Many diseases remain without proper attention and often go away on their own. However, in some cases, minor discomfort when urinating may indicate that a source of inflammation has arisen in the body. Cystitis is one of those diseases that can not only significantly worsen a woman’s quality of life, but can also be a sign of a much more serious illness.
Effective treatment of cystitis in women requires an integrated approach, including drug therapy, diet and regular monitoring of the condition.
The cause of this disease is conditionally pathogenic microflora. The immune system of the human body regulates its growth and numbers. However, a failure in the functioning of protective mechanisms can provoke an imbalance of bacteria, causing an inflammatory process.
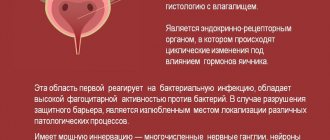
Cystitis occurs more often in women than in men. This is due to the anatomical features of the structure of the female genitourinary system. The short, wide and straight urethra of a woman facilitates the unhindered penetration of pathogenic flora into the bladder. In addition, the proximity of the rectum and vagina, sources of bacteria, is another factor contributing to infection.
Cystitis: causes
- neglect of hygiene rules;
- promiscuous sex life;
- tight underwear;
- pregnancy (in later stages);
- hypothermia;
- blood stagnation in the pelvic area (for example, during sedentary work);
- frequent constipation;
- poor nutrition;
- the presence of hidden foci of infection in the body;
- elderly age.
Based on the nature of its origin, cystitis is usually divided into primary and secondary. The cause of primary cystitis in most cases is E. coli, which invades the bladder mucosa. Secondary cystitis occurs against the background of other diseases.
The following diseases can cause the development of secondary infection:
- malignant neoplasms of the kidneys, bladder, urinary tract;
- gynecological pathologies;
- sexually transmitted diseases.
Sources
- Laden BF., Bresee C., De Hoedt A., Dallas KB., Scharfenberg A., Saxena R., Senechal JF., Barbour KE., Kim J., Freedland SJ., Anger JT. Comorbidities in a Nationwide, Heterogenous Population of Veterans with Interstitial Cystitis/Bladder Pain Syndrome. // Urology - 2021 - Vol - NNULL - p.; PMID:33901534
- Williams WV., Brind J., Haynes L., Manhart MD., Klaus H., Lanfranchi A., Migeon G., Gaskins M., Seman EI., Ruppersberger L., Raviele KM. Hormonally Active Contraceptives Part I: Risks Acknowledged and Unacknowledged. // Linacre Q - 2021 - Vol88 - N2 - p.126-148; PMID:33897046
- Feng Z., Shi H., Liang B., Ge T., Cai M., Liu F., Huang K., Wen J., Chen Q., Ge B. Bioinformatics and experimental findings reveal the therapeutic actions and targets of pachymic acid against cystitis glandularis. // Biofactors - 2021 - Vol - NNULL - p.; PMID:33893687
- Shin JH., Kang B., Choo MS. Features of Various Bladder Lesions and Their Impact on Clinical Symptoms and Recurrence in Interstitial Cystitis. // J Urol - 2021 - Vol - NNULL - p.101097JU0000000000001811; PMID:33890486
- Famularo G., Galluzzo M. Encrusted cystitis. // Intern Emerg Med - 2021 - Vol - NNULL - p.; PMID:33890207
- Mixon MA., Dietrich S., Bushong B., Peksa G., Rogoszewski R., Theiler A., Spears L., Werth J., Meister E., Martin MS. Urinary tract infection pocket card effect on preferred antimicrobial prescribing for cystitis among patients discharged from the emergency department. // Am J Health Syst Pharm - 2021 - Vol - NNULL - p.; PMID:33889933
- Kim JK., Lee YG., Han K., Han JH. Obesity, metabolic health, and urological disorders in adults: a nationwide population-based study. // Sci Rep - 2021 - Vol11 - N1 - p.8687; PMID:33888807
- Scribano D., Sarshar M., Fettucciari L., Ambrosi C. Urinary tract infections: Can we prevent uropathogenic Escherichia coli infection with dietary intervention? // Int J Vitam Nutr Res - 2021 - Vol - NNULL - p.1-5; PMID:33880966
- Zhang B., Chen L., Zhou J., Zu Y., Gui R., Li Z., Wang J., Yu F., Zhang Y., Zhao H., Ji Z., Song Y. Ruxolitinib early administration reduces acute GVHD after alternative donor hematopoietic stem cell transplantation in acute leukemia. // Sci Rep - 2021 - Vol11 - N1 - p.8501; PMID:33875780
- Cernat M., Skampardonis V., Papadopoulos GA., Kroustallas F., Chalvatzi S., Petridou E., Psychas V., Marouda C., Fortomaris P., Leontides L. Urinary tract infections in culled sows from Greek herds: prevalence and associations between findings of histopathology, bacteriology and urinalysis. // Porcine Health Manag - 2021 - Vol7 - N1 - p.33; PMID:33875002
Diagnosis of cystitis
The clinical picture of cystitis is characterized by sudden onset and is accompanied by a slight increase in temperature - from 370C to 370C, fever, weakness, sharp pain in the lower abdomen, difficulty urinating, cloudy urine, and the presence of flakes. A characteristic symptom of cystitis is the absence of a feeling of emptying the bladder. In rare cases, nausea or vomiting may occur.
