Patient's feelings after surgery
Many people are concerned about the question: after a cataract is removed: is pain in the eye normal or a sign of pathology? In the first days after manipulation, damaged tissues naturally send pain signals to the nervous system. During the operation, a microscopic puncture of the cornea is made, and an ultra-thin needle is inserted. Ultrasound is applied through it and the clouded lens is destroyed. The crushed particles are removed and an artificial lens is installed. If an advanced cataract is removed, the pain in the eye will be more noticeable—higher power ultrasound is used to crush dense formations. The body needs time to recover.
Eyes and head hurt after cataract
ATTENTION! Before asking a question, we recommend that you read the contents of the “Frequently Asked Questions” section. There is a high probability that you will find the answer to your question there right now, without wasting time waiting for an answer from a consultant doctor.
July 24, 2020
Hello! Couldn't answer; My mother, a year after replacing the lens, that is, now, began to have a severe headache in the area of the operated eye, and there was a constant leak from it. What is the reason and how to treat it? Thanks in advance! Best regards, Sergei -
August 17, 2020
Prayer Oksana Vasilievna answers:
In order to treat, you need to know what to treat. The presence of an artificial lens can only suggest the possibility of diseases associated with it. But, at the same time, it may not have any connection with the disease that has arisen. Therefore, visit an ophthalmologist to determine the cause of these complaints.
June 24, 2010
Good afternoon I am 39 years old. A month ago I had an operation to replace the lens (phacoemulsification), I was diagnosed with cataracts, but my vision was restored from 0.2 to 0.5 and there is no clarity, the pupils in the operated eye are wider. I don’t know what they injected to dilate the pupil. Tell me, How long does the recovery process take, and what needs to be done in order to narrow the pupil? Thanks in advance!
September 30, 2010
Kozina Ekaterina Nikolaevna answers:
It is difficult to answer your question without knowing the causes of cataracts and the specifics of the operation. There is a possibility that the cause of low vision is a wide pupil. Discuss this problem with your doctor. In the normal course of the postoperative period, by one month visual functions are stabilized and the eye is restored.
May 14, 2010
Good afternoon My father was given a referral for surgery to remove a cataract. But now his eye is inflamed (red) and requires surgery. For 2 months, we used all kinds of drops, applied ointments, took pills (including antibiotics). We are not helping. the time for redness in the eye goes away, but after a few days it appears again. They recommended undergoing a full examination by all doctors (cardiologist, ophthalmologist, ENT specialist, dentist, rheumatologist, psychiatrist, neurologist, therapist). Passed. Took tests. No abnormalities were found. Tell me What else can you pay attention to, what tests should you take? Thanks in advance!
June 23, 2010
Oksana Sergeevna Averyanova answers:
You need to check the patency of the lacrimal ducts - this is a simple manipulation. which can easily be carried out by an ophthalmologist. If in old age there is chronic inflammation of the mucous membrane of the eye, then the most classic cause is inflammation of the lacrimal ducts or obstruction of the lacrimal ducts.
November 10, 2014
Hello. I had cataract surgery on my left eye. The first week the eye was apparently recovering from the operation, it saw a little poorly, but after a week, and the next three weeks it saw perfectly. Then the fog and pain appeared. I went to the center where I had the operation, they said that particles from the old lens had appeared and they had gotten under the cornea. They had to be removed, and urgently. Two days later, the same surgeon who performed cataract surgery removed these remnants and prescribed me drops Balarpan, Tobradex, Indocolir, Timalol. It's been 5 days now and the fog on this eye is still there. During the day, sometimes less, sometimes more. Please answer how long this will take. Thank you.
November 12, 2014
Elena Stanislavovna Prokhvachova answers:
Hello, Vyacheslav. A feeling of fog in the operated eye may be due to inflammation, increased intraocular pressure, or impaired corneal transparency. You must be under the supervision of your ophthalmologist and strictly follow the treatment instructions. I wish you recovery!
