous administration of diclofenac. In any case, intravenous administration is carried out in the form of a drip infusion;
- Metamizole (Analgin) has a predominantly central mechanism of analgesic action. It has an active antispasmodic effect and weak anti-inflammatory activity. 1000-2000 mg is administered intravenously, then 1000 mg 2-3 times a day.
- Ketorolac 30 mg IV slowly (no faster than 15 seconds) for adults under 65 years of age and children over 16 years of age. Then, if necessary, 10-30 mg every 6 hours. Has a weak anti-inflammatory effect.
- Baralgin, a combined analgesic and antispasmodic drug. The combination of the components of the drug leads to a mutual enhancement of their pharmacological action. Metamizole sodium is a pyrazolone derivative that has an analgesic and antipyretic effect. Pitophenone hydrochloride has a direct myotropic effect on smooth muscles (papaverine-like effect). Phenpiverinium bromide has an m-anticholinergic effect and has an additional myotropic effect on smooth muscles. Inject slowly 2 ml intravenously. If necessary, re-introduce after 6-8 hours. The daily dose should not exceed 10 ml.
Need to remember:
- That parenteral forms of these drugs should not be used for more than 1-3 days.
- If the pain syndrome persists, therapy is continued using tablet forms of NSAIDs.
- That nonsteroidal anti-inflammatory drugs, with the exception of metamizole (Analgin), are contraindicated for destructive inflammatory bowel diseases in the acute phase, “aspirin-induced” bronchial asthma, and in the last trimester of pregnancy. In addition, they should be used with caution in patients with arterial hypertension, impaired renal function and heart failure.
If the pain syndrome is not sufficiently controlled by taking NSAIDs, narcotic analgesics are prescribed:
- Morphine. To reduce the likelihood of side effects (respiratory depression, hypotension), 10 mg of morphine is diluted in 10 ml of 0.9% sodium chloride and administered intravenously at 2-3 ml intervals of 5 minutes, or use a dispenser;
- Trimeperidine (Promedol), unlike morphine, depresses the respiratory center to a lesser extent and is less likely to cause nausea and vomiting. Inferior to morphine in analgesic activity. Prescribe 10-20 mg intravenously, it is safer to administer in small doses.
If pain persists:
Lidocaine IV 1.5 mg/kg, administer the dose no faster than 5 minutes. Has analgesic and antispasmodic effects;
Desmopressin (Minirin). Taking 20 mcg of desmopressin intranasally or 200 mcg orally or as sublingual tablets provides an antidiuretic effect lasting 8-12 hours in most patients. And provides an effective reduction in intrapelvic pressure;
Causes and symptoms
Before you begin to relieve renal colic, you need to understand the cause of its occurrence and the characteristics of its manifestation.
An attack characterized by sudden pain occurs due to the following pathological changes in the body:
- The presence of tumor processes in the kidney tissues;
- Movement of stones in the urinary tract system;
- Kidney damage due to mechanical stress;
- Renal tuberculosis;
- Excessive physical activity;
- Alcohol abuse;
- Narrow lumen in the ureter;
- Formations of a benign or malignant nature in the uterine region, thyroid gland or in the digestive tract;
- Kidney prolapse.
With these diseases, the kidneys often hurt, and a sharp attack of pain can strike at any moment.
However, when providing assistance for renal colic, it is important to know not only about the presence of pathological changes, but also about the reasons that caused them:
- Stones that are in the kidneys;
- Blood lumps formed in the kidney space;
- Plugs of pus in the urinary tract;
- Bend or swelling in the ureter.
If there is no information about the clinical picture of the disease, emergency care for renal colic is provided based on the symptoms of the attack.
- Sharp, severe pain during spasm, which can cause fainting or painful shock.
- Blood clots appear in the urine.
- Without first aid, the pain felt in the abdomen, groin and sides intensifies.
- When the bladder is emptied, little or no urine comes out.
- Inability to defecate.
If kidney function is impaired, the symptoms intensify and manifest themselves in the following disorders:
Manifestations of pain when urinating;
- Dizziness;
- Rapid increase in body temperature and blood pressure;
- Nausea;
- Vomit.
Note!
Important symptoms of colic are the inability to eliminate pain when changing body position and its paroxysmal nature.
The duration of the attack depends on the individual characteristics of the body, as well as the reasons that caused renal colic. Thus, cases of colic have been recorded that lasted from 2 hours to 3 days.
These symptoms require immediate medical intervention, and first aid is used to relieve pain.