Urinary disorders in acute or chronic cystitis are usually divided according to the following criteria:
- Imperative urges. This pathological condition is characterized by a constant feeling that it is necessary to immediately empty the bladder. Often this condition is accompanied by incontinence.
- Strangury. A symptom in which the patient experiences sharp pain at the beginning and end of urination.
- Pollakiuria. With pollakiuria, the patient experiences pain when urinating and lack of sensation of completely emptying the bladder.
- Nocturia. An alarming symptom in which the volume of urine during nighttime emptying exceeds daytime.
How to treat cystitis
At the first suspicion of an inflammatory process, you should immediately contact a specialist. Diagnosis of the disease is made by a urologist. To differentiate cystitis from pathologies with a similar clinical picture and clarify the diagnosis, the following examinations are prescribed:
- general urine analysis;
- ultrasound examination of the pelvic organs;
- cystoscopy;
- vaginal flora smear;
- bacterial culture of urine;
- biopsy of the bladder mucosa (if necessary).
The standard treatment protocol for acute disease includes:
- prescription of antibacterial or antimicrobial drugs;
- prescription of uroseptics;
- phytotherapy;
- following a diet excluding spicy, salty, fermented foods;
- The drinking regime shifts towards increasing fluid intake.
For exacerbation of chronic cystitis, the treatment protocol is the same. However, in order to increase periods of conditional remission, prevention should not be neglected.
If you consult a doctor in a timely manner, drug treatment in gynecology shows good results. However, to avoid relapses, prevention should not be neglected.
Causes of cervical cystitis
Cervical cystitis has an infectious and non-infectious nature. Inflammation can develop when bacteria enter the bladder mucosa due to non-compliance with hygiene standards, hypothermia, or in the presence of other inflammatory processes in the body. A distinctive feature of cervical cystitis is that the structural features of the bladder contribute to the localization of cystitis in the cervical area. The main causative agents of infection are Escherichia coli, as well as Candida fungi, protozoa and some viruses.
The pathogen can enter the bladder:
- from the kidneys, with pyelonephritis;
- from the intestines and genitals;
- with blood flow in the presence of distant foci of inflammation in the body;
- during medical procedures, for example, when inserting a catheter or stent.
The entry of pathogenic microorganisms into the urethra and bladder is not necessarily accompanied by the development of inflammation; sometimes additional conditions are required for the onset of cystitis:
- decreased immunity;
- severe stress;
- sexual intercourse;
- the need to endure and delay urination for a long time;
- inability to perform usual hygiene procedures;
- hypothermia.
Types and forms of cystitis
Like other diseases, cystitis can be acute or chronic .
Acute cystitis
Acute cystitis manifests itself differently in all people; it can last from 2 to 10 days and occur with alternating periods of exacerbation and remission.
The acute form of cystitis is characterized by fever, chills, general weakness, difficult and painful urination. Urine comes out in small portions, sometimes requiring effort to pass it out. During urination, the patient feels a burning sensation in the urethra, and after it - a pain in the lower abdomen. In acute cystitis, a picture of general poisoning of the body may be observed (body temperature 38-40 degrees, weakness, sweating, dry mouth, thirst). This may indicate that the infection has spread to the tissues of the kidneys and renal pelvis, leading to the development of pyelonephritis. In this case, emergency medical care is required.
Chronic cystitis
Chronic cystitis is characterized by waves of exacerbation and decline of the disease. There is a frequent urge to urinate and pain when passing urine. In chronic cystitis, the symptoms are constant, only their intensity changes during treatment. Microorganisms in the urine in this form of the disease are not detected during laboratory examination. Tuberculous cystitis poses a particular danger.