February 27, 2020
Good afternoon. My father had his lens replaced. He has type 2 diabetes. He takes metformin 850 mg. and glibenclamide 5 mg. Sugar was always normal after taking medications. 5 months have passed since the operation, and throughout these 5 months the sugar level remains at 12-14. Could this be related to the surgery? Thank you
March 02, 2020
Elena Stanislavovna Prokhvachova answers:
Hello Irina. For 1 month after surgery, the level of glycemia can be affected by Dexamethasone drops, which are prescribed in the postoperative period. After 5 months. Increased blood sugar levels are associated with decompensation of diabetes mellitus. Contact your endocrinologist to adjust your treatment. I wish you health!
November 24, 2014
Good afternoon My mother had surgery to replace her lens (chronic cataract). Vision improved very slowly. 1 month has passed. In the vision test table he sees only the top line. The doctor said that the eye was almost in normal condition. I couldn’t answer why my vision doesn’t improve. Please tell me whether and when my vision will be restored or if this is the only effect of the operation.
November 27, 2014
Elena Stanislavovna Prokhvachova answers:
Hello, Elena. Additional examinations of the retina and optic nerve should be performed to determine the cause of low vision after surgery. OCT (optical coherence tomography) of the retina and optic nerve is required, as well as visual field studies (computer perimetry). I wish you health!
May 17, 2011
My grandmother is 90 years old, she was diagnosed with cataracts, and she is insulin dependent. Is it possible to have surgery at this age and how much will it cost?
May 24, 2011
Kozina Ekaterina Nikolaevna answers:
Good afternoon. Age and diabetes (including insulin-dependent) are not a contraindication for performance. lens replacement surgery. Before the operation, you must visit an endocrinologist. The cost depends on the category of complexity, the model of the selected lens and the level of the clinic where the operation is performed.
January 05, 2012
Good evening, tell me what kind of physical activity can I do after lens replacement surgery, like playing football, for example, professionally?
January 24, 2012
The medical consultant of the portal “health-ua.org” answers:
Hello Olga! Much depends on the type of operation, the period elapsed after the operation, and its consequences. During the next 3 postoperative months, professional football is contraindicated. Further recommendations on limiting physical activity will be provided by your attending physician. Take care of your health!
March 19, 2013
Irina Kharintseva asks:
Hello! After surgery to replace the lens, my mother developed corneal edema. She was given injections of solcoseryl and drops were given. The swelling began to subside and she was discharged. But a week passed and the swelling began to progress again. We went for a consultation with a doctor, she was admitted to the hospital again, they injected her with solcoseryl again. Today is the fifth day, but there is no improvement. The eye doesn’t see anything in the morning, and in the evening it’s a little blurry to see anything. The swelling of the cornea should go away 1-2 weeks after the operation, but for her it hasn’t gone away for a month and a half. What should we do? Please tell me.
March 24, 2013
Kozina Ekaterina Nikolaevna answers:
In older people, vision restoration after surgery can take much longer due to age-related inferiority of the corneal structures. In the case of epithelial endothelial dystrophy, treatment is quite complex and requires patience and perseverance from both the doctor and the patient.
November 27, 2014
Hello, Doctor! I am 69 years old. I am being monitored for cataracts. (Ripe). The medical record says: In the history of surgery, myopia (-4.5D) in 1986. DZN from serov. shade, borders merging with myopic staphyloma, angiosclerosis. Dystrophic changes throughout the retina. Is it possible to perform surgery to remove cataracts with this diagnosis? Will I see?
November 30, 2014
Elena Stanislavovna Prokhvachova answers:
Hello, Natalia. Before surgery (if the transparency of the lens allows), a study of the retina and optic nerve should be performed - OCT (optical coherence tomography), this method will help make a prognosis regarding vision after lens replacement. I wish you health!
February 26, 2011
My grandmother is 90 years old, 4-5 years ago she had the lens replaced in one eye. Now she leads a sedentary-lying lifestyle and constantly asks to darken the room, because... she believes that it is better for her eyes. We insist that the eye receives both daylight and the rays of the sun. Tell me, please, how is this correct?
March 03, 2011
Kozina Ekaterina Nikolaevna answers:
Good afternoon. The right thing to do is to do as grandma asks. Although not only the eye, but the whole body needs sun rays. It is impossible to damage the lens with light. But pay attention to whether there are signs of irritation or inflammation of the eye. In this case, a concomitant complaint will be photophobia.