Nausea and vomiting
For nausea and vomiting, selective blockers of serotonin 5-HT3 receptors are most effective: tropisetron 5 mg once a day IV or ondansetron 4-8 mg twice a day IV. But the high cost limits the possibility of using these drugs. Droperidol, used in a dose of 0.6-1.2 mg IV 1-3 times a day, is practically safe (almost does not prolong the QT interval) and is quite effective for the treatment and prevention of PONV. If higher doses are used, the risk of droperidol side effects increases dramatically. Dopamine receptor blocker metoclopramide hydrochloride (Cerucal), administered 10 mg 3-4 times a day intravenously.
Surgery
The use of surgical treatment is performed in case of ineffectiveness of drug therapy. Also, the reason for surgical intervention may be wrinkling and hydrocele of the kidney, complications of urolithiasis and stones larger than 1 cm.
Before undergoing surgery to remove stones, the patient must undergo several procedures:
- donate blood and urine for analysis;
- do fluorography;
- undergo ultrasound and x-ray examination;
- consult a physician to determine possible allergic reactions;
- follow a diet to avoid bloating and stool formation.
Nowadays, there are several productive methods for surgically removing stones from the urinary tract with the least shock to the body.
Survey
After the pain has reduced, the patient is examined.
Laboratory methods
General blood analysis. Changes in indicators in general are not typical for renal colic. In dehydrated patients, the hemoglobin concentration and the number of red blood cells may increase.
Creatinine, urea. High rates are a contraindication for excretory urography and the prescription of NSAIDs;
General urine analysis. Erythrocyturia occurs in approximately 80% of patients with renal colic. Leukocyturia and bacteriuria indicate the presence of a urinary tract infection.
Instrumental examination methods
Ultrasound examination of the kidneys and upper urinary tract is the most accessible method to detect stones in the kidneys, upper and, in some cases, lower third of the ureter, as well as dilation of the collecting system. It should be noted that in approximately 25% of patients no pathological changes or expansion of the collecting system are found, which requires additional research methods.
Non-contrast spiral computed tomography (CT) - this method provides the most complete information about the cause of the obstruction that caused the development of PC. And, at the same time, identify/exclude many diseases of the abdominal organs.
Excretory urography, until recently the “gold standard” in the diagnosis of PC, is currently performed when CT is not possible. Excretory urography can detect radiopaque stones in the urinary tract. During an attack of renal colic, when there is a segmental spasm of the pyelocaliceal or ureteric muscles with a simultaneous weakening of blood flow in the cortical zone of the renal parenchyma, the contrast agent is not secreted by the kidney, which is noted on the urogram as a sign of the so-called “silent kidney”. But if the increase in intrapelvic pressure is not so critical (65-100 mm Hg), then the images clearly reveal a nephrogram (the so-called “white kidney”), indicating the impregnation of the renal parenchyma with a contrast agent, but without its penetration into the upper urinary tract ;
Retrograde ureterography is indicated in difficult cases of differential diagnosis between renal colic and diseases of the abdominal organs, when the results of spiral computed tomography and excretory urography are ambiguous.
Clinical picture and complications of renal colic
In general, about 3% of the world's population suffers from urolithiasis.
Urolithiasis affects people of all age groups. In young and middle-aged people, urinary stones often form in the ureters and kidneys, and in older people and children - in the bladder.
One of the most severe and dangerous conditions associated with urolithiasis is renal colic.
Definition 1
Renal colic is a sharp, paroxysmal pain caused by acute obstruction of the upper urinary tract.
An attack of renal colic is characterized by the following symptoms:
- Sudden, constant cramping pain in the lumbar region and/or hypochondrium. Its duration varies from a few minutes to 10-12 hours. The pain is especially intense in the first 1.5-2 hours; it forces the patient to constantly change body position and rush about. The patient holds his hand on the lower back on the side of pain, but this usually does not bring relief. The pain spreads along the ureter to the inguinal and iliac regions, to the area of the external genitalia. The characteristics of pain irradiation are determined by the localization of stones; most often they stop at places of physiological narrowing of the ureter.
- Dysuric disorders (non-persistent).
- Other common symptoms are: vomiting that does not bring relief and nausea, which occur almost simultaneously with lower back pain); retention of stool and gases; dizziness and fainting; moderate increase in blood pressure; bradycardia; oligo- and anuria; hematuria.
Finished works on a similar topic
Course work Urolithiasis. The role of the paramedic in providing care at the prehospital stage 420 ₽ Abstract Urolithiasis. The role of the paramedic in providing assistance at the prehospital stage 240 ₽ Test work Urolithiasis. The role of a paramedic in providing care at the prehospital stage 240 ₽
Receive completed work or specialist advice on your educational project Find out the cost
In the absence of timely qualified medical care, an attack of renal colic can lead to the development of complications: acute obstructive pyelonephritis; bacteremic shock; urosepsis; decreased kidney function; formation of ureteral stricture.