Forms of cystitis in chronic form:
- latent cystitis (has hidden, implicit symptoms, characterized by the absence of obvious exacerbations);
- persistent cystitis (exacerbations occur more than 3 times a year);
- interstitial cystitis (constant, sometimes unexplained pain in the bladder, frequent exacerbations, deformation of the bladder walls).
There are also other forms of the disease - for example, postcoital cystitis ( cystitis after sex ), as well as “honeymoon cystitis” (occurs in women after defloration). The mechanism of postcoital cystitis lies in the anatomical feature of the female urethra. During sexual intercourse, vaginal mucus is thrown into the urethra, which causes irritation and inflammation. The disease can be triggered by frequent changes of sexual partners.
“Honeymoon cystitis” occurs against the background of disturbances in the vaginal microflora that already exist at the time of the onset of sexual activity. The same “thrush” can cause acute cystitis in a woman. Sexual intercourse is accompanied by abundant discharge of vaginal microflora into the urethra and bladder, which until now have not been subject to such “close” contact with infection.
1 Gynecological examination for cystitis
2 Laboratory diagnostics for cystitis
3 Ultrasound of the genitourinary tract
3. Symptoms and diagnosis
An attack of postcoital cystitis is manifested by pain in the lower abdomen and/or lower back, appearing at the end or some time after sexual intercourse. The intensity of pain can be very high. There is frequent, painful urination (especially in the final phase), sometimes with sharp pain and hematuria (the appearance of visible amounts of blood in the urine). Body temperature often rises, severe general malaise, headache, dyssomnia (certain sleep disturbances) and other general inflammatory symptoms occur.
It is easy to see that the correct diagnosis of postcoital cystitis requires, first of all, that the doctor have accurate anamnestic information from the patient: in what situations and under what circumstances attacks occur, what is the general nature of sexual activity (age of onset, number of partners, forms of activity practiced, means of contraception etc.). Laboratory tests (clinical and necessarily bacteriological) of urine, vaginal and urethral contents are prescribed. Ultrasound of the pelvic organs is informative; according to indications, specific venereal and/or urological studies are prescribed (PCR, urocystoscopy, etc.).
About our clinic Chistye Prudy metro station Medintercom page!
Sources of cystitis
In most women, cystitis is associated with infectious agents. The easy penetration of pathogens is due to the wide and short urethra, the close location of the anus, vagina and urethra (ascending tract).
In some cases, infection of the bladder occurs through the descending tract - bacteria pass from the pelvic organs, through the blood from tissues affected by inflammation. The main pathogens are presented:
- coli;
- staphylococci;
- klebsiella;
- Pseudomonas aeruginosa;
- Proteus.
Pathological processes develop in patients:
- due to vulvitis, colpitis, urethritis;
- mycoplasmosis, gonorrhea, ureplasmosis;
- trichomoniasis, chlamydia, genital tuberculosis, etc.
Primary cystitis is formed against the background of:
- hypothermia, ARVI;
- the beginning of sexual activity, frequent changes of sexual partners;
- the beginning of the menstrual cycle;
- using tight underwear;
- passion for alcohol or spicy foods.
Provoking factors for cystitis in women include pyelonephritis, congestion and stones in the bladder, urethral strictures, rare urination, and constipation. In pregnant women, the problem arises due to changes in hormonal balance and microflora in the urogenital tract. In childhood, the pathology is associated with poor hygiene and a neurogenic bladder.
The list of non-infectious factors for the development of cystitis includes:
- radiation therapy – for tumors in the pelvic organs;
- allergic reactions;
- toxic effects;
- metabolic and metabolic disorders.
The climacteric form of the disease is formed due to insufficient production of estrogen and atrophy of the mucous membrane of the genitourinary system. Sometimes the source of the disease is injuries to the outer membranes of the organ that occur during medical procedures or surgery. Chronic course occurs when the vagina or uterus is prolapsed.
The pathological process is prone to relapse; in half of the cases, a repeated episode is recorded within a year after the first attack of cystitis. If the disease manifests itself a month after recovery, then the problem is associated with secondary damage to the genitourinary tract by pathogenic microflora. Frequent complications of the disease include pyelonephritis - inflammatory processes in the kidneys. Chronic cystitis can cause the development of sclerotic changes in the organ.