December 13, 2012
Hello! Please tell me, is it possible to change the lens in only one eye? Myopia, astigmatism in both eyes, cataract in the right eye. Is it necessary to change the lens in an eye without a cataract? Or is it possible to replace only the lens with a cataract, and only make a correction on the other eye? Thank you.
December 17, 2012
Elena Stanislavovna Prokhvachova answers:
Hello Tatiana. There is no need to change the lens in an eye without a cataract (at the same time, as it were). If your age is under 40 years and the parameters of the cornea allow it, then you can do laser correction, and if not, you can wear a contact lens on your unoperated eye. I wish you a successful operation!
December 18, 2013
Hello, my dad is 70 years old, he was scheduled for cataract surgery, with the lens replaced with lenses in both eyes, the operation was done with a break of a little more than a week, on the right the lens diameter was 21, on the left 19.5, 20 days passed after the operation, we walked for an appointment with the local ophthalmologist, the right eye sees only 1 line, the left one is better, please tell me whether the visual acuity in the right eye will be restored 7 maybe the lens is not selected correctly? IOP OD = 22 mm Hg. OS = 22.0 mm Hg on on the right, lens + 21.0D, on the left IOP OD = 19.0 mm Hg. OS = 20.0 mm Hg, lens on the left + 19.5 D, floaters are still flying in the right eye, please tell me, will there be an improvement? the disease upon admission on the right eye: age-related cataract of the 3rd degree, on the left eye: age-related cataract of the 3rd degree, associated: pseudophakia. thank you in advance for your answer.
December 19, 2013
Elena Stanislavovna Prokhvachova answers:
Hello Olga. The cause of low vision in the right eye is not necessarily an incorrectly designed intraocular lens. There may be retinal disease or partial atrophy of the optic nerve. Consult an ophthalmologist. I wish you recovery!
June 07, 2020
Nila Alexandrovna asks:
Diagnosis: both eyes - immature cataract, primary open-angle glaucoma of the right eye 1A. primary open angle glaucoma of the left eye 11 A. Exfoliation syndrome in both eyes. Phacoemulsification of cataract with implantation of a flexible IOL was proposed for the left eye. The question is: is it possible to perform such an operation if I am disabled in group 1 with Parkinson's disease? Despite taking the pills, two or three times a day I feel so afraid that my head almost falls off, my blood pressure rises, including inside my skull. Is it possible to ensure complete immobility during the operation and how can shaking affect the eyes after the operation? Or just give up and wait in the wings? How much of that life is left? I'm already 70. Thank you in advance!
June 15, 2020
Prayer Oksana Vasilievna answers:
During the operation, you can ensure immobility; a great danger will exist after the operation, especially the first 2 months. If you can still read, even with glasses, then you don’t have to think about surgery for now. If you can’t read, you can’t take care of yourself, then the risk is justified.
April 02, 2020
Hello, after replacing the lens, at the end of the second week I began to have sharp pains after I drip TOBRADEX drops and the white of my eye turned red (I drop every two hours, as prescribed by the doctors). After two weeks, I will drip DEXAMETHOSONE for the remaining two weeks. Why did the redness and pain?
April 26, 2020
Artem Aleksandrovich Salyukov answers:
Good afternoon. Perhaps this is the body’s reaction to the operation, but if the pain persists and does not decrease every day, you need to contact your surgeon to check whether there is inflammation inside the eye, or is it all just on the surface; further treatment tactics depend on this.
SEE ALSO: What are the consequences of cataracts for the eyes? Can cataracts be cured? Treatment of cataracts after laser correction. Possible complications after cataract surgery. How to get compensation for cataract surgery. Compress on the eyes for cataracts.
Prohibitions during the rehabilitation period
Following the patient's instructions, which can be found in the extract, will help reduce the risk of complications. The restrictions are significant, but reasonable.
- For the first 7 days, it is not recommended to go outside without a bandage.
- Do not use cosmetics for 10 days.
- Physical activity and lifting weights over 3 kg are prohibited for 8 weeks.
- Drinking alcohol and visiting saunas and baths are also not allowed.
Also not worth it:
- massage the eyeball until completely restored;
- be near a fire, oven, fire, fireplace;
- be exposed to cold temperatures (wind, frost);
- watch TV for a long time, read, work on the computer.
This is a period of being gentle with your health in general and your eyes in particular.
Pain in the eyes after laser vision correction
During laser vision correction, the upper flap of the cornea is cut off.
Therefore, the patient may experience pain and discomfort, which are normal during the first few days after surgery.
If the pain persists for a longer period of time, you should immediately consult an ophthalmologist. This may be a symptom of complications that arise as a result of the procedure. The sooner they are eliminated, the higher the possibility of complete restoration of the eyeballs.
Causes
There are physiological and pathological reasons for the development of pain after laser vision correction. In the first case, the symptom quickly goes away as the eyeballs are restored. If the pain is caused by a pathological factor, the doctor needs to identify the root cause using diagnostic tests and prescribe the treatment necessary for the patient.
Pain immediately after surgery
During surgery, a solution is instilled into the patient's eyes, temporarily eliminating all sensation in the eyes. This is an anesthetic. It works within 1-2 hours. After the effect of the drug ends, the patient’s eyes begin to burn, ache, and water. This is a temporary phenomenon, which is caused by the fact that an incision was made on the cornea.
Most often, such pain persists during the first day and goes away in the evening. There are patients with increased eye sensitivity, in which case the pain can persist for up to 5 days. After time it should disappear completely. If this does not happen, the doctor should look for another reason.
Displacement of the corneal flap
To restore vision function, the patient's cornea is cut using a surgical scalpel or laser. In the first case, pain will be inevitable, since this is an outdated technique that leads to severe tissue deformation.
If the doctor used a laser, a thin flap is created, therefore reducing the risk of prolonged pain.
After completion of the surgical intervention, the doctor tells the patient that the eyes should not be scratched or rubbed, since the corneal flap must connect to the structure of the eye at the molecular and cellular level. If the patient violates this rule, the corneal flap is displaced. This condition can occur due to a blow or injury. Additional clinical symptoms appear:
- decreased visual acuity;
- acute pain;
- increased tearfulness.
If the corneal flap has been displaced, the patient is scheduled for additional surgery. The doctor restores the position of the cornea and places it in the required place. A bandage lens is placed on top.
Since displacement of the flap increases the risk of spreading a bacterial infection inside the eyeball, the person is additionally prescribed antibacterial drops and anti-inflammatory drugs.
Dry eye syndrome
The integrity of the eyeball is compromised, as a vacuum must be applied. It keeps the internal structure of the eyes in place.
But when used, the endothelial cells of the cornea, which are responsible for maintaining the tear film on the surface of the eyes, are destroyed. An additional negative effect is the use of a laser for cauterization.
It may cause burns, especially if it has been used longer than required.
Increased dryness of the eyes occurs. This additionally injures the cornea, causing microtraumas and cracks to form on its surface. The patient develops the following clinical symptoms:
- dry eyes;
- pain, pain, during the day and at night;
- redness;
- in complicated cases of hemorrhage on the surface of the cornea;
- increased sensitivity to bright light.
Often pathological symptoms do not appear immediately, but over time. You must consult a doctor immediately. He will prescribe moisturizing drops that will help keep the tear film on the cornea for a long time. During the treatment period, it is recommended to reduce the amount of time spent in front of the TV, tablet, phone, computer.
Keratitis
Complications such as inflammation of the cornea are rare. This is because the surface structure of this area has been damaged. The complication does not develop immediately, but over a period of time, most often after 2-3 months.
The risk group for developing keratitis includes the following categories of patients:
- having scars on the cornea;
- infected with a bacterial infection;
- patients with corneal flap displacement;
- suffering from an allergic reaction to one of the components of medications prescribed after surgery.
The patient develops the following clinical symptoms:
- severe swelling and redness of the cornea;
- formation of scar tissue on the cornea;
- the formation of foreign deposits on the surface structure of the eye, for example, classification, fatty inclusions.
Treatment is carried out using steroid and non-steroidal anti-inflammatory drugs. If they do not help, additional surgery is performed to eliminate the cause of the inflammation.
What to do if eye pain occurs after correction
If eye pain occurs within the first few days after surgery, you do not need to see a doctor. It is recommended to take a pain reliever if a person has increased eye sensitivity.
A new drug for vision treatment was presented at the Skolkovo Innovation Center. The medicine is not commercial and will not be advertised... Read more
If the pain persists after 5 days, it is recommended not to self-medicate. Contact a doctor immediately. He will conduct diagnostic tests that will identify the root cause of the condition. Only after this the doctor will prescribe the necessary therapy.
Poor vision significantly worsens the quality of life and makes it impossible to see the world as it is.
Not to mention the progression of pathologies and complete blindness.
MNTK "Eye Microsurgery" published an article on non-surgical restoration of vision up to 90%, this became possible thanks to...
Read more Was this article helpful?
Rate the material on a five-point scale!
( 1 1.00
Source: //proglazki.ru/lazernaya-korrektsiya/boli-v-glazah-posle-lazernoj-korrektsii-zreniya/
Persistent discomfort after lens replacement
Good afternoon. Woman, 64 years old, lenses replaced. After the operation, there is constant discomfort, daylight irritates, plus the eye pulsates. 2 months have passed since the operation, the discomfort does not go away. What do you advise? What could be the reasons? Doctors assure that everything is fine. Thank you.
Answer from a cataract specialist
Hello. The most common problem of discomfort after surgery is the so-called ocular surface disease. This is a modern term that combines a group of pathologies of an inflammatory and dystrophic nature, leading to disruption of the structure of the tear film, dryness on the surface of the eye or damage to the corneal epithelium. To determine in detail which component of damage to the ocular surface you have, a serious multicomponent examination is necessary. The most common disorder in this group is Dry Eye Syndrome. Therefore, the first, most universal and at the same time safe recommendation would be frequent (at least 4 times a day) constant instillation of tear replacement drugs (for example, Hilokomod 1 drop 4 times a day in both eyes). You can also add antiallergic tablets for 7-10 days (for example, Claritin 1 t once a day), since an allergic reaction is also a component of damage to the ocular surface and causes complaints of discomfort in some cases.
YOU MAY BE INTERESTED in: Treatment of cataracts Semashko Diseases as the cause of cataracts Why the eye waters after cataract surgery Treatment of excimer cataracts Sick leave period after cataract surgery
What to do if your eyes hurt very badly?
Each patient recovers individually from this type of surgical intervention. Therefore, the rehabilitation period and the list of restrictions changes depending on how you feel. In case of severe pain or sudden loss of visual acuity, you should immediately consult an ophthalmologist.
After thirty days, a person can live a full life if there are no complications. Emergency medical intervention is necessary if there is severe swelling, inflammation, or conjunctivitis.
FREE CONSULTATION
Possible complications
As with any surgical intervention, complications may occur after cataract removal. Such unpleasant consequences are explained by the individual characteristics of a particular organism, non-compliance with medical recommendations, or a doctor’s mistake during the operation.
Experts identify several main types of complications that occur most often:
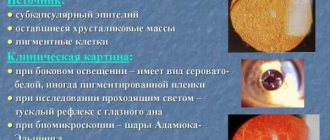
- Secondary cataract (15 – 40%). The problem develops after the patient has undergone extracapsular cataract extraction, ultrasound or laser phacoemulsification. The risk of such a complication is reduced if doctors used the latest technologies in microsurgery. In addition, the material from which the intraocular lens is made is very important. The complication is eliminated by surgical or laser capsulotomy.
- Increased intraocular pressure (1-4%). This symptom is observed when the eyeball is damaged, due to the patient’s hereditary predisposition or due to excessive strain on the eyes.
- Retinal detachment (0.3 – 5.6%). The nature of the damage is determined by how limited the field of vision is. Most often, the problem occurs in patients with diabetes or myopia. In order to correct the situation, another operation will be required.
- Macular edema (1 – 6%). The macular area may swell after extracapsular extraction. The risk of such a complication after cataract removal increases the presence of diabetes and glaucoma.
- Displacement of the iola (1 – 1.4%). The artificial lens may become dislodged after unskilled actions by the ophthalmologist. Even with a slight displacement, the patient urgently needs to be operated on again.
- Hemorrhage in the anterior chamber of the eye (0.6 – 1.5%). This may be due to improper installation of the lens or heavy loads in the postoperative period. The problem is treated either with medication or repeated surgical intervention.
- Iris loss (0.5 -1%). If specialists performed an operation with a small incision, then such a complication may occur. The problem manifests itself as uneven scarring of the wound, astigmatism, swelling and skin ingrowth. The treatment regimen for the complication depends on the time at which it appeared: if the iris falls out 2 weeks after the operation and the wound is not infected, the doctor will simply apply additional stitches. And if the intervention was carried out a long time ago, then the prolapsed iris is excised.
Immediately after surgery, a person may have pain in the eye, eyebrow, or temple. There is no need to be afraid of this, because this is a normal reaction of the body to eye injury. But to eliminate the risk of complications after replacing the lens of the eye, it is worth telling your doctor about the problem that has arisen. Only strict adherence to the doctor's instructions and the use of eye drops will help prevent the unpleasant consequences of surgery.
Therapeutic actions aimed at ridding the patient of complications must be carried out taking into account the cause of the development of the pathology and the degree of its neglect. Some complications resolve on their own and require only minor correction, while others require surgical intervention.
In what cases is scleroplasty necessary and when is it contraindicated?
Eye scleroplasty surgery is prescribed for children and adolescents at the age at which the eye is actively growing - 8-16 years. The intervention is indicated:
- With the progression of myopia, when visual acuity drops by one or more diopters over the course of a year, the initial vision for surgery is -4 - -6 diopters;
- In cases where the eye grows predominantly in length, increasing in the anterior-posterior direction, which provokes visual impairment;
- Myopic women (visual acuity -5 - -6 diopters) planning pregnancy and natural childbirth, since during childbirth you can completely lose vision due to retinal detachment;
Scleroplasty surgery has certain limitations:
- Age - before the 8th birthday it is not advisable due to the high probability of recurrence of myopia with active eye growth;
- The scleral membrane of the eye that is too thin gives a high risk of injury, which is why surgery is considered contraindicated;
- Scar changes do not allow the strengthener to be evenly distributed under the sclera;
- Acute infections (respiratory viral diseases, pneumonia) or chronic diseases during exacerbation (diabetes, pathology of the lungs, heart and blood vessels);
- Inflammatory processes of the eyelids and other elements of the eye (conjunctivitis, uveitis, etc.) serve as a contraindication until they are completely eliminated due to the likelihood of developing endophthalmitis;
- Allergy to local anesthetics or scleral strengthening agents.
If the patient has been ill or is suffering from an acute infection or has an inflammatory process in the eye, then surgery will be scheduled no earlier than one to two weeks after complete recovery. If allergies are present, the possibility of scleroplasty is considered individually after allergological studies.
Causes of cataracts
There are about a hundred eye diseases, but now we will talk about cataracts. It is cataract surgery, the postoperative period, as well as further rehabilitation that are of great interest to patients with visual impairment.
In simple terms, a cataract is a clouding of the lens with visual impairment up to its complete loss.
There are not many reasons for the development of cataracts. The most important and common one is age-related changes in the lens of the eye, leading to a loss of its elasticity and transparency. All organs wear out with age, and the organ of vision is no exception. A secondary role is played by injuries, infections, metabolic disorders, and radiation. There are cases of congenital cataracts.
The main method of treating the disease is surgery, namely removing the affected lens and replacing it with an artificial one.
Drug treatment in the form of eye drops to prevent the disease has not been scientifically proven to be effective. It's hard to believe, but Chinese ophthalmologists have found an amazing way to grow lens tissue from their own stem cells. However, this method of treatment will not soon become widespread.
Few people know that cataract operations were performed a thousand years before our era, but of course these operations cannot be considered successful. It was only in 1752 that the surgeon Jacques Daviel removed the affected lens for the first time. But a full-fledged successful cataract operation was performed already during the Second World War in England.